44th Annual Contact Lens ReportCheck out the other feature articles in this month's report:- The Building Blocks for a Specialty Contact Lens Practice - Are You Making the Most of the New Soft Lenses? - Don’t Let the Scleral Surge Pass You By |
Currently, 34% of the world is myopic—approximately 42% of the US population and 80% of some Asian populations.1-3 Projections show that more than 50% of the global population will be myopic by 2050 with one billion at risk of subsequent sight-threatening complications.1-3 In addition to rising numbers, the severity of the condition is also increasing.
The pathogenesis of myopia is tied to a combination of environmental and genetic factors. Researchers believe myopia progresses due to peripheral hyperopic defocus along the horizontal meridian.4 This defocus stimulates the growth or elongation of the eye. As axial length increases, the risk for myopic macular degeneration, glaucoma, retinal detachment and cataract increase.1,3,5-7 Highly myopic patients (refractive error >-6.00D, axial length >26mm) have an increased risk for visual impairment, as one-third will experience blindness or low vision.1,4-6
Now more than ever is the time to start implementing myopia control therapies in your practice. Several treatment options exist, ranging from lifestyle changes to corneal reshaping. But one modality, multifocal contact lenses, fits neatly into the optometrist’s toolbox.
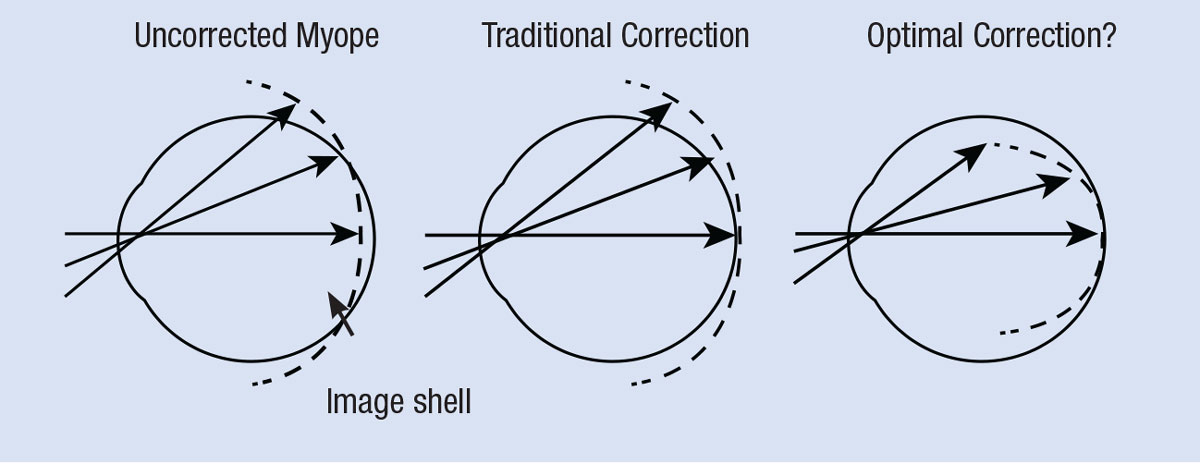 |
Fig. 1. This graphic illustrates myopic and hyperopic defocus, and the possible target for ideal correction. Image: adapted from Smith EL. Optom Vis Sci. 2011;88(9):1029-14. Click image to enlarge. |
Starting Therapy
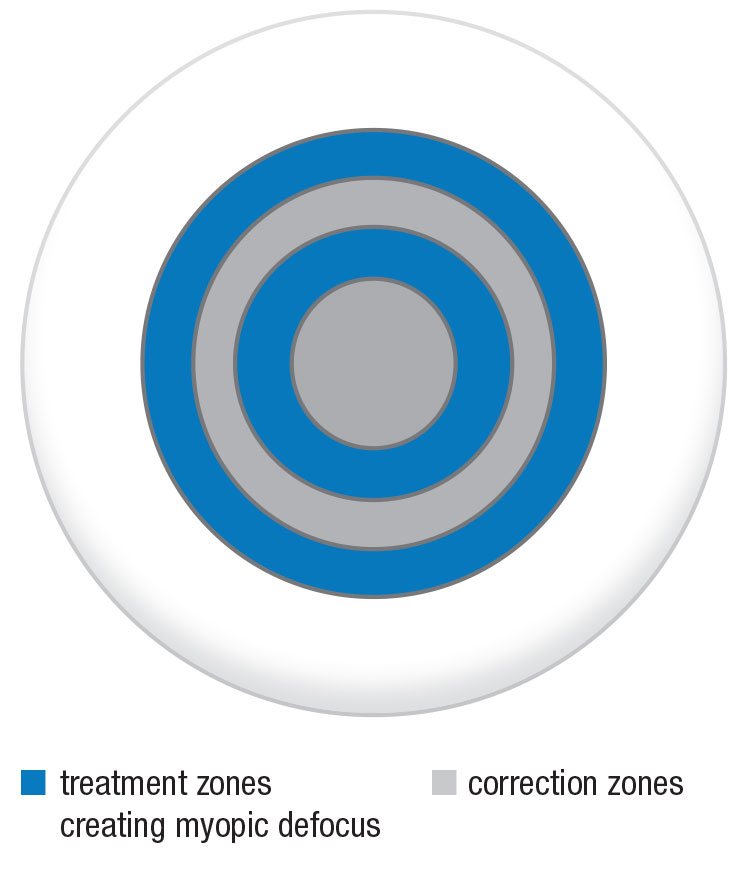 |
Fig. 2. The MiSight lens has two treatment zones, creating a peripheral myopic defocus that causes the image to focus in front of the retina and slow axial elongation. Myopia is corrected in all gaze positions. Image: adapted from CooperVision. Click image to enlarge. |
