The prevalence of dry eye disease (DED) has focused the attention of many in eye care on the plethora of new methods of analysis and treatment. Sure, any clinician would love to successfully identify and manage dry eye 100% of the time and would even settle for success most of the time, especially if it doesn’t mean spending a king’s ransom. We may never reach 100% success, but we can maximize our efforts by establishing a specific protocol when confronted with these patients.
Proper dry eye diagnosis can fall into three categories:
- Patients who present with symptoms and signs of dry eye.
- Patients who have symptoms, but lack signs.
- Patients free of symptoms, but show an anomalous sign indicative of dry eye and similar diagnoses.
The trick to correctly diagnosing dry eye is to identify the presence of lid wiper epitheliopathy (LWE), measure tear osmolarity and determine the presence or absence of ocular surface inflammation.
This article provides an in-depth look at how to approach these three steps and get closer to hitting the bull’s eye with your DED patients.
 |
| Dry eye tests need not be exorbitantly costly. The InflammaDry (Rapid Pathogen Screening), is a single-use, noninvasive, disposable test used to detect matrix metalloproteinase-9, a proteolytic enzyme elevated in the tears of dry eye patients. |
Check Under the Lid
The lid wiper is a band of tissue that courses the parallel underside of the lid margin, beneath the eyelashes. Though the lid wiper can be viewed in bright white light, disturbances in the tissue and lid wiper epitheliopathy can best be observed with the aid of vital dyes.1
Surprisingly, until 1965 researchers presumed that much of the internal eyelid was in contact with the globe upon the blink.2 We now know the lid wiper comes into contact with the anterior ocular surface some 3,000 to 15,000 times daily.3 If lubrication is inadequate at the boundary of the tissue interaction, one or both tissues could eventually become compromised. If only the ocular surface is compromised, DED diagnosis is a simple matter of applying diagnostic dyes and using a slit lamp to view the cornea and conjunctiva.
However, when the lid wiper is affected, an OD could easily overlook it, as this part of the anatomy has been routinely ignored. In any state of dry eye disease, the lid wiper suffers greater trauma and epithelial compromise than the ocular surface.3 After all, the lid wiper is in apposition to the globe at all times and, with poor lubrication, is constantly susceptible to mechanical trauma. The ocular surface, in contrast, comes in contact with the lid wiper for only a fraction of a second. Interestingly, a damaged lid wiper could result in symptomatology and be the sole clinical sign. Since it is so easy to overlook, researchers speculate that LWE could explain the clinical phenomenon of patients who experience symptoms but lack other more commonly recognized clinical signs.4
LWE is becoming more noteworthy as its association with dry eye and contact lens discomfort is better understood. LWE can occur with or without contact lens wear and correlates with symptoms for both dry eye and contact lens discomfort.3-5 Researchers believe LWE stems from increased friction between the lid wiper and the ocular surface (or the anterior lens surface in a contact lens wearer) due to inadequate lubrication.1
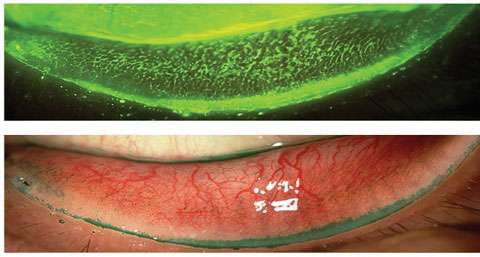
The term epitheliopathy is used to note the uptake of vital dye(s), thereby implying that the tissue is found to have devitalized cells or is in the presence of neighboring cellular apoptosis.7,8,9 Since 2002, researchers have used a combination of fluorescein, rose bengal and lissamine green. Investigators explain that subjects experience different staining patterns with the various dyes and show optimal presentation when applied in pairs (e.g., fluorescein paired with rose bengal or lissamine green).1,5
A recent study proposed an optimal technique for LWE staining and identification by using fluorescein and lissamine green paper strips moistened with saline and subsequently applied to the eye. Specifically, optimal dye effect is observed when two strips of fluorescein (same procedure for lissamine green) are moistened simultaneously with saline and applied to the eye, two times, one minute apart. With this procedure, there is enough dye and enough time for the tissue effect to be observed. The lid margins can be very well inspected three minutes after dye application. This procedure is repeated one minute later and the lid is visualized three minutes later with the benefit of a Kodak Wratten 12 barrier filter (for use with fluorescein dye; transmitting above 495nm).1,10,11 If LWE is present, the lid wiper will stain with either dye. The lid wiper staining is assessed and graded from zero to three in two characteristics: the linear area and width of involvement. The higher of the two characteristics is the resultant grade of LWE.1,3,5
Tear Osmolarity
Dry eye complaints can bewilder an OD given the variability of their presentations. The discovery of tear osmolarity as a biomarker is extremely valuable.
