For patients struggling with limited acuity in spectacles or standard soft contact lenses, a specialty soft or rigid gas permeable lens may make a difference in vision; corneal topography can dramatically aid the evaluation of such patients. This article focuses on the employment of corneal topography relative to ocular irregularities that are present secondary to disease, trauma or surgery.
Mapquest
With the former manual keratometry method, the curvature of the ocular surface was assessed through alignment of two corneal mires (reflections) along the major meridians of the eye (steep and flat). While some corneal irregularities such as poor tear quality or keratoconus could be detected, manual keratometry was limited when compared to today’s automated topography.
Advances in current topographers have established the ability to interpret corneal data via maps that illustrate the amount of change over the corneal surface: various types of maps are classified as refractive, sagittal, tangential or elevation. The refractive map provides insight into the change of refractive power across a patient’s eye, and is a good way to reveal the focusing power of the eye attributable to the cornea, as well as the magnitude of cylinder present in an astigmatic eye.
Refractive maps are useful when estimating values for LASIK refractive surgery or selecting an intraocular lens implant for cataract extraction.
• The sagittal map, also known as an axial map, presumes the change in corneal curvature is relative to a perfect sphere. This normalizes the data and, in turn, results in less accuracy, but is still a good tool to evaluate the course of change across the cornea.
• The tangential map is generated by compiling the instantaneous radius of curvature across each of the given points of the cornea. This property is why tangential maps are innately more accurate for evaluation of contact lens selection for scleral or specialty lens fits.1,2
• The elevation map is typically best to gain an impression of how steep or flat the eye is, and aids in initial lens selection, in particular for scleral or other specialty lenses.
One of the first things to evaluate when looking at a topography image is the elevation map. This provides the “big picture” of the contour of the ocular surface, and quickly identifies what type of surface we are dealing with. This map uses a relative sphere or average sphere to depict the corneal shape. Warm colors represent areas that are elevated above that sphere, and bluer colors represent areas that are lower than a relative sphere.
Another critical, and perhaps most commonly recognized, map is the axial topography, sometimes referred to as a power map. This map is generated from reflections that come off the device’s concentric placido rings; it essentially represents the slope of change as one moves from central to peripheral cornea.
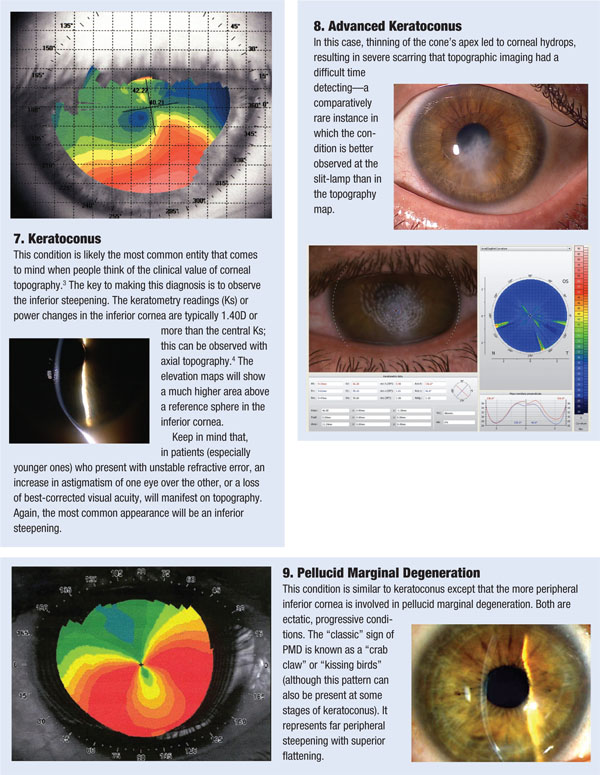
The following examples illustrate the correlation between various corneal etiologies and topography maps. Compare the map and slit-lamp images with the descriptions below.