As primary eye care practitioners, we are the first to diagnose and treat a variety of ocular conditions. The role we play becomes even more vital in our youngest patients. Amblyopia, often diagnosed during a patient’s first eye examination, can be managed in a general optometric practice to dramatically improve quality of life in the developing child.
Amblyopia is defined as a decrease in the best-corrected visual acuity of one eye, or less frequently both eyes, in the absence of any structural or pathological changes. Also critical to this definition is the presence of a condition that causes the development of amblyopia, including either a significant anisometropic or isoametropic refractive error; a constant, unilateral strabismus; or some form of deprivation occurring before six years of age.1
 | |
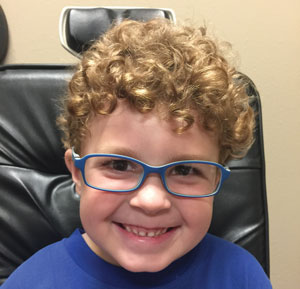
| A thorough exam can uncover the underlying cause of a patient’s amblyopia and help shape the course of treatment. Photo: Kathleen Elliott, OD. |
Why is it important, as a primary care optometrist, to know how to diagnose and treat amblyopia? First, it is not an uncommon condition; the prevalence has been reported to be between 1% and 5% of the population, and it is the most common cause of vision impairment in children and young adults.2-8 Second, it is critical not only to the ocular health but also to the overall well-being of our patients that we correctly diagnose and treat this condition.
It is often difficult to convince patients and parents to invest time and money into treating an amblyopic eye if the patient has good vision in the fellow eye. It is important to educate all parties about what happens if the child loses vision from injury or ocular disease in the non-amblyopic eye. Patients with amblyopia have almost twice the incidence of bilateral visual impairment as those without amblyopia, and their lifetime risk of serious vision loss in both eyes is estimated to be between 1.2% and 3.3%.9,10 A bilateral loss of visual acuity can impact a patient’s ability to drive, maintain employment and function in the world. It is our job, therefore, to not only diagnose and manage this condition, but to also educate our patients on the importance of treating amblyopia.
Causes of Amblyopia
As amblyopia is a rather imprecise term, clinicians must be familiar with the variety of potential etiologies that may be responsible.
• Refractive error. It is important to understand what is considered a ‘significant’ refractive error in the diagnosis of refractive amblyopia. Although there are no definitive refractive values at which amblyopia will absolutely occur, there are guidelines we can use to identify refractive errors that put our patients at risk for the development of refractive amblyopia. This also helps identify patients who do not have a refractive error significant enough, leading us to investigate other causes of decreased best-corrected visual acuity.
Amblyopia can be caused by a significant anisometropia or, less commonly, significant bilateral refractive error. Isoametropic amblyopia is caused by image blur due to a high amount of bilateral ametropia. Refractive errors have to be high enough to prohibit a clear retinal image at any distance. Based on expert consensus outlined in the American Optometric Association’s Clinical Practice Guidelines and the American Academy of Ophthalmology’s Preferred Practice Patterns—supported by the data from the Multi-Ethnic Pediatric Eye Disease Study—significant refractive error causing isoametropic amblyopia can be defined as a minimum of approximately 6D to 8D of myopia, 4D to 5D of hyperopia and 2D to 2.5D of astigmatism in both eyes.11-13 Lower values of ametropia can also result in anisometropic amblyopia—in addition to blur, the difference in refractive error can cause abnormal binocular vision and suppression. Patients with 3D of myopic anisometropia or more, 1.5D to 2D of astigmatic anisometropia and only 1D of hyperopic anisometropia are considered at risk for developing refractive amblyopia.11-13
• Strabismic amblyopia. This is caused by a constant, unilateral strabismus. It is important to note that the size of the deviation is not related to the development of amblyopia, nor is the size of the deviation related to the severity of amblyopia, and even a very small-angle, constant, unilateral strabismus can cause strabismic amblyopia. This highlights the importance of a careful cover test to ensure that the patient has a constant, unilateral deviation.