Cycloplegic spherical equivalent refractive errors are the best predictors for myopia onset.8 For example, research shows six-year-olds with a low degree of hyperopia (+0.75D or less) are at risk for becoming myopic.8 Clinicians should monitor children yearly, as myopia progresses at an increased rate for children between the ages of seven and 12, those who have a higher baseline myopia and patients who have experienced a prior myopia progression of >-0.50D a year.5
Axial elongation has the greatest occurrence the year before the onset of myopia, and once myopia is present, axial length growth continues for an average of five years.5
In addition, myopia shows a higher increase in the winter months. The exact reason for this is unclear but may be due to more schoolwork or less outdoor time.4 It is thought that younger age is inversely related to effectiveness; thus, it is important to intervene when the patient is younger because they tend to progress more aggressively.
When starting myopia control, clinicians should consider the age of onset, current refractive errors, previous myopia control treatments, rate of progression, ethnicity, lifestyle and family history of myopia. We should not recommend myopia control therapies until myopia is visually significant (greater or equal to -0.50DS).5,9,10 Some practitioners choose to wait until they observe progression to initiate myopia therapy.11
The ultimate goal of myopia control is halting axial elongation with a secondary effect of slowing refractive error. Clinically, most practitioners are only able to measure success by monitoring progression of refractive error.
Without intervention, refractive errors, on average, continue to change by 0.50D to 1.00D per year during eye elongation.5 Fortunately, we now have viable treatment options to help slow the progression of myopia, with some showing more success than others (Table 1). Low-dose atropine, orthokeratology and soft multifocal contact lenses are current popular myopia control treatment options. Here, we focus on multifocal contact lenses.
