 |
A 16-year-old white male presented complaining of “shiny gray spots” in his peripheral vision, more in the right eye than the left. He also reported a mild decrease in vision in both eyes, which started about a month earlier. Finally, he noted an increase in floaters in both eyes with no complaints of flashes.
His medical history was unremarkable and he reported good general health. He was not on any medications and denied any previous history of vision problems.
Upon examination, his best-corrected vision was 20/40 in the right eye and 20/30 in the left eye. His pupils, confrontation visual fields and motility were all within normal limits in both eyes.
Anterior segments were also unremarkable with no inflammation noted in the anterior chambers of either eye.
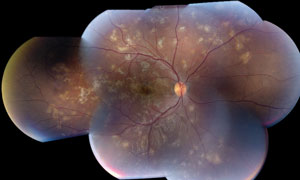
Upon dilation, a mild vitritis was noted in both eyes. The fundus examination revealed multiple creamy white “placoid” lesions along the arcades, in the mid-periphery and periphery of both eyes.
Lesions that were similar in appearance, but more pigmented, were scattered throughout the peripheral retina close to the cream-colored lesions, as seen on fundus autofluorescence images.
 | |
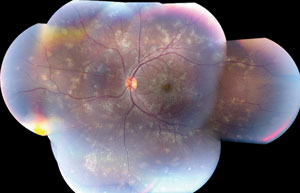 | |
| A 16-year-old patient’s fundus exam revealed multiple creamy white “placoid” lesions along the arcades, in the mid-periphery and periphery of both eyes. |
Take the Retina Quiz
1. Where are the fundus lesions located?
a. RPE and choroid.
b. Vitreous.
c. Outer retinal layers.
d. Photoreceptor layer.
2. How should this patient be treated?
a. Start patient on steroid.
b. Start patient on antivirals.
c. Perform diagnostic vitrectomy.
d. Monitor closely.
3. What is the likely etiology?
a. Infectious.
b. Viral.
c. Autoimmune.
d. Unknown.
4. What’s the likely diagnosis?
a. Acute posterior multifocal placoid pigment epitheliopathy.(AMPPE)
b. Serpiginous chorioretinopathy.
c. Ampiginous chorioretinopathy.
d. Infectious retinitis.
For answers, see below.
Diagnosis
We ordered a systemic medical workup for our patient, which revealed normal complete blood count (CBC), rapid plasma reagin (RPR), and erythrocyte sedimentation rate (ESR). Tests for Lyme disease, Bartonella species and HIV came back negative. His thyroid panel was within normal limits and a chest X-ray was unremarkable.
Our patient returned in two days with a further decrease in vision to 20/60 OD and 20/40 OS. More creamy-white placoid lesions had developed. We started him on oral prednisone 80mg a day. Over three months, the patient had a gradual improvement of vision to 20/30 OD and 20/25 OS and stabilization of retinal lesions. The prednisone was tapered and then discontinued six months after the initial presentation; however, over the next six months, the symptoms returned and new active placoid lesions were noted. The patient was restarted on 40mg a day of prednisone.
Based on the clinical presentation and disease course, our patient has a rare condition called ampiginous chorioretinopathy.
Ampiginous Chorioretinopathy
Ampiginous chorioretinopathy is an inflammatory condition of the retinal pigmented epithelium and the inner choroid. It is similar to acute posterior multifocal placoid pigment epitheliopathy (APMPPE) and serpiginous choroiditis but has distinct “phenotypical” features and clinical course that sets it apart from the other white-dot syndromes.
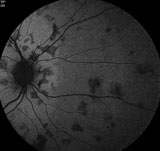 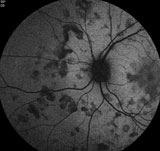 | |
| Fundus autofluorescence shows more lesions scattered througout the peripheral retinas in both eyes. |
Ampiginous chorioretinopathy causes bilateral, yellowish-white placoid lesions with geographic borders in the mid-peripheral and peripheral fundus.1 The location of these lesions is unlike serpiginous choroiditis and APMPPE, in which lesions are located at the posterior pole. The posterior pole may become involved, but this rarely occurs during the initial presentation. The placoid lesions are much smaller (approximately a half disc diameter) compared with APMPPE and serpiginous lesions.2 Ampiginous lesions are recurrent and relentless, like serpiginous, but unlike APMPPE.