 |
| Positive lissamine green conjunctival staining as seen in the above photo can indicate dry eye, whereas the lid margin staining is indicative of lid wiper epitheliopathy. Photos: Jalaiah Varikooty, Centre for Contact Lens Research, University of Waterloo, Ontario. |
 |
When the tear fluid’s volume is reduced, as is seen with dry eye, the osmolarity increases. A prospective, observational case series of 314 consecutive subjects rated tear osmolarity the single best metric to diagnose and classify DED.12 One study shows tear osmolarity—when compared with traditional tests for dry eye, such as tear break-up time, Schirmer, corneal staining, conjunctival staining and grading of the meibomian glands—is the only test with a greater than 62% sensitivity (72.8%) and specificity (92%).12
Normal tear osmolarity ranges between 275mOsms/L and 307mOsms/L, whereas a reading of 308mOsms/L in one or both eyes or a difference greater than 8mOsm/L between the eyes is noted as abnormal.12,13
An unstable tear film is usually more concentrated and is more variable in dry eye patients when compared with healthy patients.14
There are a few key points in performing this assessment to obtain ideal results. The patient should direct their gaze upwards and away from the tear collection point (generally from the lacrimal lake upon the lower lid at the lateral canthus). The tip of the instrument pen should not touch the sclera. When there is an obvious lacrimal lake, the tip does not need to touch the lid margin. Instead, the fluid resting on the lower lid will be wicked away towards the pen as the device is placed in the tears.
When an inadequate tear sample is suspected, the tester can slide the pen tip along one third of the lower lid margin to collect a greater sample. Once an adequate sample is collected, the unit can quantify the osmolarity.
Eye care professionals should look towards trends and variability when using osmolarity testing. A single test isn’t as valuable as monitoring changes over time. Sporadic changes and variations between the two eyes are far more indicative of a problem than one assessment.
Identifying MMP-9
Dry eye is often accompanied by increased osmolarity of the tear film and inflammation of the ocular surface.15 Hyperosmolarity contributes to the inflammatory cascade, causing distressed epithelial cells and increased levels of cytokines and matrix metalloproteinase-9 (MMP-9), a proteolytic enzyme.16 Research shows MMP-9 is elevated in the tears of dry eye patients.13 These levels correlate well with clinical examination findings. Increased MMP-9 activity increases proportionately with ocular surface dryness and can contribute to damaged corneal epithelial barrier function, increased corneal epithelial desquamation and corneal surface irregularity.17,18
Grading Lid Wiper Epitheliopathy | |
| 1. Grading of horizontal length of fluorescein or lissamine green staining, or both, of the epithelium of the lid wiper.3 | |
| Horizontal Length of Staining | Grade |
| <2mm 2mm to 4mm 5mm to 9mm >10mm | 0 1 2 3 |
| 2. Grading of sagittal height (width) of fluorescein or lissamine green staining of the epithelium of the lid wiper.3 | |
| Sagittal Height (Width) of Staining | Grade |
| <25% 25% to 50% 50% to 75% >75% | 0 1 2 3 |
| 3. For fluorescein or lissamine green grading, or both, the above two tables are averaged to determine an overall score. 4. Grading of lid wiper epitheliopathy is calculated by taking the average score from step 3. The higher of the final fluorescein and the final lissamine green staining is used as the LWE severity grade.3 | |
| Grading Average | LWE Severity Grade |
| 0 0.25 to 1.0 1.25 to 2.0 2.25 to 3.0 | No LWE Grade 1 LWE Grade 2 LWE Grade 3 LWE |
InflammaDry (Rapid Pathogen Screening) is a single-use, noninvasive, disposable test to detect MMP-9. It can detect the presence of inflammation in a simple way in-office and within 10 minutes.