Myopia Control Theories
The mechanism behind myopia control is not well understood, as little is known about the specific signal and pathways that regulate eye growth.4,7,12 When regulating eye growth, the peripheral portion of the eye plays a larger role than the central part of the eye. With traditional contact lenses and glasses, the central retina is in focus, while the peripheral retina experiences a hyperopic defocus (Figure 1). Researchers first suggested hyperopic retinal defocus in the 1970s as a potential mechanism for myopia progression.12,13
Table 1. Myopia Control Research | |
| Under Correction of Myopic Refractive Error | Ineffective |
| Gas-permeable Contact Lenses | Ineffective |
| Outdoor Time | Effective at reducing onset of myopia, ineffective for myopia control |
| Bifocal or Multifocal Spectacles | Statistically significant but clinically not significant4,15 |
| Executive Bifocal | Approximately 39% slowing of refractive error9 *Did not assess axial elongation |
| Orthokeratology | Approximately 45% reduction axial elongation2,4 |
| Bifocal Contact Lenses | 50% to 81.25% effect on refractive error 29% to 55% effect on axial elongation |
| Anti-Muscarinic Agents (0.01% Atropine) | Approximately 59% slowing of refractive error and no effect on axial elongation5,21 |
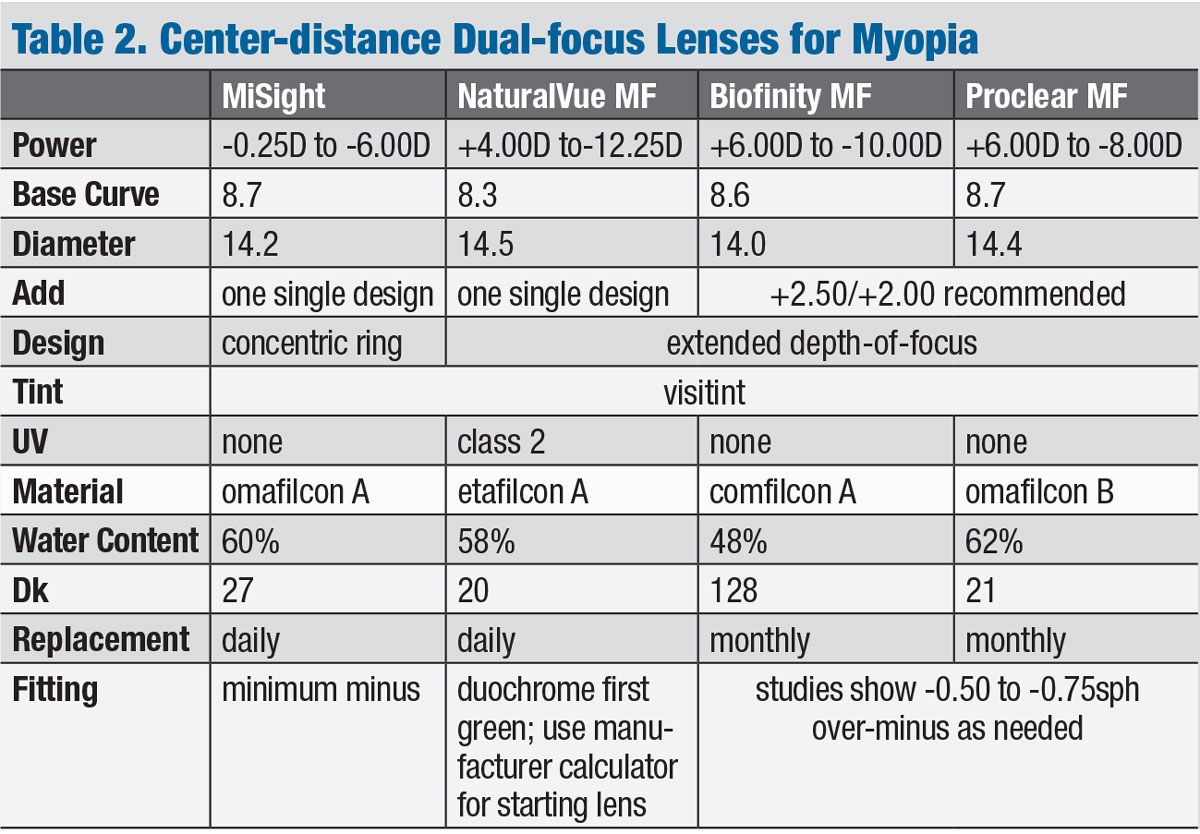
Research shows that axial elongation can be delayed by creating a myopic defocus on the peripheral retina. Orthokeratology and soft multifocal contact lenses are both thought to eliminate the hyperopic defocus and provide a peripheral myopic blur to the retina, which slows eye growth.4,7,12 Little is known regarding the amount of myopic blur needed to effectively slow growth, although current research suggests that increasing the degree and extent of peripheral myopic defocus can improve myopia control outcomes (Table 2).2,5,7
Multifocal Benefits
Historically, multifocal soft contact lenses were designed for correcting presbyopia; however, they have also been used for myopia control and one lens is now FDA approved for myopia management.14 Research suggests the center-distance, or extended depth-of-focus, lenses slow myopia by reducing peripheral hyperopic defocus.14Research suggests this lens modality can slow myopia by approximately 50% to 87.5%.14,15
Factors Influencing Myopia DevelopmentGenetics is just one component of the inheritance pattern of myopia development. For example, a child with two myopic parents is at a higher risk of developing the condition than children whose parents are not myopic.4,14Research shows East Asian children between the ages of 11 and 15 are eight times more likely to be myopic than Caucasians.5 Additionally, time spent outdoors, a close working distance while reading and length of time of reading are environmental factors that may affect the development of the condition.4,5,27 Few preventative