Doc, my cataract surgery went beautifully—or so I thought. I spent thousands of dollars on this premium lens implant, but I can’t see well anymore. Can you help?”
Unfortunately, this patient has likely developed posterior capsular opacification, or PCO, behind the intraocular lens (IOL) implant. The good news is that a quick, simple, in-office laser procedure can fix this problem for good.
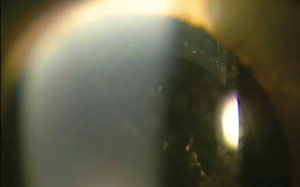 | ||
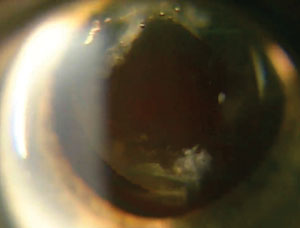
| Posterior capsular opacification (above) occurs in about one in six cataract patients. Fortunately, YAG laser capsulotomy (right) quickly and effectively fixes this complication, and makes patients extremely thankful. |  | |
YAG capsulotomy is a relatively simple procedure that takes only minutes to perform and can make an enormous impact on a patient’s vision. This article—the sixth in a six-part, print-and-video, how-to series—details the step-by-step procedure of a YAG laser capsulotomy.
Posterior Capsular Opacification
Modern cataract surgery involves making a hole in the anterior capsule to remove the lens, while leaving the posterior capsule intact. Unfortunately, this technique can leave behind lens epithelial cells on the anterior capsule and equatorial region. With time, these cells are believed to proliferate and migrate onto the IOL and the posterior capsule, creating a PCO. When enough of these cells build up, they become more opaque and can obscure or scatter the path of light entering the eye, causing patient symptoms. These cells can also cause wrinkling of the capsule, which can interfere with vision.1
Posterior capsular opacification is the most common complication of cataract surgery. Incidence rates used to be as high as 50%; but with improvements in surgical technique, IOL designs and IOL materials, the incidence has decreased to about 14% to 18%.1
The problem may not bother patients for months to years afterward, so they may forget that in-depth conversation you had prior to their surgery about the possibility of its development.
Blurry vision is just one of the symptoms that patients may experience. Other signs and symptoms include hazy or cloudy vision, decreased visual acuity, decreased contrast sensitivity, glare or halos around lights, double vision and asthenopia.
The current standard treatment for PCO is a capsulotomy using a laser.
YAG Capsulotomy
This technique is performed with a neodymium-doped yttrium aluminum garnet (Nd:YAG) laser to make an opening in the posterior capsule along the patient’s visual axis. The Nd:YAG laser uses photodisruption to apply a series of focal ablations to disintegrate the offending tissues. The Nd:YAG laser does not have a thermal reaction or coagulative properties that may cause other complications.
 | |
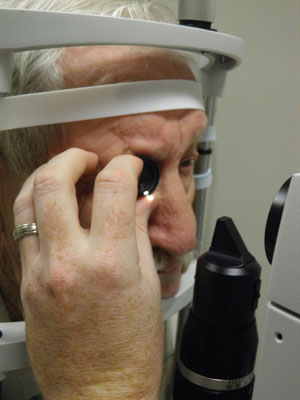
| Patient preparation involves instillation of dilating drops, an alpha-agonist to prevent intraocular pressure spike and proparacaine. The patient should be positioned comfortably at the slit lamp, with good fixation and head position. |
Indications and Contraindications
Consider a YAG capsulotomy when the patient’s symptoms interfere with his or her activities of daily living or when the PCO restricts the ability to monitor or treat a patient’s retinal condition. Thorough education of expectations after the procedure should be addressed with patients, especially if there is pre-existing retinal or macular disease.
Contraindications for YAG capsulotomies include corneal opacities, corneal scars, corneal edema, corneal surface irregularities, intraocular inflammation, cystoid macular edema, red eyes and patients who are unable to hold still. Retinal and/or macular pathologies—including macular hole, vitreomacular traction (VMT) and retinal tears—are other possible contraindications in which the risk-to-benefit ratio of the procedure needs to be considered.
How YAG Capsulotomy is Performed
Prior to the YAG capsulotomy, perform a comprehensive exam including components such as best-corrected visual acuity, contrast sensitivity, glare testing and potential acuity. This should also include a thorough slit lamp exam and fundus evaluation including binocular indirect ophthalmoscopy. If there is concern about the state of the macula, a macular OCT is warranted.
Take a careful patient health history and physical information including allergies, current medications, respiration, pulse and blood pressure. A consent form reviewing indications, contraindications, risks and benefits, and alternative treatments should also be explained and signed by the patient.
