Trends and ControversiesCheck out the other feature articles in this month's issue: - Myopia: Should We Treat It Like a Disease? |
Major changes to the outpatient and office evaluation and management (E/M) codes are slated to go into effect on January 1, 2021.1 These changes have been long awaited and will certainly reduce the administrative burden on the average practice by making coding your office encounters much easier and straightforward. The changes, made by the American Medical Association CPT Editorial Panel and others, are in response to the Centers for Medicare & Medicaid’s (CMS) request to collapse the E/M codes and reduce the burden of medical record keeping on the physician.
A Look at the Past
The history of determining appropriate reimbursement levels for professional medical services is entrenched in mystery and confusion. For optometry, it began with the profession’s inclusion in the Federal Medicare program on April 1, 1987, which formally classified optometrists as physicians—an important milestone for medical reimbursement protocols in optometry.
The Medicare physician fee schedule is founded on the resource-based relative value system (RBRVS), which stemmed from the Harvard/American Medical Association’s (AMA) RBRVS developed in the late 1980s. The first RBRVS was a Harvard research study initiated by the government because of double-digit annual increases in the cost of medical care in the United States and a perceived opinion that physician fees based on the reasonable/usual/customary methodology were not consistent or equitable. To address this inequity, physician work values and practice expenses for key AMA CPT codes were determined by a survey and validated by physician consensus panels known as the Clinical Practice Expert Panels.
Based on this early RBRVS, the Health Care Finance Administration implemented the new RBRVS for Medicare physician reimbursement in 1992 for all CPT codes, using a crosswalk methodology to fill the gaps where surveyed data was not yet available.
Today’s RBRVS is based on a series of relative value units (RVUs) associated with each CPT code. The three major elements of Medicare’s current system include:
The relative value scale (RVS). This is a list of physician services ranked according to value. The total RVU, in turn, consists of three relative values: physician-work, practice expense and malpractice risk. Values for new and revised procedures in the CPT are included in the updated RVS each year. The malpractice risks are directly assigned by the CMS based on a survey of estimated risk levels by specialty.
The geographic adjustments. The RVS components are factored by a corresponding adjustment for the locality, as geographic adjustments to Medicare payment amounts were introduced in 1995. Three geographic practice cost indices (GPCIs, pronounced “gypsies”) were developed by private researchers, including the Urban Institute, with funding from the CMS.
The conversion factor. Reimbursements are determined for each and every CPT code with a mathematical formula. The formula incorporates all six of the above variables and then uses a conversion factor determined by Congress in the budget-balancing process (Figure 1). This factor is also published each year in the Federal Register.
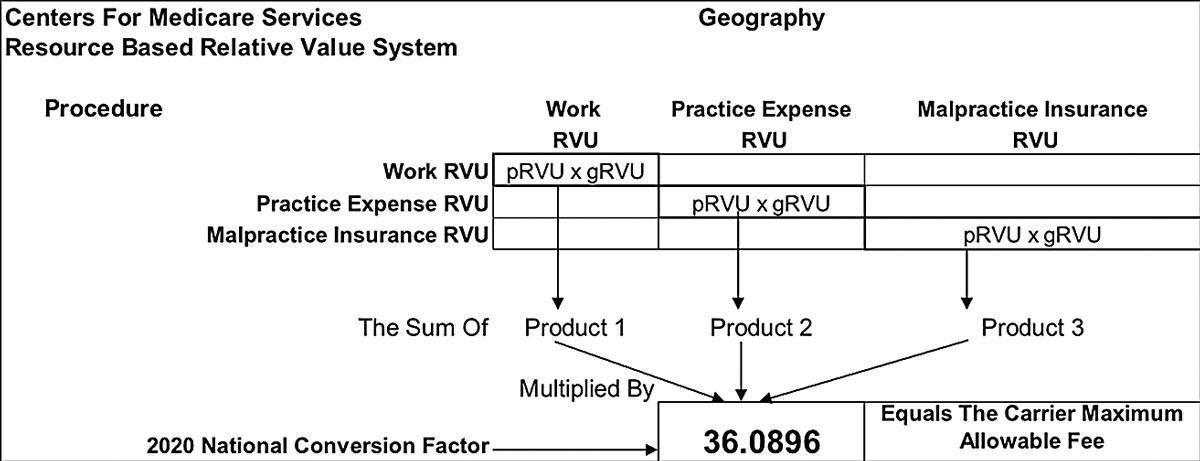 |
| Fig. 1. This is the mathematical formula that determines Medicare reimbursement. Click image to enlarge. |
Changes on the Way
Starting January 1, 2021, performing a history and/or exam will still be medically appropriate for reporting all levels of an E/M service but will no longer play a significant role in the E/M code selection. Instead, providers will select the code based only on the level of medical decision making or total time. These other major changes—for the better—will also make workflow easier to code:
• Deletion of CPT code 99201: Due to low use of the level 1 code for office/other outpatient visit for the evaluation and management of a new patient, this code will be deleted in 2021.
