 |
As use of technology skyrockets, so too does the incidence of near vision complaints. To provide the proper diagnosis and treatment, practitioners must be familiar with the diagnostic possibilities of near work–induced asthenopia. In children, these symptoms are often due to an underlying accommodative or binocular vision disorder. In the more advanced-age population, it can be as simple as presbyopia. However, in the pre-presbyopic population, near vision complaints may be due to accommodative dysfunction.
The ability to accommodate requires a change in the dioptric power of the eye through the increase of lens thickness and curvature. This is achieved through the contraction of the ciliary muscle and relaxation of the lens zonules. These changes are necessary to view objects and images clearly at near.1 Accommodation testing offers the practitioner crucial information about a patient’s focusing capacity.
A Focus on AnatomyThe accommodative pathway is mostly innervated by the parasympathetic system and begins in the midbrain. Stimulation arises via the near triad, which encompasses miosis, convergence and accommodation. There is projection to the Edinger-Westphal nucleus, where the fibers travel to the ciliary ganglion, synapse and, ultimately, continue to the ciliary body and iris sphincter.1
|
Out of Focus
Accommodation decreases with increasing age and the loss of lens elasticity. Other causes of decreased accommodation can include head trauma, midbrain diseases and encephalitis.1 In pre-presbyopes, this is termed accommodative insufficiency. The exact underlying mechanism for accommodative insufficiency in healthy pre-presbyopic subjects is not well understood. However, evidence suggests the presence of an inhibitory accommodative control system regulated by the autonomic nervous system, specifically the sympathetic branch.2
Accommodative dysfunction is a term that encompasses accommodative insufficiency, ill-sustained accommodation, accommodative excess and accommodative infacility (Table 1). Of these subtypes, insufficient accommodation is the most commonly encountered condition, representing 55% to 84% of cases.3-5 It also accounts for the most common cause of asthenopia in children ages eight to 15, highlighting the importance of proper diagnosis and management.6
Those with accommodative insufficiency often present with difficulty performing near tasks. Symptoms can include visual discomfort, eyestrain, fatigue, blurred vision, headache, diplopia and difficulty focusing from one distance to another.2,7,8 These can interfere with a student’s academic progress because avoiding work at near relieves the visual demand.2,7
Accommodative insufficiency is often misdiagnosed in young children and must be differentiated from dyslexia or other binocular vision disorders.9
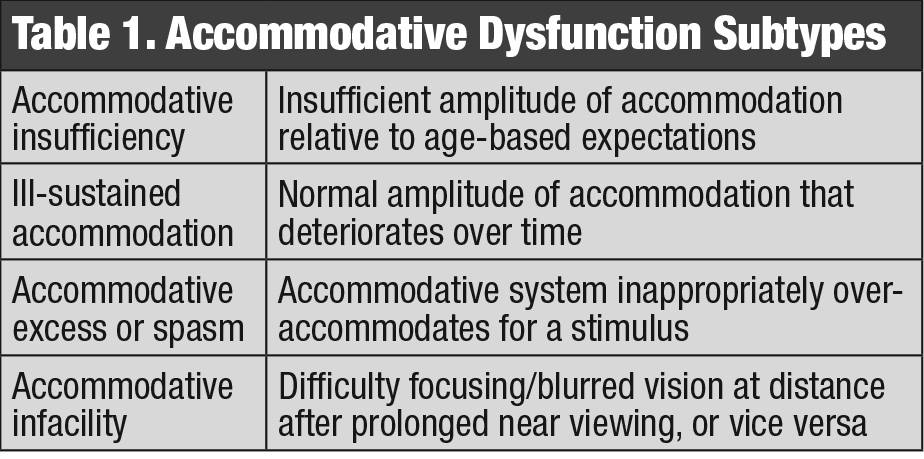 |
| Click table to enlarge. |
Diagnostic Know-how
Clinicians can test accommodative amplitudes using push up to blur monocularly and comparing it with the relative age-based expectations, determined through use of Hofstetter’s formula to calculate the minimum amplitude, as follows:8
15 – (patient age x 0.25)
If the measured value falls two or more diopters below the minimum, the patient has insufficient accommodation.6,10,11 However, research that compared this subjective push up test with more objective methods such as minus lens stimulation or techniques employing a proximal stimulus found the subjective measure substantially overestimates amplitudes in young children.10
Additional diagnostic criteria for accommodative insufficiency include a score of ≤3 cycles per minute (cpm) on binocular accommodative facility (BAF) testing and ≤6cpm in each eye on monocular accommodative facility (MAF), with trouble clearing the -2.00D lens on each test (Table 2). Negative relative accommodation (NRA) is normal, but positive relative accommodation (PRA) values are often less than -1.25D. Finally, monocular estimated method (MEM) testing would reveal a lag of accommodation and is often ≥+0.75D. Many suggest that a combination of two abnormal test values is required to make the diagnosis.6,11 In addition to reduced amplitudes, failing minus on monocular accommodative facility testing is the most associated diagnostic finding with accommodative insufficiency.12
 |
| Vision training activities, such as accommodative flippers, can help to improve accommodation. Photo: Deborah Amster, OD. Click image to enlarge. |
Bring Things Back into Focus