measures exist for this condition, although research shows that an average of two hours of outdoor time per day can help reduce the onset of myopia.14 The exact mechanism is unknown, but theories include brightness of light exposure, increased short wavelength and ultraviolet exposure (UV) exposure.5 Once a patient does become myopic, outdoor time does not slow the progression of myopia.7,28,29 Additionally, one study showed a 50% reduction in the number of children progressing into myopia with the use of 0.025% atropine.4 |
The lenses can provide benefits for those who do not want to wear spectacles or use long-term medication. Contact lenses can improve the visual quality of life for myopic children and can improve self-esteem, athletic competence and societal acceptance.15,16 In addition, research shows one lens can reduce lag of accommodation and showed improvement in accommodative amplitude in patients.2
Another advantage of this treatment option is that most optometrists are already familiar with soft multifocal lenses.
Some parents have concerns regarding contact lens use with children. However, with proper education on wear time, modality and lens hygiene, clinicians can help reduce the risk of adverse events such as microbial keratitis.1 A child has more risk of visual impairment from complications of high myopia than from microbial keratitis.1
Daily replacement contact lenses can help to reduce the risk of infections, as one study found this modality had 12.5 times lower risk of inflammatory issues compared with other lens replacement schedules.17 Most of the newer myopia-control contact lenses are daily disposable designs.1
Fitting Tips
The multifocal soft contact lens parameters, such as wear time, add power and pupil size, vary with each patient and may affect the fitting and clinical outcomes of myopia control.13
Wear time is an important factor in slowing myopia progression.18 When evaluating efficacy of a lens, studies usually require a minimum of six hours of wear time per day.13 In daily practice, the suggested wear time for adequate myopia control is seven to eight hours a day.13
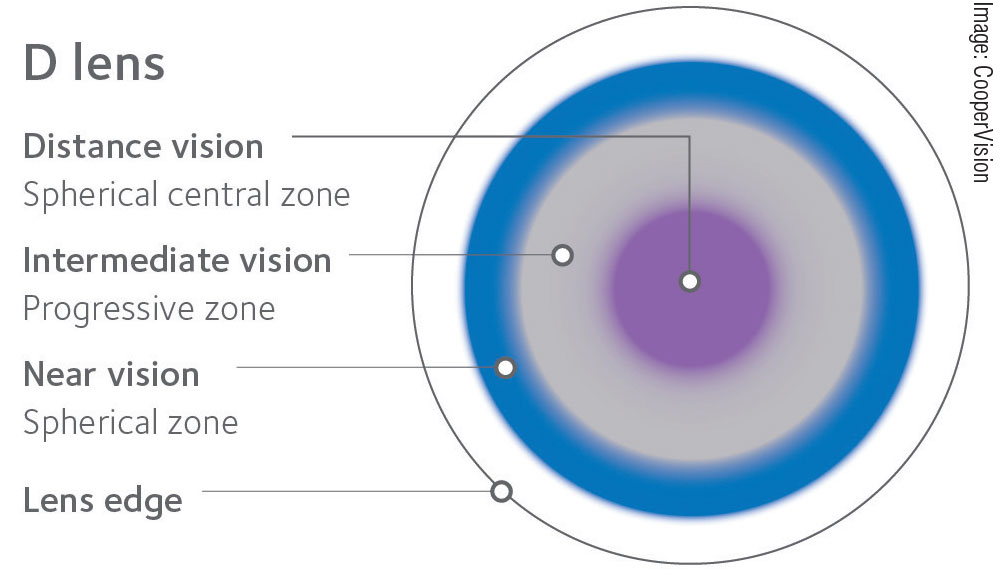 |
Fig. 3. CooperVision’s Proclear and Biofinity both employ a distance-center design that is an effective off-label option for myopia control. Click image to enlarge. |
The add power of a lens is what induces myopic blur and halts eye growth, and research shows improved myopia control with higher add powers.19 The BLINK study is the first trial to evaluate soft multifocal contact lenses (distance-center design) with a low (+1.50D) vs. high (+2.50D) add over a three-year period.20 The results of the BLINK study were not available at the time of publication, but once they are, they may modify the previous recommendation of high add powers for soft multifocal contact lenses to achieve adequate myopia control therapies.5
