 |  |
When a patient has an elevated optic nerve head (ONH) with blurred disc margins, alarm bells should go off. These could be harbingers of true papilledema caused by an underlying systemic process or mass lesion in need of urgent treatment.
But these signs could also be pseudopapilledema. Optic nerve head drusen (ONHD), the most common etiology of pseudopapilledema, are found in approximately 1% of the population with bilateral distribution in 75% to 85%.1-3 Although patients with benign ONHD are often asymptomatic, the drusen can cause elevation, congestion and blurred margins of the optic nerve, simulating papilledema.
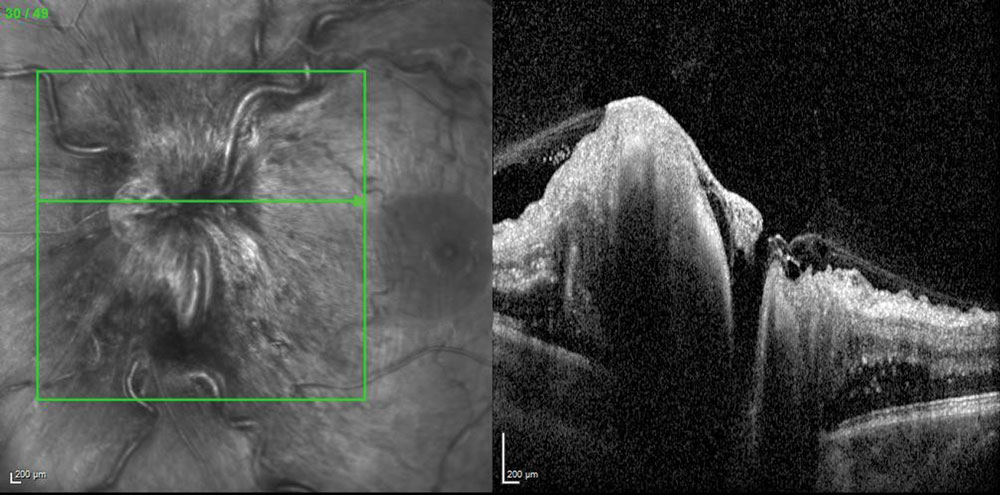 |
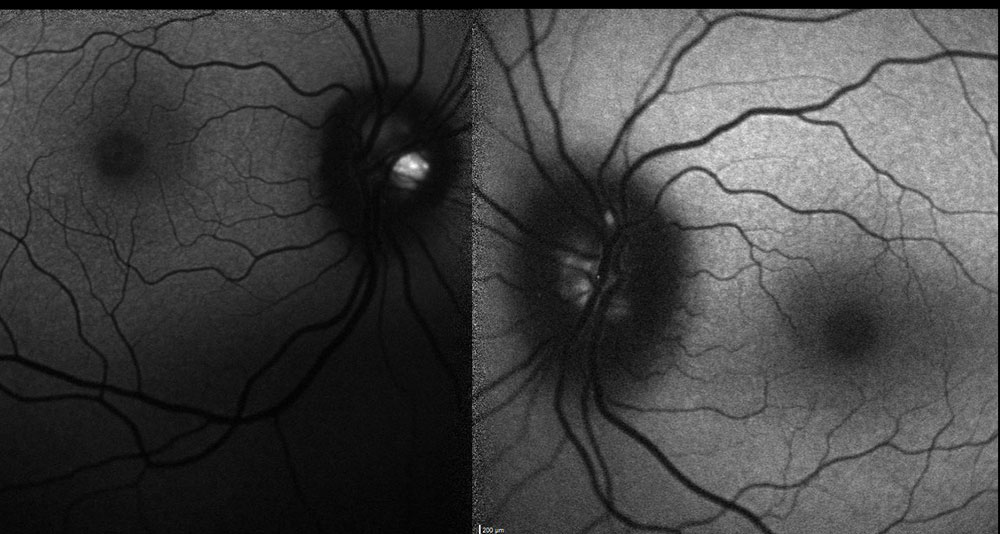
| Fig. 1. SD-OCT of a patient with papilledema shows the shadow or darkening of the deeper structures. |
Patients with ONHD are often asymptomatic, leading to a high rate of incidental discovery. Visual inspection of an elevated ONH is often insufficient to confirm pseudopapilledema and rule out a more serious diagnosis. Thus, a multitude of tests—including radiologic neuroimaging and a spinal tap—are warranted to rule out an intracranial mass or lesion and to assess for increased intracranial hypertension. Many other useful diagnostic tests are available in the optometric setting to assess ONHD, including spectral domain OCT (SD-OCT), fundus autofluoresence (FAF), intravenous fluorescein angiography (IVFA), OCT angiography (OCT-A) and B-scan ultrasonography.
