 |
Last November a 72-year-old African-American male was referred from his usual OD for glaucoma evaluation. The patient recently presented to his OD with complaints of blurry vision and dry, ‘irritated’ eyes. The patient presented to my office for the initial evaluation along with his 76-year-old sister, who delivered most of his medical history. It was obvious within a few minutes that the patient was somewhat mentally challenged, and, while fully functional, he was apparently not able to live without his sister’s care. It is hard to articulate, but we all have patients who can get by, but need a bit of assistance or guidance to fully succeed.
In any event, he presented with blurry vision for several years, with apparent worsening in the previous few months. He also complained of chronic waxing and waning foreign body sensation in both eyes. Significant in his medical history was a “nervous breakdown” approximately two years earlier, which required hospitalization. As best I could garner, his care involved admittance into the local mental health unit for several weeks. Current medications at that visit included meloxicam qd, propranolol qd, acetylsalicylic acid PRN and acetaminophen PRN. He reported no known allergies to medications.
His entering visual acuities that day were 20/40- OD and 20/60- OS through hyperopic astigmatic and presbyopic correction. Pinhole acuities were 20/40 OD and 20/50 OS. Confrontation fields were constricted peripherally and showed some central defects as well. Amsler testing was difficult to ascertain.
A slit lamp examination of his anterior segments was characterized by moderate SPK present on both corneas, open angles on slit lamp estimation, quiet anterior chambers OU with no evidence of cell nor flare, and mild episcleral injection. The episcleral injection was consistent clinically with the appearance of the SPK, which was located throughout the inferior corneas, consistent with evaporative dry eye.
 |
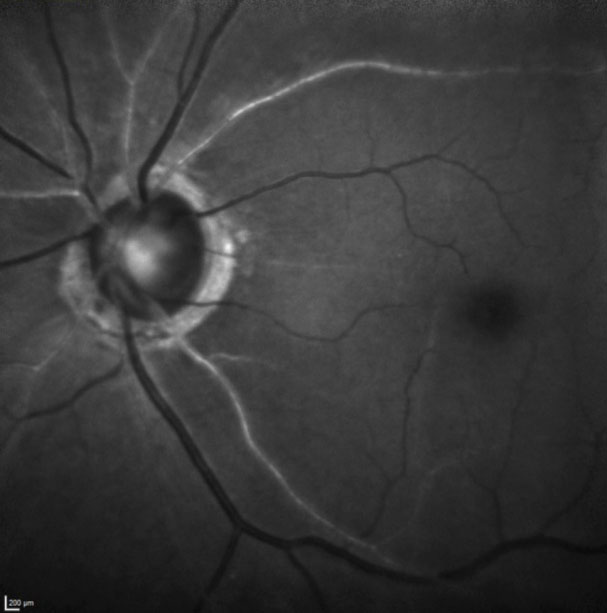
| Note the significantly disseminated arteriolarsclerosis in this multicolor laser composite of the right optic nerve and vasculature. |
Examination
Applanation tensions were 35mm Hg OD, 37mm Hg OS at 2:45pm. Pachymemtry readings were obtained and they showed relatively thin corneas of 505µm OD and 512µm OS.
Through dilated pupils his crystalline lenses were characterized by early nuclear sclerosis bilaterally, as well as cortical spoking off the visual axis. His cataracts were estimated to account for one, and perhaps two, lines of visual acuity decrease. We also noted posterior vitreous detachment.
His cup-to-disc ratios were 0.05x0.07 OD and 0.75x0.85 OS. Both neuroretinal rims were characterized by thinning temporally, especially superotemporally in the right eye and temporally in the left from 2 o’clock to 5 o’clock. Additionally, both remaining neuroretinal rims were slightly pale and mildly atrophic. No disc hemorrhages were present.
Macular evaluations were consistent with RPE mottling and fine drusen. Of clinical significance, his retinal vasculature, in particular his retinal arterial vascular picture, was consistent with marked arteriolarsclerosis OU. The retinal arteries were segmentally sclerosed, with narrowing, and secondarily inducing moderate crossing changes. Blood pressure in the office was 128/80, with a resting pulse of 72. The retinal vascular picture was more consistent with atherosclerotic cardiovascular disease moreso than hypertension. His peripheral retinal evaluations were normal.
 |
| In this green laser image of the left optic nerve and macular vasculature, note the segmental atherosclerotic changes to the retinal vasculature, most readily seen in the superior temporal artery. |
Imaging
Once the patient was dilated and examined, I had my techs obtain optical coherence tomography (OCT) images of the optic nerves as well as multimodal shots of the posterior segments. The OCT demonstrated significant thinning of the neuroretinal rim as well as loss of perioptic retinal nerve fiber layer (RNFL) tissue on all three-diameter circle scans. The multimodal imaging documented the extent and severity of the arteriolarsclerosis present OU.
Given the findings of both open angle glaucoma of moderate-to-severe staging, as well as clinical evidence of an overlying vascular component, the patient was asked to return within the week for threshold field studies, gonioscopy and UBM imaging. While the patient was clearly going to need intervention to reduce his IOP, I chose not to medicate the patient that day as only having one pretreatment IOP reading makes it difficult to assess post treatment efficacy, especially in light of potential IOP fluctuations, which may be significant in a vasculopathic eye such as his. The patient was also scheduled for carotid ultrasonography.