Some children may have difficulty adapting to multifocal soft contact lenses with high add powers. Practitioners should consider visual acuity, contrast sensitivity and subjective quality of vision when adjusting the prescribed contact lens power.
An increase by -0.25D to -0.75D may improve distance visual acuity and decrease symptoms. If visual function does not improve, clinicians can consider adjusting the add power, if available.15
Pupil size can affect both the refractive power of the multifocal lens and the patient’s visual function and should be considered when fitting these contact lenses.13,21,22 Visual distortions can increase in low lighting and when larger pupil sizes are measured with the light distortion index.21
Multifocal Options
Industry is beginning to offer products designed—or at least effective off-label—for myopia management.
MiSight (CooperVision) is currently the only FDA approved multifocal lens for myopia management, and the company’s online training (https://coopervision.com/practitioner/myopia-management) is required to fit the lens. The lens is indicated for myopia control in patients between the ages of eight and 12 with a myopia correction of -0.75D to -4.00D with ≤0.75D of astigmatism.24
MiSight is a daily disposable lens with a dual focus design (Figure 2). The four-ring structure combines distance correction zones with peripheral treatment zones designed to control the progression rate of myopia.23,24 The lens power is chosen by refracting to the most plus or least minus and calculating the spherical equivalent for any astigmatism.24 If the patient has 1.00D or greater of astigmatism, spectacles over the contact lenses are suggested to minimize ghosting.
 |
| Click table to enlarge. |
Research shows the lens provides a 59% reduction in mean cycloplegic spherical equivalent refractive error and 52% reduction in axial elongation compared with spherical lens wearers in a three-year study.23
NaturalVue multifocal (Visioneering Technologies) is a daily disposable lens used for myopia control in other countries but remains an off-label option in the United States. The lens uses an extended depth-of-focus design to help slow myopia progression. Because of the design, the expectation is that visual acuity is similar to that with spectacles.2 The lens has a universal add power effective up to +3.00D. The manufacturer recommends starting with the best spectacle refraction, using the red/green (duochrome) test for the final binocular sphere power and then using one click into the green (-0.25D) as the starting lens.25
NaturalVue shows an 81.25% halting of myopia progression and 6.25% regression over a six to 25-month period.2 It also shows a 55% reduction in axial length.26 NaturalVue parameters range from +4.00D to -12.25D in 0.25D steps. Patients with up to 1.00D of astigmatism may be successfully fit in these lenses.