SD-OCT can be quite helpful in differentiating pseudopapilledema from true papilledema, as the latter will show nerve fiber layer edema on SD-OCT imaging, which may cast a shadow on the structures below (Figure 1). ONHD, on the other hand, will be hyper-reflective on SD-OCT.
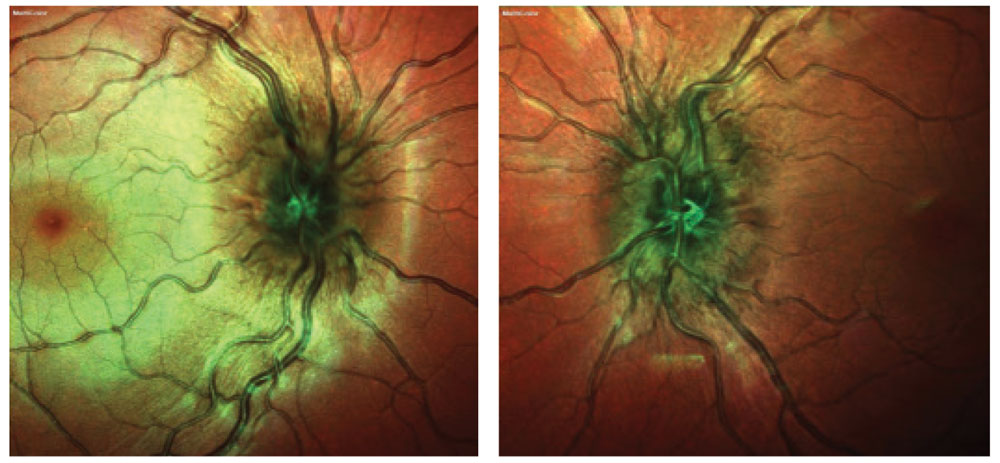 |
| Fig. 2. Color fundus images reveal crowded elevation of the ONH with indistinct margins in both eyes. |
Blurry Signs
Cases by Dr. Shechtman
Case 1. An 11-year-old Caucasian female with an elevated ONH was referred to rule out papilledema. She had no visual complaints and denied headaches. Her visual acuities measured 20/20 OU, intraocular pressures (IOPs) measured 15mm Hg OD and 14mm Hg OS, pupil assessment was normal without afferent pupillary defect (APD) and her body mass index (BMI) was 21.0. Her anterior segment examination was unremarkable, but her dilated examination revealed a congested ONH in each eye with blurred disc margins (Figure 2). We then performed SD-OCT, FAF and B-scan ultrasonography (Figure 3), which helped us diagnose her with buried ONHD and advise annual follow-up.
ONHD are generally seen well with FAF; however, in younger patients, as in this case, the drusen deposits are more posterior and may not been seen until later in life.