He returned a few days later as requested. At this visit his IOPs by applanation were 34mm Hg OD and OS at 9:55am. Threshold visual field studies demonstrated significant global depression, along with central field loss, and field loss in the classic arcuate area 10-20 from fixation OU. Gonioscopy demonstrated open angles with moderate trabecular pigmentation 360 degrees OU with normal angle anatomy. Ultrasound biomicroscopy (UBM) studies demonstrated no angle abnormalities that would be complicating the management of the glaucoma. At this follow-up visit, carotid studies were pending.
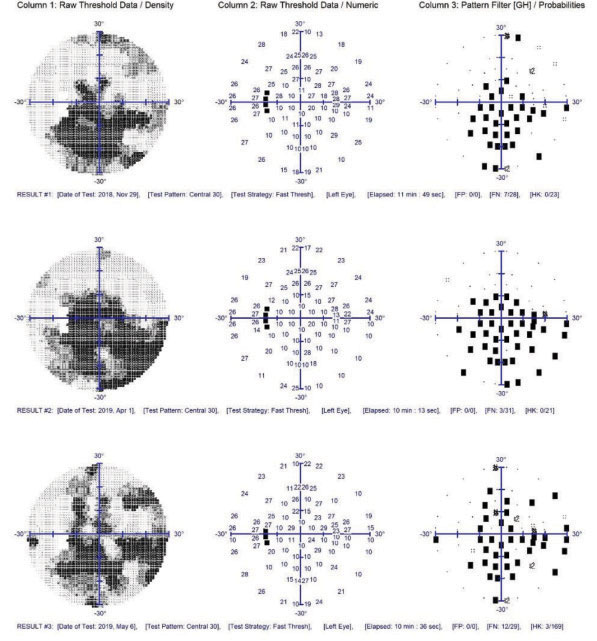 |
| Note the generalized depression and central visual field defects, which are correlated to the vascular insufficiency more so than the glaucomatous damage in these threshold field studies of the patient’s left eye. While the visual fields show no frank progression, the reliability indices and repeatability were not optimum. |
Discussion
This case highlights the classic presentation of an untreated pressure dependent glaucoma patient who also has a vascular component. At this point, the extent of the vasculopathic disease is not yet clear, as the initial workup—including the carotid ultrasonographic results—have not been investigated.
Given that we now have had two separate IOP readings, which show relatively little variation between afternoon and morning readings, it is imperative to begin IOP lowering therapy. As such, the patient received a sample of Vyzulta (latanoprostene bunod ophthalmic solution, Bausch + Lomb) to use QHS OU, and he was scheduled for another follow-up visit in three weeks to assess the efficacy of this medication and to evaluate anterior segment anatomy using OCT imaging and UBM ultrasonography.
Prior to the next follow-up visit, the Doppler image results were sent and they showed bilateral minimally significant plaque at the bifurcations of the common and internal carotid arteries on both sides. The good news is that he has no overt carotid artery disease, but on the other hand, his vascular picture is consistent with atherosclerotic cardiovascular disease; accordingly a discussion was had with his doctor regarding tight lipid control (and re-evaluation of lipids, which haven’t been performed in more than two years) as well as anticoagulation therapy to assist with vascular perfusion to the eye.
The Heart of the Matter
So how did we jump to the discussion of anticoagulant therapy so soon? Quite simply: though his carotid arteries were not demonstrating clinically significant disease, certainly his retinal arteries were. And the common vessel between these two is the ophthalmic artery, which, by clinical presentation of the retinal vasculature, I would have to assume were (as the retinal findings were bilateral) also manifesting atherosclerosis. And therein lies the key to this case.
It has been discussed for many years the role of optic nerve perfusion in the context of glaucoma. Simply put, an eye with a compromised vascular supply, is at increased risk for many ophthalmic conditions, including normal pressure (pressure independent) glaucoma and worsening glaucoma. There are many pieces to the puzzle insofar as ophthalmic perfusion pressure, and there are several proposed formulae for estimating ocular perfusion pressure. In a case such as this, the significant appearance of retinal arteriolar vascular disease would naturally imply ophthalmic artery disease as a comorbid process, and consequently, decreased ocular perfusion. And how is any arterial occlusive disease dealt with? The answer is increasing perfusion, whether that is a carotid endarterectomy in the case of carotid artery disease, or anticoagulant therapy in the case of coronary artery disease. It’s the same disease process, its just that different end organs are affected depending on which vessels are problematic. Of course, any surgical intervention or anticoagulant therapy needs to be evaluated against possible complications, but it is a natural step in increasing perfusion to the eye.
After consulting with the patients primary care provider and subsequent labs, the patient was found to have elevated cholesterol and lipid levels, and the patient was medicated with a statin. He was also anticoagulated with 81mg ASA and 75mg Plavix as the patient’s primary care provider was also concerned about cerebral ischemia.
Since the initiation of Vyzulta QHS OU, the patient’s IOPs have averaged 15mm Hg OD and 17mm Hg OS on three separate visits. Visual fields as shown have remained stable, as have the optic nerve OCTs and physical evaluations of the nerves. The retinal vasculature has remained stable.
The patient is also currently scheduled for an neuroimaging, as part of further investigation of disseminated vascular disease.
This is optometry: caring for glaucoma, mild, moderate and severe. Working in collaboration with internal medicine, this patient can be adequately cared for without involving ophthalmology.