Ampiginous chorioretinitis has a male predominance and usually presents in the third or fourth decade of life.2 Common presenting symptoms are sudden, painless loss of vision, new onset floaters, metamorphopsia, or any combination.
Disease Stages
In the acute stage of the disease, fundus exams reveal multiple bilateral yellow to gray colored lesions involving the mid-peripheral and peripheral retina. The macula and posterior pole are spared during the first presentation, but can become involved during recurrent episodes.
There is minimal to 2+ vitritis during the active stage of the disease with occasional subretinal fluid.1 In some cases, subretinal fibrosis and an epiretinal membrane are present.2,3 Anterior segment inflammation may be present with occasional keratic precipitates and episcleritis.1-3
On fluorescein angiography, central hypofluorescence of the active lesion exists with hyperfluorescent margin during the early phase.
The late phase shows hyperfluorescence of the entire lesion. APMPPE lesions, unlike serpiginous and ampiginous chorioretinitis, block fluorescence completely during the early phase of fluorescein angiograpy.1
Active Phase
On fundus autofluorescence, during the active phase of the disease, there is a subtle, diffuse increased autofluorescence of the lesion. A few weeks into the active phase, the lesions reveal a more intense, discrete and coalesced autofluorescence, which decreases over several weeks and eventually shows decreased autofluorescence as the lesions become quiescent.
With our patient, we noted increased autofluorescence of the creamy placoid lesions in both eyes and decreased autofluorescence of the pigmented lesions.4
Relentlessness
Another diagnostic characteristic of ampiginous chorioretinitis is its relentless nature. Various case series show a relapse rate of 35% to 67%.2 Some studies show a relapse rate as high as 81%.2
Relapse can occur as early as six months to as late as five years. During a recurrent phase, new active white placoid lesions often accompany older, healed lesions with chorioretinal atrophy. In severe recurrent cases, more than 50 lesions can be found scattered throughout the fundus.1,2
Treatment
Ampiginous chorioretinopathy is treated with a steroid combined with an immunosuppressive agent. Most reported cases required prolonged treatment with the steroid, or immunosuppressants, or both, to prevent recurrences.1 Subtenon steroid injections have also been used to treat more aggressive and persistent disease.
No reports show improvement of viral prodrome with antiviral therapy.1
The prognosis of ampiginous chorioretinopathy is variable. Permanent vision loss is usually rare unless the fovea is involved.1
Our patient’s final visual acuity was 20/30 OD and 20/25 OS. He has had several recurrences over a period of two years upon discontinuation of the steroids. He was put on a maintenance dose of 15mg of methotraxate weekly and has been quiescent since. He is being followed every six months and follows up with his rheumatologist on a regular basis.
1. Jones B, Jampol L, Yannuzzi L, et al. Relentless placoid chorioretinitis: a new entity or an unusual variant of serpiginouschorioretinitis? Arch Ophthalmol. 2000;118:931–8.
2. Jyotirmay B, Jafferji S, Sudharshan S, et al. Clinical profile, treatment, and visual outcome of ampiginous choroiditis. Ocul Immunol Inflamm. 2010;18:46–51.
3. Mirza, R, Lee, J. Relentless Placoid Chorioretinitis International Ophthalmology Clinics. 2012;52:2377-42.
4. Yeh S, Forooghian F, Wong WT, et al. Fundus autofluorescence imaging of the white dot syndromes. Arch Ophthalmol. 2010;128:46–56.
Retina Quiz Answers:
1) a; 2) a; 3) d; 4) c.