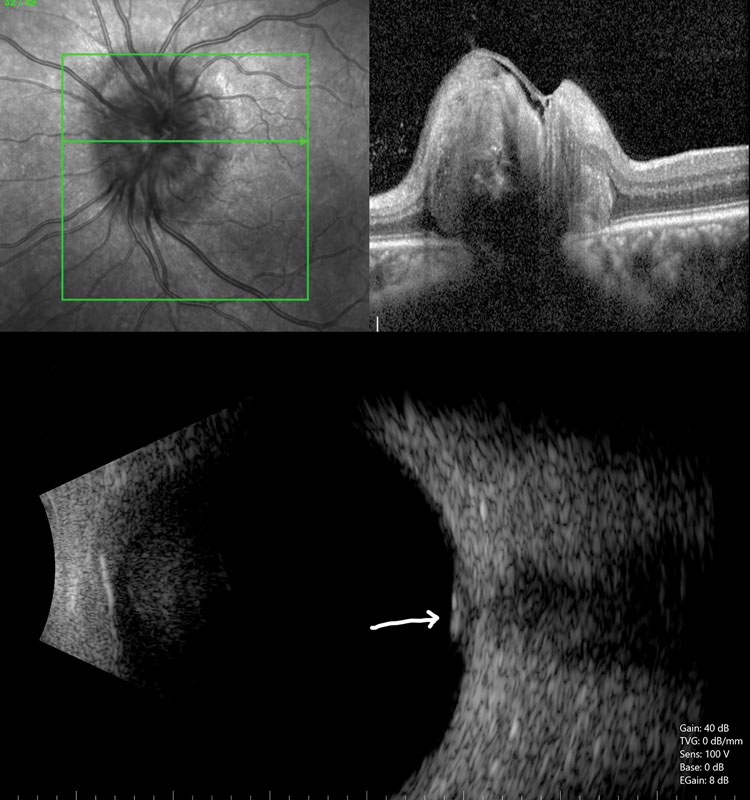 |
| Fig. 3. SD-OCT, top, and ultrasonography, bottom, show hyper-reflective lesions deep in the ONH consistent with drusen. Findings were similar in both eyes. |
Case 2. A 37-year-old Hispanic woman was referred by her neurologist for an evaluation of optic nerve edema. She was diagnosed with papilledema by a local ophthalmologist who then referred her to neurology. However, her radiologic neuroimaging and lumbar puncture were both normal, and the neurologist referred her for a retinal consultation. Her chief complaint was headaches, which were later attributed to probable migraine. Her past medical history was negative. Her visual acuity measured 20/20 OU, IOPs measured 20mm Hg OD and 21mm Hg OS, pupil assessment was normal without APD and her BMI was 27.0. Her anterior segment examination was unremarkable, but dilation revealed congested ONHs with blurred disc margins. Her IVFA was normal without late leakage as we would expect with papilledema. Her SD-OCT and FAF images confirmed the diagnosis of ONHD (Figures 4 and 5).
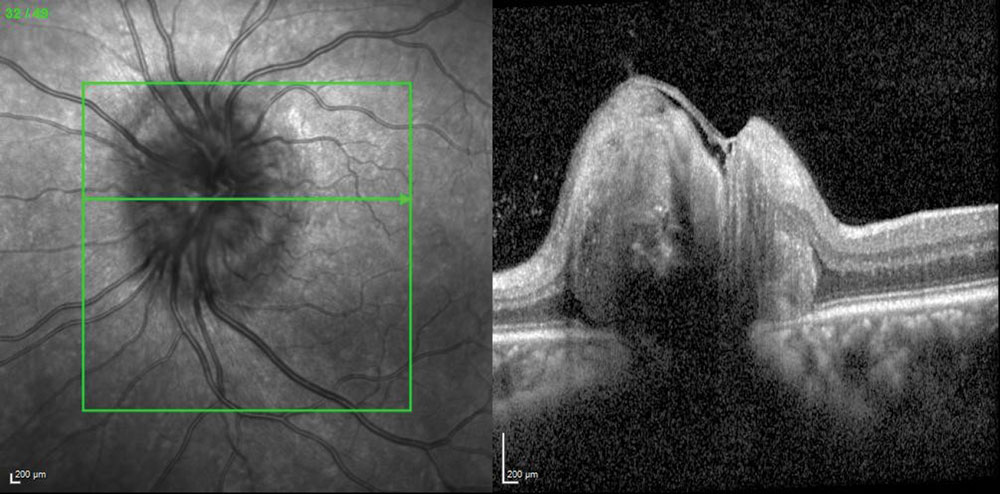 |
| Fig. 4. SD-OCT of the left eye shows hyper-reflective lesions deep in the ONH consistent with drusen. The right eye shows similar findings. |
A Diagnostic Roadmap
Commentary by Dr. Shechtman and Dr. Taher
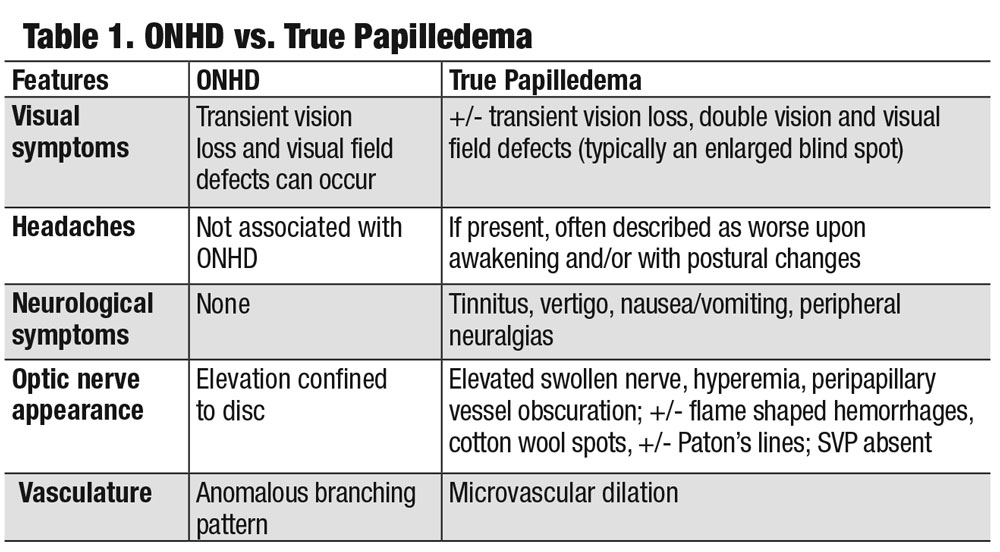
Although no set protocols exist for the assessment of pseudopapilledema vs. true papilledema, a comprehensive eye examination with a dilated fundus evaluation and the use of various diagnostic modalities can be quite valuable when distinguishing between the two (Table 1).
 |
| Fig. 5. FAF confirmed focal hyperautofluoresence of the ONH consistent with lipofuscin (ONHD) in both eyes. |