• Vision deprivation. Finally, amblyopia can be caused by form deprivation. Deprivation amblyopia is caused by a physical obstruction along the line of sight, which prevents a well focused, high contrast image on the retina. This type of amblyopia is relatively rare, found in only about 0.1% of the population, and is associated with conditions such as cataract, hyphema, corneal opacities, vitreous opacities or significant ptosis occurring early in life.14
Diagnosis
When amblyopia is suspected, an initial clinical examination should include visual acuity testing, fixation, refraction, evaluation of ocular alignment and sensory fusion, stereoacuity, accommodation, ocular motility and a thorough ocular health evaluation.11 Acuity testing can be particularly challenging in amblyopic patients: they generally perform poorly on full chart acuity, but exhibit better results on single-line and single-letter acuity testing due to the crowding phenomenon.15 It is important, therefore, to use the same type of visual acuity testing on follow up examination to avoid obtaining an artificially high or low visual acuity measurement.15 It can be difficult to test young children using full-line visual acuity, but using isolated letters may not adequately describe the vision loss seen in amblyopia.
The Amblyopia Treatment Studies use a single HOTV (for children ages three to under seven) or ETDRS (for children ages seven and older) optotype surrounded by crowding bars to evaluate visual acuity, which combines the ease of testing using single letter acuity with the addition of a consistent contour surrounding each letter.16 Obtaining both single-line and single-letter visual acuity measurements give an estimate of the impact of crowding on the decrease in visual acuity in amblyopic patients.
An objective, and if possible a subjective, evaluation of refractive error should be performed during all initial examinations of patients with amblyopia, both before and after cycloplegia. Two drops of cyclopentolate 1% are used in children over the age of one for cycloplegic retinoscopy and refraction. If the patient also needs a dilated fundus evaluation, mydriatic drops should be used in addition to cyclopentolate to give adequate mydriasis for a peripheral retinal examination. Subjective refraction can be challenging in patients with amblyopia, and it is important to have a good objective measure of refractive error, such as retinoscopy. When prescribing for patients with amblyopia, take into consideration the refractive error before and after cycloplegia, the amount of anisometropia after cycloplegia and the patient’s ocular alignment.
A careful evaluation of ocular alignment is necessary to determine the presence or absence of strabismus, and sensory fusion can be evaluated using random dot stereoacuity and Worth 4-Dot testing. An evaluation of fixation using a visuoscope target should also be done in all patients with amblyopia to evaluate for the presence or absence of eccentric fixation. Finally, a thorough ocular health evaluation is critical for proper diagnosis. Any pathological cause of decreased visual acuity must be ruled out prior to making a diagnosis of amblyopia. Patients with amblyogenic conditions such as strabismus or significant refractive error may also concurrently have an ocular disease process occurring, which may contribute to the decrease in visual acuity.
 | |
| Spectacles are the first choice for bilateral refractive amblyopia treatment, considering many patients will improve with spectacle correction alone. Photo: Kathleen Elliott, OD. |
Treating with Spectacles
When deciding whether or not to treat amblyopia, age should not be a factor; amblyopia has been successfully treated in patients seven to 17 years of age.17 In a study of amblyopia treatment in children of this age range, 53% of patients treated with spectacle correction, patching and atropine improved by at least 10 letters after 24 weeks of treatment.17 Although it may be more challenging to treat older patients, all patients—even adults—should be given the option of amblyopia treatment, particularly given the increased relative risk of severe vision loss in both eyes in patients with amblyopia.
The first line of treatment in amblyopia is spectacle correction. Patients should be given spectacles and then monitored regularly, generally every six weeks, for improvement in visual acuity. It is intuitive that patients with bilateral, relatively symmetrical isoametropic amblyopia will have improved visual acuity with spectacle correction alone. In fact, most of these patients will completely resolve their amblyopia with spectacle correction alone within one year.18 These patients are usually easy to treat and can be monitored until their amblyopia resolves, usually within one year, but often sooner.