Treatment includes the use of plus lenses for reading as well as in-office or home-based vision therapy to train accommodative facility, with cure rates ranging from 80% to 100% of cases.6,13 The use of plus lenses at near serves as an aid to reduce the blur secondary to the patients accommodative system and obtain a clear retinal image.6
The optimal amount of plus has yet to be determined and may range from patient to patient. Many studies support the use of a +1.00D add power, especially compared with +2.00D lenses. In such studies, +1.00D alleviated symptoms by providing minimal aid with near focus, which allows the accommodative system to relax while still engaging during near tasks. With +2.00D lenses at near, the patient’s accommodative system is not stimulated and the lenses serve as a crutch, minimizing the potential for long-term improvement in accommodative amplitudes.6 Several studies conclude that a statistically significant improvement in the near point of accommodation was measured in patients using +1.00D lenses at near after several weeks of treatment.2,6,14 One study also showed a significant improvement in accommodative amplitudes and reading velocity after eight weeks.2
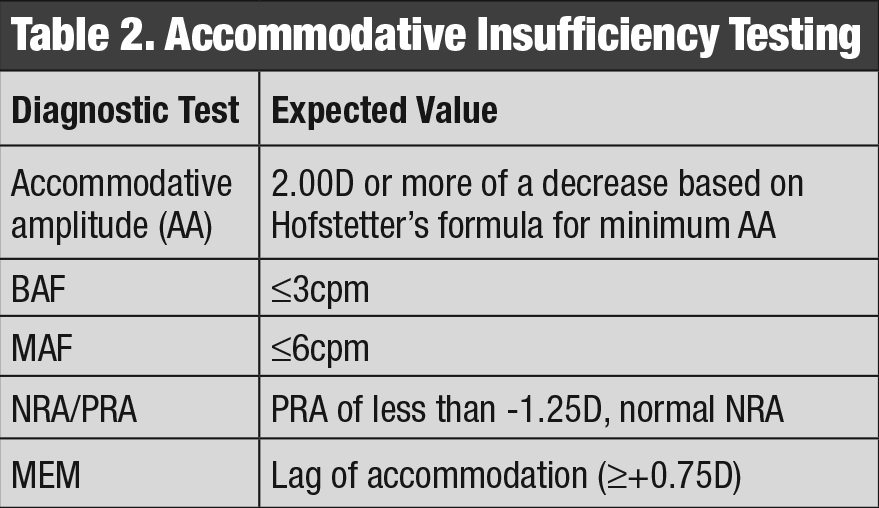 |
| Click table to enlarge. |
Vision therapy for accommodative insufficiency emphasizes the manipulation of blur, disparity and target proximity.7 Tasks are designed to improve accommodative amplitudes and facility, as well as reduce latency. The sequence of office-based vision therapy begins with normalizing and balancing the accommodative responses in each eye, followed by binocular accommodative therapy. Programs consist of weekly 60-minute sessions for 12 weeks, with periods of re-evaluation.15 Often, office-based therapy is reinforced with home-based exercises for 15 minutes per day, with a focus on accommodative rock.15
Overall, while there is a statistically significant improvement in accommodative amplitudes using both plus lenses at near and vision therapy, greater and more long-term improvements are seen with compliance with vision therapy regimens.14
Up to 100% of accommodation insufficiency cases are curable but, if left unmanaged, can deter students from performing well academically. Understanding the various diagnostic elements of accommodation can ensure you catch these cases early and treat appropriately.
| 1. Lee JJ, Baek SH, Kim US. Long-term follow-up of acute isolated accommodation insufficiency. Korean J Ophthalmol. 2013;27(2):116-19. 2. Abdi S, Brautaset R, Rydberg A, Pansell T. The influence of accommodative insufficiency on reading. Clin Exp Optom. 2007;90(1):36-43. 3. Hokoda SC. General binocular dysfunctions in an urban optometry clinic. J Am Optom Assoc. 1985;56(7):560-2. 4. Daum KM. Accommodative dysfunction. Doc Ophthalmol. 1983;55(3):177-98. 5. Borsting E, Rouse MW, Deland PN, et al. Association of symptoms and convergence and accommodative insufficiency in school-age children. Optometry. 2003;74(1):25-34. 6. Wahlberg M, Abdi S, Brautaset R. Treatment of accommodative insufficiency with plus lens reading addition: is +1.00 D better than +2.00 D? Strabismus. 2010;18(2):67-71. 7. Garcia-Munoz A, Carbonell-Bonete S, Cacho-Martinez P. Symptomatology associated with accommodative and binocular vision anomalies. J Optom. 2014;7:178-92. 8. Davis AL, Harvey EM, Twelker JD, et al. convergence insufficiency, accommodative insufficiency, visual symptoms, and astigmatism in Tohono O’odham students. J Opthalmol. 2016:1-7. 9. Boschi A, Bergmans J, Moulaert E, Spiritus M. [Accommodative insufficiency in children]. Bull Soc Ophthalmol. 1990;259:51-60. 10. Anderson HA, Stuebing KK. Subjective versus objective accommodative amplitude: preschool to presbyopia. Optom Vis Sci. 2014;91(11):1290-301. 11. Cacho-Martinez P, García-Muñoz A, Ruiz-Canterob MT. Is there any validity in the diagnostic criteria used for accommodative and nonstrabismic binocular dysfunctions. J Optom. 2014;7(1):2-21. 12. Cacho-Martinez P, García A, Lara F, Seguí MM. Diagnostic signs of accommodative insufficiency. Optom Vis Sci. 2002;79(9):614-20. 13. Russel GE, Wick B. A prospective study of treatment of accommodative insufficiency. Optom Vis Sci. 1993;70(2):131-35. 14. Brautaset R, Wahlberg M, Abdi S, Pansell T. Acommodative insufficiency in children: are exercises better than reading glasses? Strabismus. 2008;16(2):65-9. 15. Scheiman M, Cotter S, Kulp MT, et al. Treatment of accommodative dysfunction in children: results from an random clinical trial. Optom Vis Sci. 2011;88(11):1343-52. |