• Although they are necessary factors when reporting an E/M visit, the history and exam elements will no longer be key in the office/outpatient E/M code selection.
• The definition of time associated with E/M levels 99202–99215 is changing from “typical face-to-face time” to “total time spent on the day of the encounter”—a critical distinction. Providers will no longer need to establish how much time was devoted to counseling and coordinating on the day of the encounter. The time values associated with each of the revised office/outpatient E/M codes will reflect the total time spent.
• There are changes to the wording of the medical decision-making elements:
- “Number of diagnoses or management options” is changing to “number and complexity of problems addressed.”
- “Amount and/or complexity of data to be reviewed” is becoming “amount and/or complexity of data to be reviewed and analyzed.”
- “Risk of complications and/or morbidity or mortality” is changing to “risk of complications and/or morbidity or mortality of patient management.”
Practitioners will have a choice on factors to use to determine the E/M code for the encounter: time or medical decision making. That being said, time has a new definition as well, before being applied to the clinical circumstance:1
“When time is used to select the appropriate level for E/M services codes, time is defined by the service descriptors. The E/M services for which these guidelines apply require a face-to-face encounter with the physician or other qualified health care professional. For office or other outpatient services, if the physician’s or other qualified health care professional’s time is spent in the supervision of clinical staff who perform the face-to-face services of the encounter, use 99211.”
For coding purposes, time for office or other outpatient services (99202-99205, 99212-99215) is the total time on the date of the encounter, including both the face-to-face and non-face-to-face time personally spent by the physician and/or other qualified health care professional(s). This also encompasses the time spent in activities that require the physician or other qualified health care professional but does not include time in activities normally performed by clinical staff.
The physician’s or other qualified health care professional’s time includes the following activities, when performed:
- Preparing to see the patient (e.g., review of tests).
- Obtaining and/or reviewing separately obtained history.
- Performing a medically appropriate examination and/or evaluation.
- Counseling and educating the patient/family/caregiver.
- Ordering medications, tests or procedures.
- Referring and communicating with other health care professionals (when not separately reported).
- Documenting clinical information in the health record.
- Independently interpreting results (not separately reported) and communicating results to the patient/family/caregiver.
- Care coordination (not separately reported).
These changes in how the practitioner’s total time is recorded will be helpful in achieving specific levels of coding for an individual encounter.
The new E/M code definitions clearly demonstrate the elimination of the history and exam requirements while emphasizing the time and/or medical decision-making elements by using the wording “medically appropriate history and/or examination.”
Here are the new definitions:1
New Patient (99201 has been deleted; to report, use 99202)
• 99202: Office or other outpatient visit for the evaluation and management of a new patient, which requires a medically appropriate history and/or exam and straightforward medical decision making. When using time for code selection, 15 to 29 minutes of total time is spent on the date of the encounter.
• 99203: Office or other outpatient visit for the evaluation and management of a new patient, which requires a medically appropriate history and/or exam and low level of medical decision making. When using time for code selection, 30 to 44 minutes of total time is spent on the date of the encounter.