Anisometropic and strabismic amblyopia are first treated with spectacle correction, but may require additional, more complex treatment such as penalization therapy if vision does not improve with spectacle correction alone. In one study, approximately one-third of children ages three to under seven with anisometropic amblyopia resolved their amblyopia with spectacle correction alone, and over 75% of patients improved two or more lines of visual acuity with spectacle correction alone.19
Surprisingly, another study showed patients with strabismic amblyopia and combined mechanism amblyopia had significant improvement with spectacle correction alone as well; over 75% of patients improved more than two lines of visual acuity, and over 50% improved more than three lines of visual acuity.20 Overall, approximately 25% of patients with strabismus and combined mechanism amblyopia resolved their amblyopia completely with only spectacle correction over 18 weeks of treatment. Amblyopia still improved in approximately one fourth of children ages seven to 17, who are thought to be more difficult to treat than a younger cohort, with optical treatment alone.17
These results highlight the importance of beginning treatment with refraction correction and monitoring. Patients are generally followed every six weeks until the amblyopia resolves, or until their vision plateaus, requiring further treatment.
Advanced Treatment
The next step in amblyopia treatment is penalization of the better-seeing eye. This can be achieved by a variety of methods, the most common being patching or atropine use to blur the sound eye. Patching for two hours per day is recommended for patients with moderate amblyopia (20/80 or better visual acuity), while patching for six hours is recommended for patients with severe amblyopia (20/100 or worse visual acuity).21,22 Studies have found patients with severe amblyopia improved an average of 4.8 lines of visual acuity over four months with six hours of daily patching, and 62% of patients with moderate amblyopia had either an improvement of three lines of visual acuity or a visual acuity of 20/32 or better after four months of daily patching for two hours.21,22
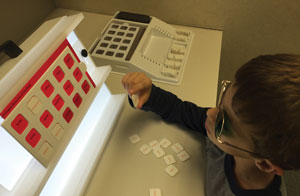 | |
| Advanced amblyopia treatment may include vision therapy, such as anti-suppression therapy using the MFBF matching game. Photo: Marc B. Taub, OD, MS. |
In addition to patching, practitioners may also prescribe at least one hour of near activities per day while patching, such as tasks to improve tracking, fixation and accommodation. One study found no significant difference in visual acuity improvement when comparing near and distance activities during patching; however, the activities in this study were common near tasks and not specifically designed to improve monocular skills.23 Computer activities, such as Amblyopia iNet (Vision Therapy Solutions), can also be used during patching to help improve monocular skills.
Patching compliance can be an issue when treating amblyopia, as patients and parents are often concerned about its social and cosmetic aspects. Studies using an occlusion dose monitor to objectively evaluate compliance have found that patients are compliant with patching therapy approximately 40% to 60% of the time.24,25
The use of atropine for penalization of the better-seeing eye is a good alternative for patients who do not comply with patching, as it has been found to have similar visual outcomes to patching.26 To make compliance even simpler for patients and families, atropine can be used successfully on a daily basis or on weekend days only to treat amblyopia.27 Weekend atropine has been found to be as effective as daily atropine for the treatment of moderate and severe amblyopia in children three to under seven years of age.27,28 Bangerter filters, worn full-time over the sound eye’s spectacle lens to degrade the image, have also been used to successfully treat moderate amblyopia.29 This can also be a good treatment method for patients who are not compliant with patching or atropine penalization.
Another treatment currently under investigation is the use of binocular therapy to treat amblyopia. One approach is to use dichoptic stimuli, in which the amblyopic eye views a high contrast image and the fellow eye views a lower contrast image. This therapy has been implemented using games on an iPad and by having patients view movies with this type of stimulus.33,34 The Pediatric Eye Disease Investigator Group is currently performing a randomized clinical trial comparing the effectiveness of binocular dichoptic iPad games to patching therapy in treating amblyopia.35
Challenges
One of the biggest challenges is the chance of recurrence after completion of treatment. A study of moderate and severe amblyopia treatment found approximately 25% of patients under age seven had a recurrence of amblyopia within the first year of stopping treatment, and children ages seven to 12 had a 7% chance of recurrence (worsening of two lines of visual acuity).30,36 This recurrence is more common in patients with severe amblyopia who went from six hours of patching per day to no patching.30 To help prevent this recurrence, patients should be weaned off patching therapy. Additionally, patients with a history of successfully treated amblyopia need continued close monitoring for a recurrence of amblyopia.