Not all patients respond to anti-inflammatory agents, and it is now understood that not all patients with dry eye have significant ocular surface inflammation.18 Differentiating between patients with and without inflammation using InflammaDry can help direct management in an appropriate direction and can assist in the OD’s expectations. The results of InflammaDry can be used to guide care when symptoms and signs are confounding to the eye care provider. For example, identifying patients with underlying inflammation can guide therapeutic recommendations, including artificial tear replacement, punctal occlusion or anti-inflammatory therapeutics such as a short course of corticosteroids, oral doxycycline, or long-term maintenance treatment with cyclosporine or lifitegrast.13
To perform the InflammaDry test, a technician collects a small tear sample from the palpebral conjunctiva by dabbing the collector’s sampling fleece against the tissue. Adequate saturation is indicated by glistening fleece, turning a pink hue, or both. The device then gets assembled and activated by a buffer solution. After 10 minutes, the device is read in much the same way as a home pregnancy test. A positive test result is noted by a red line on the screen, which is indicative of MMP-9 ≥40ng/mL.13
Dry eye patients challenge optometrists by delivering ambiguous symptoms—sometimes with and sometimes without obvious clinical signs. These three in-office assessments can easily be added to our testing sequence for this patient base. They can help us:
- Examine a region of the eye that previously went undescribed;
- Measure a value that previously would have required extensive and expensive laboratory equipment; and
- Provide direction as to when to tackle ocular inflammation. With a few more steps we can simply and affordably detect and manage most of our dry eye cases.
Dr. Lievens is a professor and chief of staff of The Eye Center at Southern College of Optometry.
|
1. Efron N, Brennan N, Morgan P, Wilson T. Lid wiper epitheliopathy. Progress in Retinal and Eye Research. 2016 July;53:140-74. 2. Ehlers N. On the lid margin, the meibomian glands and their secretions. Acta Ophthalmologica. 1965 March;43(S81):67–75. 3. Korb D, Herman J, Blackie C, et al. Prevalence of lid wiper epitheliopathy in subjects with dry eye signs and symptoms. Cornea. 2010;29(4):377–83. 4. Korb D, Herman J, Greiner J.,et al. Lid wiper epitheliopathy and dry eye symptoms. Eye & Contact Lens. 2005;31(1):2–8. 5. Korb D, Greiner J, Herman J, et al. Lid-wiper epitheliopathy and dry-eye symptoms in contact lens wearers. CLAO. 2002;28(4):211–6. 6. Pult H, Purslow C, Berry M, Murphy P. Clinical tests for successful contact lens wear: relationship and predictive potential. Optometry and Vision Science. 2008;85(10):E924-9. 7. Bandamwar K, Papas E, Garrett Q. Fluorescein staining and physiological state of corneal epithelial cells. Contact Lens and Anterior Eye. 2014;37(3):213–23. 8. Feenstra R, Tseng S. What is actually stained by rose bengal? Archives of Ophthalmology. 1992;110(7):984–93. 9. Machado L, Castro R, Fontes B. Staining patterns in dry eye syndrome: rose bengal versus lissamine green. Cornea. 2009;28(7):732–4. 10. Varikooty J, Lay B, Jones L. Optimization of assessment and grading for lid wiper epitheliopathy. Optometry and Vision Science. 2012;88:E-abstract 125603. 11. Varikooty J, Srinivasan S, Subbaraman L, et al. Variations in observable lid wiper epitheliopathy (LWE) staining patterns in wearers of silicone hydrogel lenses. Contact Lens Anterior Eye. 2015;38:471–6. 12. Lemp M, Bron A, Baudouin C. Tear osmolarity in the diagnosis and management of dry eye disease. American Journal of Ophthalmology. 2011;151(5):792–8. 13. Sambursky R, Davitt W, Friedberg M, Tauber S. Prospective, multicenter, clinical evaluation of point-of-care matrix metalloproteinase-9 test for confirming dry eye disease. Cornea. 2014;33(8):812–8. 14. Sullivan B, Whitmer D, Nichols K, et al. An objective approach to dry eye disease severity. Investigative Opthalmology & Visual Science. 2010;51(12):6125–30. 15. International Dry Eye WorkShop (DEWS). The epidemiology of dry eye disease: report of the epidemiology subcommittee of the International Dry Eye Workshop. The Ocular Surface. 2007;5(2);93–107. 16. Kaufman H. MMP-9 and its role in dry eyes. Advanced Ocular Care. Available at http://eyetubeod.com/2011/10/mmp-9-and-its-role-in-dry-eyes. Accessed November 28, 2016. 17. Chotikavanich S, de Paiva C, Li de Q, et al. Production and activity of matrix metalloproteinase-9 on the ocular surface increase in dysfunctional tear syndrome. IOVS. 2009;50(7);3203–9. 18. Lanza N, McClellan A, Batawi H, et al. Dry eye profiles in patients with a positive elevated surface matrix metalloproteinase 9 point-of-care test versus negative patients. Ocular Surface. 2016;14(2):216–23. |

