 |
A 34-year-old male presented with complaints of blurred vision in both eyes and headaches over the past few weeks. He reported that he never had vision problems before.
His systemic history was significant for Type 2 diabetes and end-stage kidney disease. While awaiting a kidney transplant he was hospitalized for 10 days with related complications. He just got out of the hospital the day he visited our clinic. He reported his hemoglobin A1c was 6.8 and his blood sugar two days earlier was 94. He also had high blood pressure for which he was medicated.
On examination, his best-corrected visual acuity was 20/50 OD and 20/30 OS. Extraocular motility testing was normal. Confrontation fields were full-to-careful finger counting OU. His pupils were equally round and reactive to light, with no afferent pupillary defect (APD). His anterior segment exam was unremarkable OU. His intraocular pressure (IOP) measured 14mm Hg OU.
Dilated fundus exam revealed changes as seen in the fundus photos. An OCT was performed and is available for review.
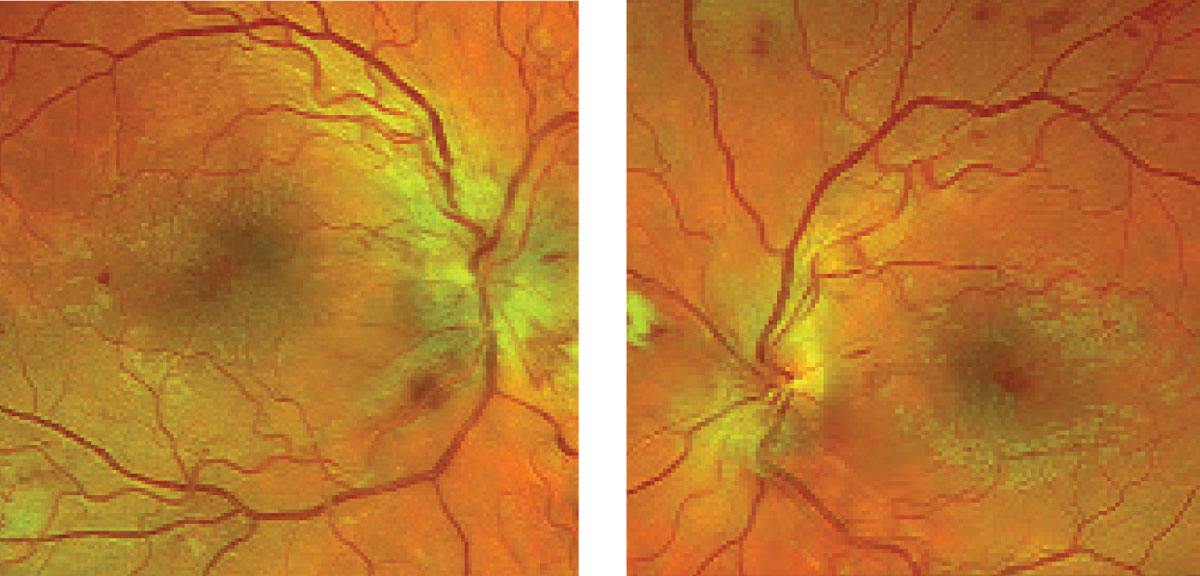 |
| What structural changes can these images of the right (at left) and left fundus reveal, and can it help explain this kidney disease patient’s visual presentation? Click image to enlarge. |
Take the Retina Quiz
1. What additional testing would be most helpful in making a diagnosis?
a. Fluorescein angiography.
b. MRI scan.
c. Blood pressure.
d. Erythrocyte sedimentation rate and C-reactive protein.
2. How would you characterize the optic nerves in this patient?
a. Physiologic.
b. Neovascularization of the disc.
c. Bilateral disc swelling.
b. Ischemic.
3. How would you characterize the retinal findings?
a. Mild microvascular retinal changes.
b. Moderate-to-severe retinal vascular changes.
c. Severe retinal ischemia.
d. Proliferative disease.
4. What is the most likely diagnosis?
a. HTN retinopathy.
b. NPDR with center-involved DME.
c. Combined HTN retinopathy and NPDR.
d. CRVO OU.
5. How should this patient be managed?
a. Referral for consideration of anti-VEGF therapy.
b. Visual field and neuro-ophthalmology consult.
c. Lumbar puncture and MRI.
d. Immediate referral to the emergency department for blood pressure control.
For answers, see below.
Diagnosis
Optic nerve swelling was evident in both eyes, as were scattered cotton-wool spots as well as retinal hemorrhages. On further questioning, our patient said that when he was admitted to the hospital, his blood pressure was 220/190. Based on the guidelines established by the Joint National Committee (JNC) on Prevention, Detection, Evaluation and Treatment of High Blood Pressure, our patient was clearly having a hypertensive emergency. The disc swelling we saw was likely a sequela from this hypertensive event. Fortunately, they were able to get his blood pressure under control. By the time he came to us, it was 135/070.
Based on the JNC guidelines systolic blood pressure (SBP) >179mm Hg or diastolic blood pressure (DBP) >109mm Hg is classified as “hypertensive crisis.” Hypertensive crisis can be further categorized as either hypertensive emergency or hypertensive urgency.1
End-organ damage in the presence of significantly elevated blood pressure is classified as hypertensive emergency whereas hypertensive crisis occurs in the absence of end organ damage. Then it is classified as hypertensive urgency. End-organ damage may manifest in the central nervous system, eye, heart (left ventricular dysfunction) and kidney.
