 |
History
A 74-year-old black male reported to the office with a chief complaint of blurry vision and a black spot in his left eye’s field of vision, which he said had existed for many years. He said that he was told “that he had a pit in the back.” He was hoping we could prescribe him some spectacles that would improve his vision.
The patient’s systemic and ocular histories were remarkable for a cerebrovascular accident (stroke) experienced in 2011—with no lasting systemic paralysis and hypertension—for which he was properly medicated with lisinopril and amlodipine. He denied allergies of any kind.
Diagnostic Data
His best-corrected entering visual acuities were 20/20 OD and 20/100 OS at distance and near. His external examination revealed no evidence of afferent pupil defect; however, a left ceco-central superior absolute scotoma was detected using the facial Amsler technique and supported by confrontation fields and Amsler grid follow up. Refraction and pinhole did not improve the acuity.
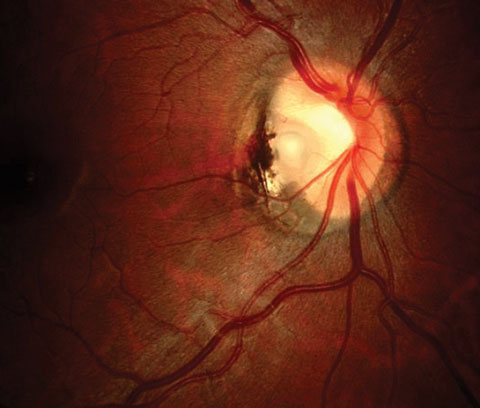
The biomicroscopic examination of the anterior segment was normal with Goldmann applanation pressures measuring 15mm Hg OU. The pertinent dilated fundus findings are demonstrated in the photograph. The periphery was normal.
Your Diagnosis
Does this case require any additional tests? How would you manage this patient? What is your diagnosis? What is the patient’s likely prognosis?
 |
| This 74-year-old patient has suffered from blurry, spotty vision in his left eye for years. Can you say why? |
Discussion
Additional studies included photodocumentation of the posterior poles and nerves for both eyes, optical coherence tomography (OCT) and automated fields.
The diagnosis in this issue is retinomacular atrophy secondary to chronic presumed serous retinal detachment as a sequellae of a congenital optic pit.
Optic disc pits are a rare clinical entity that affects approximately one in 11,000 people.1 Congenital optic pits are small, gray-white, oval depression found at the optic nerve head.1-3 Optic pits are a defect in the cribriform plate where a herniation of the dysplastic retina extends to the subarachnoid space in the optic nerve. This anomaly is surrounded by a layer of collagen-rich tissue.4-9 Optic pits occur due to imperfect closure of the superior edge of the embryonic fissure.3 Patients with congenital optic disc pit sometimes remain asymptomatic, however, 25% to 75% present with visual deterioration in their 30s or 40s after developing macular schisis and neurosensory retinal detachment.1 Men and women are affected equally.5-10
Optic pits are often found on the inferotemporal border of the optic nerve head with 25% to 75% of patients having some form of macular involvement.5-10 Visual loss in patients with optic pits is associated with retinoschisis or serous retinal detachment involving the macula, or both.5-10 Optic disc pits may produce loss in the form of arcuate scotomata or via an enlarged blind spot.6-11
Optic disc pits are categorized into the genera of congenital cavitary anomalies of the optic disc.2 The cavitary anomalies include coloboma, optic pit (and other atypical colobomas), morning glory anomaly and extrapapillary cavitation.2 All of these are associated with maculopathies characterized by schisis-like thickening and serous detachment along with their visual consequences.2 The unifying anatomic theme of these anomalies is the presence of a scleral (or lamina cribrosa) defect permitting anomalous communications between intraocular and extraocular spaces.2 These communications enable the critical pathogenic mechanism responsible for the maculopathy which is dynamic fluctuations in the gradient between intraocular and intracranial pressures. Here, direct movement of fluid (either vitreous humor or cerebrospinal fluid) can be forced into and under the retina.2 Vitreous traction does not seem to play a significant pathogenic role.2
Serous macular detachment is produced by fluid which seeps into the neurosensory retina settling in the outer nuclear layer via the subretinal space.5,10,7,12 The precise pathophysiology remains elusive.6-11 It is proposed that the fluid originates from the vitreous cavity.11 Other possible fluid sources are leaky blood vessels at the base of the pit or in the orbital space surrounding the dura.6-11 The most common theory includes communication between the subarachnoid and subretinal spaces through which cerebrospinal fluid navigates into the subretinal macular region.6-11