• 99204: Office or other outpatient visit for the evaluation and management of a new patient, which requires a medically appropriate history and/or exam and moderate level of medical decision making. When using time for code selection, 45 to 59 minutes of total time is spent on the date of the encounter.
• 99205: Office or other outpatient visit for the evaluation and management of a new patient, which requires a medically appropriate history and/or exam and high level of medical decision making. When using time for code selection, 60 to 74 minutes of total time is spent on the date of the encounter.
Established Patient
• 99211: This code may not require the presence of a physician or other qualified health care professional. Usually, the presenting problem(s) are minimal.
• 99212: Office or other outpatient visit for the evaluation and management of an established patient, which requires a medically appropriate history and/or exam and straightforward medical decision making. When using time for code selection, 10 to 19 minutes of total time is spent on the date of the encounter.
• 99213: Office or other outpatient visit for the evaluation and management of an established patient, which requires a medically appropriate history and/or exam and low level of medical decision making. When using time for code selection, 20 to 29 minutes of total time is spent on the date of the encounter.
• 99214: Office or other outpatient visit for the evaluation and management of an established patient, which requires a medically appropriate history and/or exam and moderate level of medical decision making. When using time for code selection, 30 to 39 minutes of total time is spent on the date of the encounter.
• 99215: Office or other outpatient visit for the evaluation and management of an established patient, which requires a medically appropriate history and/or exam and high level of medical decision making. When using time for code selection, 40 to 54 minutes of total time is spent on the date of the encounter.
Clinicians must ensure their electronic health record (EHR) has the ability to record total time spent while working in a patient’s record, so it will be easy to tally the total time, in minutes, spent on preparation, review, examination and so on.
Medical Decision Making
Whether in the office or for other outpatient services, this code set is defined by three elements (Table 1):1
1. The number and complexity of problem(s) that are addressed during the encounter.
2. The amount and/or complexity of data involved. This includes medical records, tests and other information that must be obtained, ordered, reviewed and analyzed. It also encompasses information obtained from multiple sources or interprofessional communications not separately reported, as well as the interpretation of tests not separately reported. Ordering a test is included in the category of test result(s) and the review of the test result is part of the encounter, not a subsequent encounter. Data is divided into three categories: (1) tests, documents, orders or independent historian(s), where each unique test, order or document is counted to meet a threshold number; (2) independent interpretation of tests; and (3) discussion of management or test interpretation with external physician or other qualified healthcare professional or appropriate source.
3. The risk of complications, morbidity and mortality of patient management decisions made at the visit, as it relates to the patient’s problem(s), diagnostic procedure(s) and treatment(s). This includes the possible management options selected and those considered, but not selected, after shared medical decision making with the patient and/or family. For example, a decision about hospitalization includes consideration of alternative levels of care. Examples may include a psychiatric patient with sufficient support in the outpatient setting or the decision to not hospitalize a patient with advanced dementia with an acute condition that warrants inpatient care, but for whom the goal is palliative treatment.
The new E/M coding system provides practitioners with both flexibility and choice due to the reduced administrative burden of documenting specific levels of history and examination to reach a particular code level.
It is important to prepare your practice for these changes by ensuring that your EHR system allows for appropriate documentation of time and that you are tallying it correctly if you use time for the code determinant. If using medical decision making, spend the time between now and January to become familiar with the new requirements for documentation. They are not all that different from the previous methodologies, but they are just different enough that they warrant your attention.
Change is coming and, for once, it just might make things easier.