CooperVision has two monthly replacement distance-center multifocal lens designs that can be used off label for myopia therapy: Proclear and Biofinity (Figure 3). A two-year study using the Proclear lens showed a 50% reduction in myopia and 29% reduction in axial elongation.4,16 The ongoing BLINK study will provide information regarding the Biofinity multifocal lens for myopia control.
When using the Proclear and Biofinity multifocal designs for myopia control, clinicians should first consider using a +2.50D add power.
There are no current studies regarding multifocal toric contact lenses and the impact of myopia progression. However, if the patient has over 1.00D of astigmatism, the Proclear Toric multifocal, Proclear Toric multifocal XR and Biofinity toric multifocal are available. If clinicians choose to use a custom lens, a smaller optical zone is preferred to affect a larger retinal area and allow greater myopia control.4
Ongoing research will provide more information for future treatments and rebound effects, optimum designs and exact amounts of peripheral myopia defocus needed.
| Other Treatment Options To complement contact lenses, or supplant that option in unsuitable patients, clinicians have other avenues to explore: Atropine is a nonspecific muscarinic receptor antagonist that causes cycloplegia and mydriasis. Muscarinic receptors are found in the human ciliary muscle, retina and sclera.27 The exact mechanism of action is unknown, but data suggests atropine acts on the retina or sclera to inhibit elongation and prevent eye growth.4,5,7,27 Because the patient is dilated, UV light may also increase collagen crosslinking within the sclera, which slows scleral growth.4 Studies suggest 0.01% atropine has similar effects on refractive error compared with higher concentrations.30 Low-dose atropine has fewer reported side effects and less rebounding effects once discontinued compared with higher doses. So far, research shows no signs of retinal damage in patients with long-term atropine use.4 While 0.01% atropine can slow myopia progression by 59%, axial elongation is not affected.4,31 Currently, the World Health Organization recommends limiting atropine treatment to two years.5 Due to the long-term daily use, clinicians should take into account the corneal toxicity from preservatives or prescribe preservative-free atropine.5 Orthokeratology, a long-established treatment for myopia control, shows a reduction in axial length by approximately 45%.4 With this modality, clinicians can only monitor effectiveness due to axial length because the treatment eliminates the refractive error, and once orthokeratology is stopped, a baseline return of the refractive error is variable and usually incomplete.32 Orthokeratology uses a rigid gas-permeable contact lens to reshape the cornea. The lens is worn during the night (>8 hours recommended). Physicians using orthokeratology for myopia control have better outcomes with patients who have moderate myopia (-1.25D to -4.00D) and larger pupils.4 The FDA has refractive error limitations with orthokeratology of 6.00D of myopia and 1.75D of cylinder. Effects on axial length are encouraging and studies show it is a useful myopia control option for those who are already moderately myopic.7 It is recommended that orthokeratology treatment is maintained until the age of 14, as there may be a greater rebound if discontinued at a younger age.4 Combination treatments may be more effective than stand-alone treatment due to the different mechanisms of action. One study shows a decrease in axial elongation when combining orthokeratology and atropine vs. orthokeratology alone.4 However, limited research exists on combining therapies, and if initiated, clinicians should have guarded expectations.15 Advances in the pipeline may soon help prevent and control myopia. With new designs of orthokeratology, contact lenses and novel spectacle lenses, the future is exciting for myopia management. Newer research has focused on Defocus Incorporated Multiple Segments (DIMS) lenses and has shown decrease in axial length by 60% and slowed refractive error progression by 59%.33 These lenses are currently marketed outside the United States. Additionally, there are other novel spectacle lenses being investigated that affect peripheral contrast but will have no effect on central vision.34 |
Follow Up and Discontinuation
Once clinicians successfully initiate treatment, regardless of the approach, they should evaluate the patient at least every six months to ensure treatment safety and efficacy.