Residual amblyopia is another treatment challenge, considering vision does not improve sufficiently with one treatment for some patients. If the patient is currently patching for two hours, increasing patching to six hours per day may help improve visual acuity and treat residual amblyopia.31 Another option is to switch from patching to atropine or vice-versa to see if acuity improves. Additionally, some practitioners combine therapies, such as using both patching and atropine therapy, although in a study of patients with residual amblyopia, combining patching and atropine did not improve vision more than patients that had patching gradually discontinued.32
Next Step: Comanagement
Depending on the type of amblyopia and the patient’s treatment outcomes, they may require a referral to a specialist. Patients with strabismic amblyopia should see a specialist who can treat strabismus, once their vision has improved with amblyopia treatment. Additionally, if vision in the amblyopic eye is not improved with spectacle correction or patching treatment, additional testing and possible referral is necessary to rule out any underlying pathological condition that may be causing or contributing to the decreased vision.
If vision improvement plateaus and acuity is still not at the level of the sound eye, a referral to an optometrist who specializes in vision therapy may be appropriate. Vision therapy can help improve fixation, oculomotor skills and accuracy of accommodation, all of which may be poorer in patients with amblyopia. Vision therapy can also help treat suppression and improve binocular skills.
Amblyopia is commonly seen in optometric practice, and initially can be managed in a primary care setting. Many patients will improve their visual acuity, some to the point of resolution, with correction only or with correction and optical penalization. Patients whose amblyopia does not resolve with correction and penalization, as well as patients with strabismus, can be referred to a specialist in binocular vision for further treatment. Proper diagnosis and management of amblyopia in a primary care setting is important to providing amblyopic patients the best care and the best possible visual outcomes. n
Dr. Jenewein completed a residency in pediatrics and binocular vision at Nova Southeastern University. She is an assistant professor at Salus University Pennsylvania College of Optometry.
1. Holmes J, Clarke M. Amblyopia. The Lancet. 2006;367: 1343-51.2. Caca I, Cingu A, Sahin A, et al. Amblyopia and refractive errors among school-aged children with low socioeconomic status in southeastern Turkey. Journal of Pediatric Ophthalmology and Strabismus. 2013;50(1):37-43.
3. Arnold R. Amblyopia risk factor prevalence. Journal of Pediatric Ophthalmology and Strabismus. 2013;50(4):213-7.
4. Tarczy-Hornoch K, Cotter S, Borchert M, et al. The Multi-Ethnic Pediatric Eye Disease Study Group. Prevalence and causes of visual impairment in asian and non-Hispanic white preschool children. Ophthalmology. 2013;120(6):1220-6.
5. Chen X, Fu Z, Yu J, et al. Prevalence of amblyopia and strabismus in eastern China: results of screening preschool children aged 36-72 months. British Journal of Ophthalmology. 2015;0:1-5.
6. Pai A, Rose K, Leone J, et al. Amblyopia prevalence and risk factors in Australian preschool children. Ophthalmology. 2012;119(1):138-44.
7. Ying G, Maguire M, Cyert L, et al. Prevalence of vision disorders by racial and ethnic group among children participating in Head Start. Ophthalmology. 2014;121(3):630-6.
8. Tarczy-Hornoch K, Varma R, Cotter S, et al. Prevalence of amblyopia and strabismus in African American and Hispanic children ages 6 to 72 months. Ophthalmology. 2008;115(7).
9. Van Leeuwen R, Eijkemans M, Vingerling J, et al. Risk of bilateral visual impairment in individuals with amblyopia: the Rotterdam Study. British Journal of Ophthalmology. 2007;91:1450-1.
10. Rahi J, Logan S, Timms C, et al. Risks, causes and outcomes of visual impairment after loss of vision in the non-amblyopic eye: A population-based study. The Lancet. 2002;360:597-602.
11. Rouse M, Cooper J, Cotter S, et al. Care of the patient with amblyopia. The American Optometric Association’s Optometric Clinical Practice Guidelines. 2004.
12. Preferred Practice Patterns: Amblyopia. The American Academy of Ophthalmology. 2012.
13. Varma R, Deneen J, Cotter S, et al. The Multi-Ethnic Pediatric Eye Disease Study: design and methods. Ophthalmic Epidemiology. 2006;13:253-62.