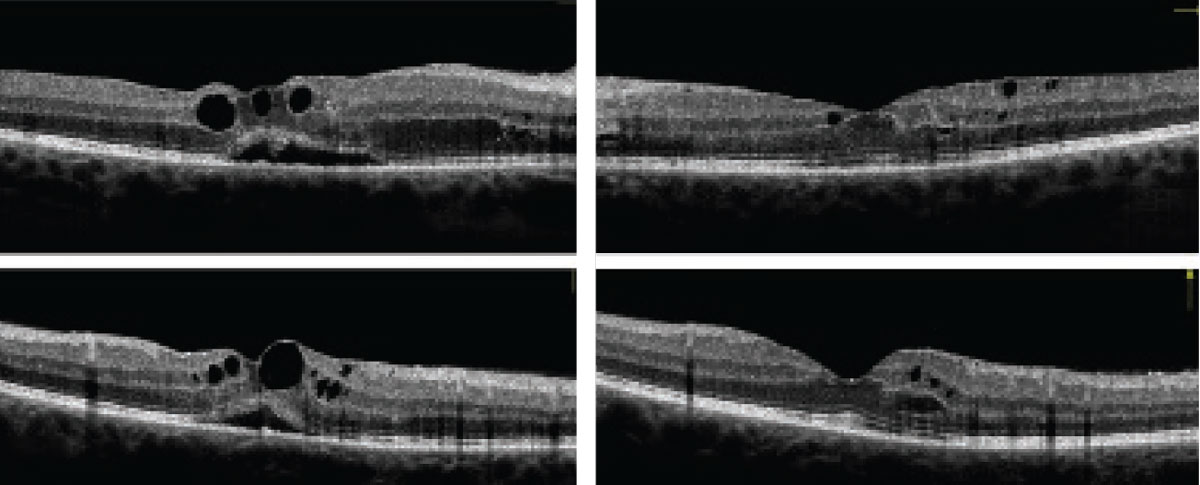 |
| Can these OCT images of the right (at left) and left eyes reveal our 34-year-old patient’s diagnosis? Click image to enlarge. |
However, not everything on his retinal exam resulted from high blood pressure. His diabetes also played a role. He had scattered retinal hemorrhages, exudate and fluid in each macula. This fluid in the macula is easily visualized on the SD-OCT scan where several large retinal cysts, as well as puddle of subretinal fluid, were visible in the right eye. The left eye also had fluid, but not as much. The macular edema was a bit confounding. Did it arise from the diabetes or the disc swelling associated with the hypertensive crisis?
Our impression was that it was more likely from his diabetic retinopathy (DR). The DR seems worse in his right eye as there were scattered retinal hemorrhages in four quadrants, which puts him at a level of severe non-proliferative diabetic retinopathy (NPDR). The left eye was not as bad. We only noted a moderate case of NPDR.
Discussion
The combination of uncontrolled blood pressure and diabetes does not bode well for our patient. Unfortunately, he’s not alone. Approximately 75 million Americans, or about one in three, have hypertension and only 54% control their blood pressure.2 The combination of hypertension and diabetes is also common, affecting 30% of patients with younger onset diabetes and 75% of people with older-onset.3 To make matters worse, in many of these patients, blood pressure is poorly controlled. In those with younger-onset diabetes only 60% of patients have their blood pressure controlled; in older-onset diabetes, it’s even worse with only 42% achieving blood pressure control.3 This combination puts patients at a higher risk of cardiovascular disease, nephropathy and amputation.
Our patient already has kidney failure and is awaiting a transplant. The current American Diabetes Association guidelines recommend a treatment goal of SBP <140mm Hg and DBP <90mm Hg for most patients with diabetes. Lower systolic and diastolic blood pressure targets, such as <130/80mm Hg, may be appropriate for individuals at high risk of cardiovascular disease, if they can be achieved without undue treatment burden.4 Our patient at this point seems to have achieved this goal.
Our patient was referred to a retina specialist to evaluate his macular edema. The specialist elected to observe the patient closely to see if the edema would resolve with better blood pressure and blood sugar control. No doubt the optic nerve swelling will slowly resolve, but it would have been interesting to see the extent and severity when he presented to the hospital 10 days earlier. Hopefully, he has turned the corner for the better and he will get the necessary care that is required to maintain good vision and a good quality of life.
Dr. Dillinger practices at Horizon EyeCare in Owatonna, MN.
1. The fifth report of the Joint National Committee on Detection, Evaluation, and Treatment of High Blood Pressure. Arch Intern Med. 1993;153,154-183. 2. Merai R, Siegel C, Rakotz M, et al. CDC Grand Rounds: A Public Health Approach to Detect and Control Hypertension. MMWR Morb Mortal Wkly Rep. 2016;65(45):1261-4. 3. Klein R, Klein B. Blood pressure control and diabetic retinopathy. Br J Ophthalmol. 2002; 86(4):365-7. 4. Passarella P, Kiseleva T, Valeeva F, et al. Hypertension management in diabetes: 2018 Update. Diabetes Spectrum. 2018;31(3):218-24. |
Retina Quiz Answers:
1) c; 2) c; 3) b; 4) c; 5) a.