Spontaneous closure of the communication is common and attributed to a pressure reduction at the level of the subarachnoid space.6 This, along with firm anatomical adhesions between the neurosensory retina layers and the retina pigment epithelium, eventually stops the fluid movement.6-11
Optical coherence tomography (OCT) images have been used to confirm fluid origins as both cerebrospinal and vitreous.7-12
Optic disc pit diagnosis is based mainly on fundus examination.7-11 OCT can shed light on the morphology of a suspected detachment with a schisis cavity and uncover coexisting outer layer detachment from the retinal pigment epithelium.7-11 OCT can also be a helpful tool to assess the integrity of the inner and outer segment junction line as well as the inner layers of the retina.7-11
Treatment in asymptomatic cases is home monitoring with an Amsler grid and serial dilated examinations with periodic OCT evaluation. Pars Plana Vitrectomy (PPV) is a useful procedure for patients with optic pits for reducing macular thickness.4,8 Vitrectomy for macular detachment due to optic disk pit has good long-term success and usually results in an improvement in visual acuity.5,9 Adjuvant techniques such as internal limiting membrane (ILM) peel and temporal endolaser have not shown success in improving outcomes.9 The long-term follow-up for patients who have received PPV to reduce macular thickness show significant improvement of best corrected visual acuity (BCVA).4,8 When comparing the functional and anatomic outcomes of the combination of PPV and juxtapapillary laser photocoagulation (JLP) with vitrectomy without JLP, PPV with JLP had similar functional and anatomic outcomes.6,10
Patients should be made aware that it can take more than a year and multiple surgeries to achieve foveal reattachment.9 Further, increased baseline central retinal thickness is a poor prognostic sign.5,9
Scleral buckling has also shown success for achieving anatomical and functional outcomes in optic pit maculopathy.7,11 The sclera buckle acts well as a barrier either obstructing the entrance of fluid from the vitreous cavity or blocking the circulation of subarachnoid cerebrospinal fluid into the retina.7,11 Successfully treated patients demonstrated permanent closure of the connection between the optic disk pit and the intraretinal schisis with eventual disappearance of the schisis and subretinal fluid.8,12 In one study the thickness of the macula returned to normal and visual acuity improved in all subjects.8,12
Finally, some studies have demonstrated spontaneous resolution of optic disc pit and associated serous macular detachment.7,11
Since the origin of the fluid that causes the serous retinal detachment can be different for individuals’ different unique treatments must be prescribed depending on the origin.8,12
As an example, laser burns create a scar between the outer retinal tissue and retinal pigment epithelium; this may prevent migration of fluid into the outer retinal space but it does not influence fluid migration into inner retinal layers.8,12 Since multiple fluid pathways exist, vitrectomy and/or laser photocoagulation may be successful in some cases and may fail in others.8,12 Thus, an ideal procedure often combines the relieving of traction and prevention of fluid migration.8,12
The most recent alternative is vitrectomy with or without ILM peeling and gas tamponade with or without endolaser photocoagulation.7,11
This patient presented with blurred vision and a longstanding black spot in their vision, OS. The facial Amsler during confrontational fields revealed a left ceco-central superior absolute scotoma. The Automated visual fields supported this finding. Optic Disc Cube 200x200 and Macular Cube 200x200 was performed. The Macular Cube revealed thinning centrally, inferior and nasally. There was no evidence of active fluid under the macula. There was evidence of retino-macular atrophy from a previous longstanding serous retinal detachment due to the optic pit. The presence of the retino-macular atrophy indicated the fluid that caused the serous retinal detachment occurred some time ago and had long since reslooved. The patient was not referred for treatment and will be monitored every six months.
Dr. Gurwood thanks Dr. Emily W. Weaver contributing this case.
|