Soft multifocal contact lenses can be continued as long as no ocular health issues arise. Most studies evaluate one to five years of treatment, so long-term effectiveness remains unknown. In addition, questions remain regarding the mechanism of action and if any rebounding effect occurs with soft multifocal lenses.4,13
When deciding when to discontinue myopia control treatments, clinicians should note that every additional year of education is associated with an increase refractive error of -0.27D.5 One study of post-university graduates who were in front of computers for an extended period of time found they experienced a 10% myopia progression.4
The COMET study showed peak myopia deceleration was 11.95 years of age.10 Further research suggests the average age of myopia stabilization is between the ages of 15 and 16; however, a large majority of myopes will continue to progress into their 20s.5,10
Knowing the estimated age of progression and stabilization, while also closely monitoring the patient’s refractive status, can help clinicians determine when to discontinue myopia control treatment. Once treatment is discontinued, continue close monitoring of the refractive error to ensure that there is no progression.
Multifocal soft contact lenses are one of the best ways to control myopia. However, only a small percentage of practitioners are fitting the lenses for this condition. An international survey indicated only 6.8% of contact lens fits in 2018 were for myopia control, albeit this is up from 0.2% in 2011.9 Of those, only 47.9% were with soft lenses.9
Hopefully, myopia fittings will continue to increase with a better understanding of the advantages of soft multifocal contact lenses to reduce myopia rather than leaving patients at a greater risk of future myopic pathologies.
Dr. Tison is an assistant professor at the University of Louisville Department of Ophthalmology and Visual Sciences. She also sees patients at the Robley Rex VAMC. She is residency-trained in pediatrics and vision therapy.
Dr. Parker has more than 32 years of experience fitting specialty contact lenses in private practice, where she continues to be a consultative research optometrist. She recently joined the Robley Rex VAMC, where she is starting the Contact Lens service.
1. Gifford KL. Childhood and lifetime risk comparison of myopia control with contact lenses. Cont Lens Ant Eye. 2020;43(1):26-32. 2. Cooper J, O’connor B, Watanabe R, et al. Case series analysis of myopic progression control with a unique extended depth of focus multifocal contact lens. Eye Cont Lens. 2018;44(5):e16-e24. 3. Holden BA, Fricke TR, Wilson DA, et al. Global prevalence of myopia and high myopia and temporal trends from 2000 through 2050. Ophthalmology. 2016;123(5):1036-42. 4. Cooper J, Tkatchenko AV. A review of current concepts of the etiology and treatment of myopia. Eye Cont Lens. 2018;44(4):231-47. 5. Gifford KL, Richdale K, Kang P, et al. IMI – clinical management guidelines report. Invest Ophthalmol Vis Sci. 2019;60(3):M184-M203. 6. Verhoeven VJ, Wong KT, Buitendijk GH, et al. visual consequences of refractive errors in the general population. Ophthalmology. 2015;122(1):101-9. 7. Walline JJ. Myopia control. Eye Cont Lens. 2016;42(1):3-8. 8. Zadnik K, Sinnott LT, Cotter SA, et al. Prediction of juvenile-onset myopia. JAMA Ophthalmol. 2015;133(6):683-89. 9. Efron N, Morgan PB, Woods CA, et al. International survey of contact lens fitting for myopia control in children. Cont Lens Ant Eye. 2020;43(1):4-8. 10. Myopia Stabilization and Associated Factors Among Participants in the Correction of Myopia Evaluation Trial (COMET). Invest Ophthalmol Vis Sci. 2013;54(13):7871-84. 