 |
Q:
My associate contracted a bad adenoviral infection from a patient last week. He’s into the second week with multiple subepithelial infiltrates (SEIs) over the visual axis and is symptomatic with blur and discomfort. He also has a conjunctival membrane. How might we have avoided this response and, now that he has it, what treatment do you recommend?
A:
“The somewhat flippant answer,” says Daniel G. Fuller, OD, of Southern College of Optometry, “is by practicing safety precautions and appropriate infection control.” Aaron Bronner, OD, of Pacific Cataract and Laser Institute agrees, stating that, “clean examination, proper hand washing and disinfection protocol are the keystones for preventing clinic-based transmission.”
An Ounce of Prevention
When examining a patient suspicious for epidemic keratoconjunctivitis (EKC), “gloving up and using a cotton-tipped applicator to manipulate lids rather than ungloved hands is wise,” says Dr. Bronner.
“Adenovirus is a hardy virus and, absent appropriate cleaning of the exam room surfaces, it remains a source of potential infection long after the patient has left the clinic,” he says. In fact, they can survive for up to 28 days on surfaces, fostering easy contamination and spread.1,2
“Using disposable tonometer tips, using bleach in a 1:10 dilution and isolating infected patients from others prevents spread,” Dr. Fuller says.2 Both ammonia and bleach are effective against adenovirus, but “isopropyl alcohol, while a common office disinfectant, is likely ineffective against adenovirus,” Dr. Bronner points out.3 ODs should consider dedicating an exam room for red eyes and disinfect it after each red eye patient.
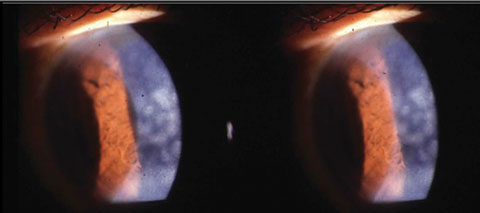 |
| Subepithelial infiltrates from a viral conjunctivitis. Photo: Jeffrey Nyman, OD. |
A Pound of Cure
With EKC, you can treat with supportive therapy (i.e., cool compresses, preservative-free tears and time), or “you could employ one of several off-label approaches in hopes that it may hasten resolution of the infection and reduce late sequelae,” says Dr. Bronner.
Adenoviruses are medium-sized (90nm to 100nm), non-enveloped icosohedral viruses with double-stranded DNA, notes Dr. Fuller.1 “There are more than 50 known serotypes responsible for causing conjunctivitis and upper respiratory, gastrointestinal, cystic and neurological illness, while only a limited number have proven responsible for EKC, pharyngoconjunctival fever and acute hemorrhagic conjunctivitis.1,4 Serotypes 8, 19 and 37 are more prevalent in severe presentations of EKC.”2,4-6
EKC presents in adults as watery discharge, hyperemia, chemosis, follicles and ipsilateral lymphadenopathy. The more severe forms, says Dr. Fuller, “include SEIs (50%) with concomitant decrease in vision, petechial hemorrhages, pseudomembrane formation and symblepharon with true membrane formation.2,5-8 The infection is considered biphasic with symptoms of inflammation appearing seven to 10 days after infection and a usual course of two to three weeks,” he explains.9
There is a dearth of FDA-approved interventions, notes Dr. Fuller.10 “Treatment is supportive for mild forms, and infection control is critical.” Multiple off-label interventions have been tried with limited success, including steroids, antiseptics, antivirals, immunosuppressants and interferon.2
Dr. Bronner credits Mark Maraman, OD, for suggesting hypochlorous acid may be an avenue worth considering. Dr. Bronner explains that a group of 14 cases treated with ultrapure hypochlorous acid (0.008%) QID had rapid clearing of signs and symptoms.11 Of all the off-label treatments for EKC, “hypochlorous acid has the least research,” he notes, “though I feel it may be a compelling option because, as with povidone-iodine (PI), hypochlorous acid is a potent disinfectant and, as with PI, would only theoretically be effective in the extracellular phase. But hypochlorous acid is available by prescription and can be dosed at home.”