We have found that IVFA is particularly useful in distinguishing papilledema from pseudopapilledema by revealing ONH leakage. On ultrasonography, another helpful diagnostic tool, drusen appear as hyper-reflective calcified bodies in the optic nerve and will continue to show increasing brightness even at a low gain. Other ancillary testing such as OCT, visual fields and FAF can also be helpful. SD-OCT of ONHD can reveal an elevated disc with a characteristic “lumpy-bumpy” appearance. A nerve with true papilledema, however, may reveal a smooth internal contour of the ONH with a characteristic hyporeflective “V” pattern in the subretinal space adjacent to the ONH. Although these are distinct findings, SD-OCT alone should not be used to distinguish between the two conditions. Furthermore, because the calcific properties of drusen have inherent autofluorescent ability, ONHD will show hyperfluorescence on FAF. Drusen autofluorescence is inversely proportional to its depth, meaning deeply buried drusen may be difficult to assess. Additionally, if the cause of pseudopapilledema is not ONHD, FAF would show unremarkable findings.
 |
Although ONHD are often found in isolation, they may be associated with other ocular findings, such as angioid streaks, that correlate with underlying conditions. Additionally, lowering IOP in patients with ONHD can help prevent progressive optic neuropathy and slow visual field loss, but ONHD are dynamic and can cause shifts of the refractile bodies at any time.
In any case where the diagnosis of pseudopapilledema is not confirmed, referral to a neuro-ophthalmologist is warranted. True papilledema requires an immediate referral for radiological imaging, such as MRI or CT MRA/MRV, followed by lumbar puncture.
| 1. Auw-Haedrich C, Staubach F, Witschel H. Optic disk drusen. Surv Ophthalmol. 2002:47(6):515-32. 2. Erkkila H. Clinical appearance of optic disc drusen in childhood. Albrecht Von Graefes Arch Klin Exp Ophthalmol. 1975;193(1):1-18. 3. Mehrpour M, Torshizi F, Esmaeeli S, et al. Optic nerve sonography in the diagnostic evaluation of pseudopapilledema and raised intracranial pressure: A cross-sectional study. Neurology Research International. 2015:Article ID 146059. |