11. Wolffsohn JS, Calossi A, Cho P, et al. Global trends in myopia management attitudes and strategies in clinical practice - 2019 Update. Cont Lens Ant Eye. 2020;43(1):9-17. 12. Sankaridurg P. Contact lenses to slow progression of myopia. Clin Exper Optom. 2017;100(5):432-37. 13. Zhu Q, Liu Y, Tighe S, et al. Retardation of myopia progression by multifocal soft contact lenses. Internat J Med Sci. 2019;16(2):198-202. 14. Pucker A. Myopia control: decisions and discussions. Rev Optom. 2020;157(1):28-33. 15. Tyler J, Wagner H. Myopia treatments: how to choose and when to use? Rev Optom. 2019;156(1):46-53. 16. Sha J, Tilia D, Diec J, et al. Visual performance of myopia control soft contact lenses in non-presbyopic myopes. Clin Optom. 2018;10:75-86. 17. Chalmers RL, Keay L, McNally J, Kern J. Multicenter case-control study of the role of lens materials and care products on the development of corneal infiltrates. Optom Vis Sci. 2012;89(3):316-25. 18. Lam CSY, Tang WC, Tse DY, et al. Defocus incorporated soft contact (disc) lens slows myopia progression in Hong Kong Chinese schoolchildren: a 2-year randomized clinical trial. Br J Ophthalmol. 2013;98(1):40-45. 19. Plainis S, Atchison DA, Charman WN. Power profiles of multifocal contact lenses and their interpretation. Optom Vis Sci. 2013;90(10):1066-77. 20. Walline JJ, Gaume Giannoni A, BLINK Study Group, et al. A randomized trial of soft multifocal contact lenses for myopia control: baseline data and methods. Optom Vis Sci. 2017;94(9):856-66. 21. De Leon M. Multifocal optics explored. RCCL. 2020:18-21. 22. Wagner S, Conrad F, Bakaraju RC, et al. Power profiles of single vision and multifocal soft contact lenses. Cont Lens Ant Eye. 2015;38(1):2-14. 23. Chamberlain P, Peixoto-de-Matos SC, Logan NS, et al. A 3-year randomized clinical trial of misight lenses for myopia control. Optom Vis Sci. 2019;96(8):556-67. 24. CooperVision. MiSight 1 day. coopervision.com/practitioner/our-products/misight-1-day/misight-1-day. Accessed June 22, 2020. 25. Visioneering Technologies. Fitting guidelines and vision enhancement guide. vtivision.com/wp-content/uploads/2020/05/FittingGuidesUpdated.pdf. Accessed June 22, 2020. 26. Aller T. Poster: myopia management with NaturalVue (etafilcon A) multifocal 1 day contact lenses: continuing evidence from clinical practice. BCLA Clinical Conference; Manchester, England, 2019. 27. WSPOS Myopia Consensus Statement. World Society of Pediatric Ophthalmology and Strabismus. 2019. www.wspos.org/wspos-myopia-consensus-statement. Accessed June 22, 2020. 28. Jones-Jordan LA, Sinnott LT, Cotter SA, et al. Time outdoors, visual activity, and myopia progression in juvenile-onset myopes. Invest Ophthalmol Vis Sci. 2012;53(11):7169-75. 29. Xiong S, Sankaridurg P, Naduvilath T, et al. Time spent in outdoor activities in relation to myopia prevention and control: a meta-analysis and systematic review. Acta Ophthalmologica. 2017;95(6):551-66. 30. Gong Q, Janowski M, Luo M. Efficacy and adverse effects of atropine in childhood myopia. JAMA Ophthalmol. 2017;135(6):624-30. 31. Bullimore MA, Berntsen DA. Low-dose atropine for myopia control. JAMA Ophthalmol. 2018;136(3):303. 32. Walline JJ. Myopia control evidence. Cont Lens Spectrum. 2020;35:18-23. 33. Lam CSY, Tang EC, Tse DY, et al. Defocus Incorporated Multiple Segments (DIMS) spectacle lenses slow myopia progression: a 2-year randomized clinical trial. Br J Ophthalmol. 2020;104:363-68. 34. Rappon J, Woods J, Jones D, Jones LW. Tolerability of novel myopia control spectacle designs. Invest Ophthalmol Vis Sci. 2019;60(9):5845-45. |