Both doctors caution against the use of steroids without weighing the risks against the benefits. Several studies show that routine use of steroids for symptomatic relief should be avoided, as they can prolong the time to achieve viral clearance, Dr. Fuller says.12-15 However, the doctor mentioned in the question is indeed a severe case, and management with steroids seems the best treatment option, especially considering infiltrates are affecting his vision and membranous changes are causing discomfort. In addition, topical ganciclovir may aid in minimizing spread to the other eye and lessen dry eye complaints.
“Since your associate has multiple SEIs, any steroid that effectively penetrates the corneal epithelium is a good way to diminish the lesion,” Dr. Bronner suggests, citing prednisolone acetate 1%, difluprednate and loteprednol etabonate as options. Start steroid treatment “at the first sign of SEIs rather than when multiple lesions are present and the visual axis is heavily involved,” says Dr. Bronner, “to reduce their downstream severity and hasten resolution.”
As a doctor, he should refrain from patient care for 10 to 12 days, and if his eye remains red or there is active tearing, discharge or both, he should stay home. While at home, he should also avoid sharing anything that could transmit the virus, such as towels and washcloths, to avoid intra-familial spread.
|
1. Centers for Disease Control. Adenovirus. Clinical Overview. Available at www.cdc.gov/adenovirus/hcp/clinical-overview.html. 2. Jhanji V, Chan TCY, Li EYM, et al. Adenoviral keratoconjunctivitis. Surv Ophthalmol. 2015;60:435-43. 3. Rutala W, Peacock JE, Gergen MF, et al. Efficacy of hospital germicides against adenovirus 8, a common cause of epidemic keratoconjunctivitis in health care facilities. Antimicrob Agents Chemother. 2006;50:1419-24. 4. Zhang L, Zhao N, Sha J, et al. Virology and epidemiology analyses of global adenovirus-associated conjunctivitis outbreaks, 1953-2013. Epidemiol Infect. 2016;144:1661-72. 5. Tabbara KF, Omar N, Hammouda E, et al. Molecular epidemiology of adenoviral keratoconjunctivitis in Saudi Arabia. Molecualr Vis. 2010;16:2132-6. 6. González-López JJ, Morcillo-Laiz R, Muñoz-Negrete FJ. Queratoconjuntivitis adenovíricas: actualización. Arch Soc Esp Oftalmol. 2013;88:108-15. 7. Chodosh J, Miller D, Stroop WG, Pflugfelder SC. Adenovirus epithelial keratitis. Cornea. 1995;14:167-74. 8. Dawson CR, Hanna L, Togni B. Adenovirus type 8 infections in the United States. IV. Observations on the pathogenesis of lesions in severe eye disease. Arch Ophthalmol. 1972;87:258–68. 9. Kaufman HE. Adenovirus advances: new diagnostic and therapeutic options. Curr Opin Ophthalmol. 2011;22:290-3. 10. Meyer-Rüsenberg B, Loderstädt U, Richard G, et al. Epidemic keratoconjunctivitis: the current situation and recommendations for prevention and treatment. Dtsch Ärzteblatt Int. 2011;108:475-80. 11. Adamson P, Roos H, von Holdt J. Treatment of bacterial and viral conjunctivitis with topical ultrapure stable hypochlorous acid (HCCL): a clinical evaluation and treatment response in 79 cases. Poster presented at ARVO 2015. 12. Romanowski EG, Yates KA, Gordon YJ. Topical corticosteroids of limited potency promote adenovirus replication in the Ad5/NZW rabbit ocular model. Cornea. 2002;21:289-91. 13. Laibson PR, Dhiri S, Oconer J, Ortolan G. Corneal infiltrates in epidemic keratoconjunctivitis. Response to double-blind corticosteroid therapy. Arch Ophthalmol. 1970;84:36-40. 14. Laibson PR, Green WR. Conjunctival membranes in epidemic keratoconjunctivitis. Arch Ophthalmol. 1970;83:100-2. 15. Romanowski EG, Roba LA, Wiley L, et al. The effects of corticosteroids of adenoviral replication. Arch Ophthalmol. 1996;114:581-5. |