After you’ve completed the examination and obtained the proper consent, the steps of a YAG capsulotomy include:
 | |
| A capsulotomy lens may be used to stabilize the eye and allow for better lid control. It also magnifies the target and can allow for better visualization of the treatment area. | |
 | |
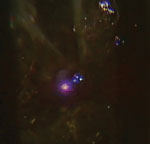
| The Nd:YAG laser in action. This particular laser’s settings display an offset of 125μm, a total number of 23 laser pulses used in the current procedure, a single pulse (1) per press of the button, and a power level of 1.7mJ. |
1. Instillation of dilating drops to get maximum dilation. Prior to dilation, the pupil position as well as the pupil size should be noted, in dim illumination. This is important for determining where and how large the capsulotomy should be.
2. Instillation of one drop of brimonidine or apraclonidine prior to the procedure to help control postoperative pressure spike.
3. Instillation of one drop of proparacaine in each eye to improve patient comfort and to minimize the blink reflex.
4. Adjustment of the laser settings:
- Power/Energy is initially set between 0.8mJ to 2.5mJ. Power can vary from laser to laser as well as from patient to patient and how dense the PCO is. The “golden rule” for any laser is to use the least amount of energy at the lowest setting to get the job done. Our typical starting energy is 1.2mJ to 1.8mJ.
- Spot size and duration are fixed, meaning they cannot be altered on a YAG laser.
- Number of pulses per shot should be one, which means one pulse of laser energy is fired at the capsule every time the button is pressed; however, this can be adjusted on a per laser and per patient basis. (For other laser procedures that employ the YAG laser, such as a laser peripheral iridotomy, the pulses may be increased to two or three, depending on the patient and the thickness of the iris.)
- The offset of the laser should be set between 125µm to 250µm posteriorly. The laser energy works anterior toward the front of the eye and therefore aiming slightly into the anterior vitreous will cause the energy to travel anteriorly and disrupt the posterior capsule and eliminate the PCO. So, the offset setting allows the operator to aim directly on the capsule with the helium-neon (“HeNe”) aiming beams, yet in actuality the laser pulse will strike 125µm to 250µm posterior to that because of the offset.
Another benefit of the offset is it helps to prevent IOL pits.
5. The patient should be aligned comfortably in the slit lamp. Good fixation and head position should be emphasized. Also, patients should be educated that they should not be alarmed if they hear small “snaps” or “claps” from the laser or see sparks of light during the procedure.
6. Some practitioners prefer to use a capsulotomy lens, which is a small lens similar to a flanged gonioscopy lens. The advantages of using the lens is to stabilize the eye and allow for better lid control; it also magnifies the target and can allow for better visualization of the treatment area. Just like with gonioscopy lenses, there can be bubble formation upon insertion and there may be reflections from the lens sometimes making the procedure more difficult. The choice of whether to use a capsulotomy lens or not is strictly up to the treating clinician and which laser is used.
7. With the laser turned on, the HeNe beams should be aimed at the posterior capsule. The HeNe laser emits two separate red beams that, when focused, become one. (Again, the laser energy will be applied 125µm to 250µm behind the posterior capsule because the offset of the laser is set behind the area of focus.)
8. Starting outside the visual axis, each laser shot is targeted such that one is placed adjacent to the next. There are multiple patterns in which the capsule can be opened; the most common is the cruciate, or cross-like, pattern, which creates a vertical and horizontal cross in the posterior capsule. Our preference with the cruciate pattern is to start at 12 o’clock and work our way down to 6 o’clock—this allows for good efficiency and usually lends itself to the least amount of laser shots and energy into the eye, and minimizes complications. During the procedure, no “laser burns” will be observed. Typically the examiner will just see an opening of the capsule as the procedure is performed. Once that is complete, we enlarge the opening in both the nasal and temporal aspects until a sufficient opening is created. Other patterns include the offset cruciate, horseshoe/arch shape, and circular.
 |  | |
| The laser emits two separate beams (the double red dots) that are used for focusing just behind the posterior capsule. | When the beams are focused, they appear as one. The pulse of laser energy hits the posterior capsule and ablates the tissue. |
9. Once finished, the posterior capsule should be inspected without the laser lens and in retro-illumination to ensure that there are no major strands or areas that need to be opened further. Initially, the capsular bag may not appear fully open; but with time the flaps will settle out and expand, leaving a central hole in the bag. We typically try to make the opening about 4mm to 6mm, which is usually about the pupil size in dim illumination.
10. Thorough documentation with any procedure is vitally important. All the laser settings—including the number of shots, energy per shot, and total energy used for the procedure—should be documented.
11. Once finished with the laser, one drop of brimonidine or apraclonidine should be instilled to help control postoperative pressure spike.