14. Friedman D, Repka M, Katz J, et al. Prevalence of amblyopia and strabismus in white and African American children aged 6 through 71 months: The Baltimore Pediatric Eye Disease Study. Ophthalmology. 2009;116(11):2128-34.
15. Morad Y, Werker E, Nemet P. Visual acuity tests using chart, line, and single optotype in healthy and amblyopic children. Journal of the American Academy of Pediatric Ophthalmology and Strabismus. 1999;3(2):94-7.
16. Holmes J, Beck R, Repka M, et al. The amblyopia treatment study visual acuity testing protocol. Archives of Ophthalmology. 2001;119(9):1345-53.
17. Scheiman M, Hertle R, Beck R, et al. Randomized trial of treatment of amblyopia in children aged 7 to 17 years. Archives of Ophthalmology. 2005;123(4):437-47.
18. Wallace D, Chandler D, Beck R, et al. Treatment of bilateral refractive amblyopia in children 3 to <10 years of age. American Journal of Ophthalmology. 2007;144(4):487-96.
19. Cotter S, Edwards A, Wallace D, Beck R. Treatment of anisometropic amblyopia in children with refractive correction. Ophthalmology. 2006;113(6):895-903.
20. Cotter S, Foster N, Holmes J, et al. Optical treatment of strabismic and combined strabismic-anisometropic amblyopia. Ophthalmology. 2012;119(1):150-8.
21. Holmes J, Kraker R, Beck R, et al. A randomized trial of prescribed patching regimens for treatment of severe amblyopia in children. Ophthalmology. 2003;110(11):2075-87.
22. Repka M, Beck R, Holmes J, et al. A randomized trial of patching regimens for treatment of moderate amblyopia in children. Archives of Ophthalmology. 2003;121(5):603-11.
23. Holmes J, Lyon,D, Strauber S. A randomized trial of near versus distance activities while patching for amblyopia in children 3 to <7 years old. Ophthalmology. 2008;115(11):2071-8.
24. Loudon S, Fronius M, Looman C, et al. Predictors and a remedy for noncompliance with amblyopia therapy in children measured with the occlusion dose monitor. Investigative Ophthalmology and Visual Science. 2006;47(10):4393-4400.
25. Wallace M, Stewart C, Moseley M, et al. Compliance with occlusion therapy for childhood amblyopia. Investigative Ophthalmology and Visual Science. 2013;54(9):6158-66.
26. Beck R, Birch E, Cole S, et al. A randomized trial of atropine versus patching for treatment of moderate amblyopia in children. 2002;120(3):268-78.
27. Repka,M, Cotter S, Beck R, et al. A randomized trial of atropine regimens for treatment of moderate amblyopia in children. Ophthalmology. 2004;111(11):2076-85.
28. Repka M, Kraker R, Beck R, et al. Treatment of severe amblyopia with weekend atropine: results from two randomized clinical trials. JAAPOS. 2009;13(3):258-63.
29. Rutstein R, Quinn G, Lazar E, et al. A randomized trial comparing Bangerter filters and patching for the treatment of moderate amblyopia in children. Ophthalmology. 2010;117(5):998-1004.
30. Holmes J, Beck R, Kraker R. Risk of amblyopia recurrence after cessation of treatment. J AAPOS. 2004;8(5):420-8.
31. Wallace D, Lazar E, Holmes J, et al. A randomized trial of increased patching for amblyopia. Ophthalmology. 2013;120(11).
32. Wallace D, Kraker R, Beck R, et al. A randomized trial to evaluate combined patching and atropine for residual amblyopia. Archives of Ophthalmology. 2011;129(7):960-2.
33. Birch E, Li S, Jost R, et al. Binocular iPad treatment for amblyopia in preschool children. Journal of AAPOS. 2015;19(1).
34. Li S, Reynaud A, Hess R, et al. Dichoptic movie viewing treats childhood amblyopia. Journal of AAPOS. 2015;19:401-5.
35. Holmes J, Vivan Manh. ATS 18: Study of binocular computer activities for the treatment of amblyopia.
36. Hertle R, Scheiman M, Beck R, et al. Stability of visual acuity improvement following discontinuation of amblyopia treatment in children 7 to 12 years old. Archives of Ophthalmology. 2007;125(5).