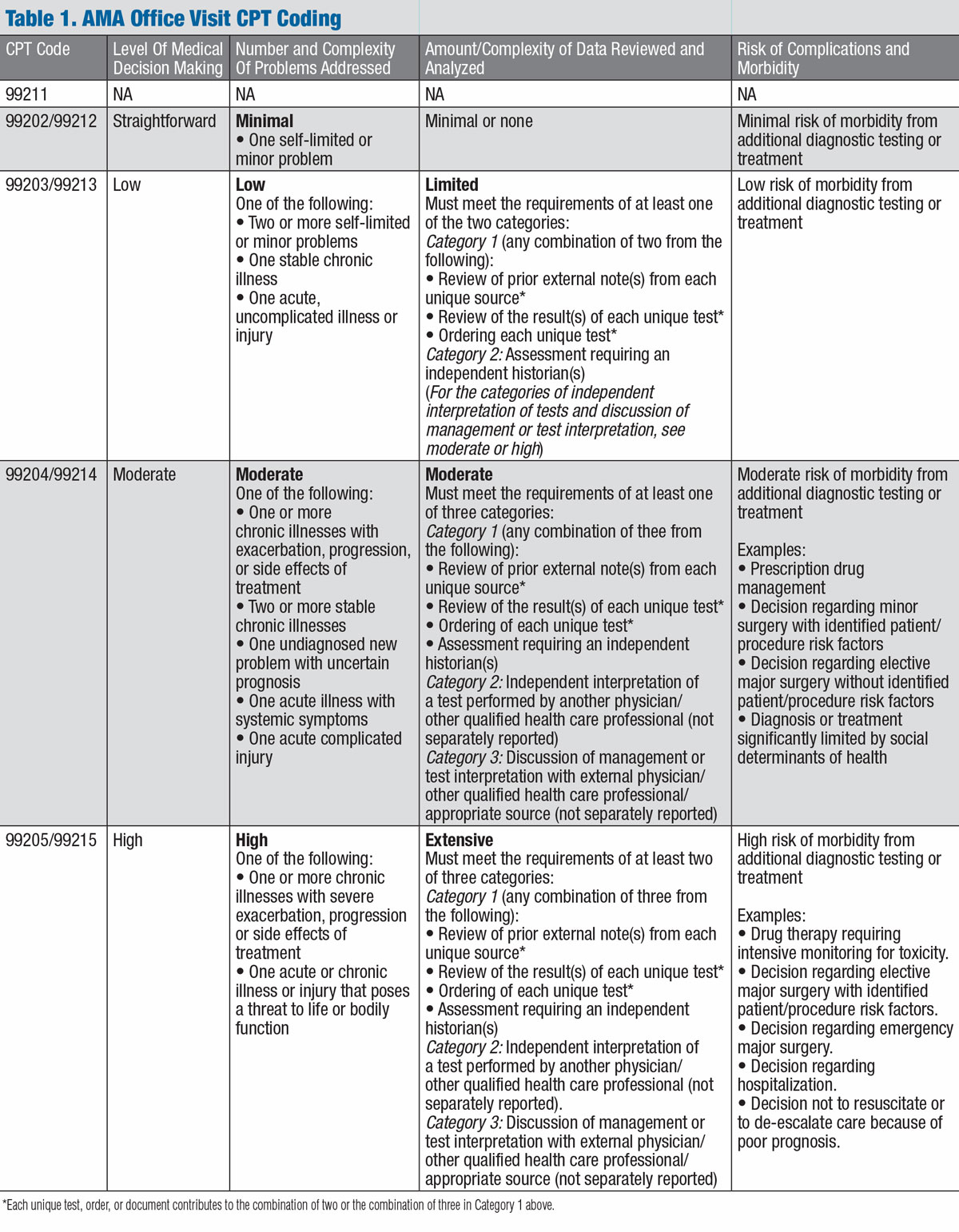 |
| Click table to enlarge. Click here to download a PDF version. |
The information in this article is not intended as a substitute for AMA guidelines. For coding purposes, see the AMA’s original document at www.ama-assn.org/system/files/2019-06/cpt-office-prolonged-svs-code-changes.pdf.1
Dr. Rumpakis is president and CEO of Practice Resource Management, Inc., a firm that provides consulting, appraisal and management services for health care professionals and industry partners. He is also Review of Optometry’s clinical coding editor and authors the monthly Coding Connection column.
| 1. American Medical Association. CPT evaluation and management (E/M) office or other outpatient (99202-99215) and prolonged services (99354, 99355, 99356, 99xxx) code and guideline changes. www.ama-assn.org/system/files/2019-06/cpt-office-prolonged-svs-code-changes.pdf. |