12. Intraocular pressure should be checked again 30 to 60 minutes post-procedure to ensure that it is not rising. (Measuring IOP immediately after the procedure may give a false sense of security as IOP typically takes one to three hours to elevate, if it does rise post-procedure.) If IOP is acceptable and close to the preoperative intraocular pressure, the patient is sent home with a topical anti-inflammatory to be used for five to seven days to decrease inflammation after the procedure. Our preference is for maximal therapy, such as topical Pred Forte (prednisolone acetate 1%, Allergan) dosed QID.
Before leaving the office, the patient should be alerted to the potential for flashes of light, floaters, spots in their vision and/or drastically reduced vision, and educated to return to the clinic immediately if any of these occur.
   |
| Each laser shot is placed adjacent to the next. In this patient’s procedure, the laser bursts are performed in a cross-like pattern—a simple and energy-efficient design—beginning from the top of the posterior capsule to the bottom, and then from left to right. |
13. The patient should be followed up in one week for a thorough dilated fundus exam as well as reassessment of visual acuity and IOP. If the desired outcome was reached at this visit, the other eye can be treated if necessary.
Complications
As with any ocular procedure, there are potential complications that the patient should be educated about. Increased intraocular pressure is a common finding after YAG capsulotomies. Increased IOP tends to maximize at one to three hours post-laser and return to close to normal within 24 hours due to the laser energy quickly dissipating from the eye. Patients with glaucoma or elevated intraocular pressures prior to the procedure are more likely to have a pressure spike and should be followed more closely in the postoperative period. Other factors, such as increased total laser energy and larger capsulotomy size, are also associated with increased IOP.2
  | |
| The posterior capsule should be inspected (left) without the laser lens and in retroillumination to ensure that there are no major strands or areas that need to be opened further. If so, the remaining “flaps” should be removed (right) to create a full central hole. |
Postoperative inflammation in the form of an anterior uveitis is the second most common potential complication with any anterior segment laser procedure. This is managed with the topical anti-inflammatory for five to seven days after the procedure. However, it is incredibly rare to see a clinically significant iritis after a capsulotomy.
A more serious complication that can occur with YAG capsulotomy is a retinal detachment. While rare, it is important to perform a thorough dilated fundus exam prior to performing the procedure. Such a retinal detachment is believed to be caused from the loss of the intact posterior capsule or laser shockwaves, which induce vitreous changes.2 Pre-existing retinal conditions such as high myopia or lattice with holes are risk factors for retinal detachments after surgery. Other factors such as larger capsulotomy size and higher total energy can also lead to increased risk for retinal detachments.2
Patients commonly experience an initial increase in floaters, but these should resolve within a few days as the tissues settle. Other complications that can occur after capsulotomy include cystoid macular edema, damage to the IOL in the form of pits, slight movement in IOL position, corneal edema, iris hemorrhage and vitreous prolapse. While complication rates are rare, it is essential to perform a comprehensive eye exam and to thoroughly explain all the risk and benefits to the patient prior to performing a YAG capsulotomy.2
Billing and Coding
The Current Procedural Terminology (CPT) code for the YAG capsulotomy procedure is 66821 with a 90-day global follow-up period. The International Classification of Disease (ICD-9) code for posterior capsule opacification is 366.53.
 | |
| We typically make the final opening about 4mm to 6mm, which is usually about the pupil size in dim illumination. Thirty to 60 minutes post-procedure, the intraocular pressure should be rechecked to make sure that it is not spiking. |
Posterior capsular opacification is a relatively common occurrence in the months to years after cataract surgery. It can leave patients frustrated and searching to find a solution.
A YAG laser capsulotomy is one of the most rewarding procedures that optometrists can be a part of. Optometrists in three states (Oklahoma, Kentucky and Louisiana) can now be certified to perform this procedure, and optometrists all across the country recognize and comanage the condition successfully with our ophthalmology colleagues.
A recent patient of ours came in for the one-week YAG-laser post-op, and nearly knocked us over with a bear hug stating that “she hadn’t seen this well in years.” Your patient will leave knowing that you gave them the best, most advanced care possible and will be raving about how you restored their vision to how it should be after cataract surgery.
Dr. Boucher is currently completing her residency in Ocular Disease and Family Practice at NSU Oklahoma College of Optometry.
Dr. Ellis is currently completing her residency in Optometric Management at NSU Oklahoma College of Optometry.
Dr. Lighthizer is the assistant dean for clinical care services, director of continuing education, and chief of both the specialty care clinic and the electrodiagnostics clinic at NSU Oklahoma College of Optometry.
1. Levin LA, Albert DM. Ocular Disease: Mechanisms and Management. Philadelphia: Saunders; 2010.2. Aslam TM, Devlin H, Dhillon B. Use of Nd:YAG laser capsulotomy. Surv Ophthalmol. 2003 Nov-Dec;48(6):594-612.

