 | |
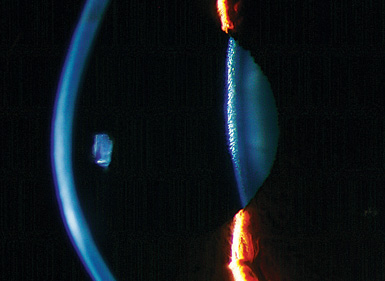
| This patient presented with allmark findings associated with keratoconus.
Could corneal collagen crosslinking slow disease progression in this patient? |
Preliminary testing and laser refractive technology have continued to advance, allowing for safer, more predictable procedures and improved surgical outcomes. From placido disc corneal curvature topography to anterior and posterior corneal elevation, curvature and corneal thickness maps, optometrists are better positioned to identify corneal abnormalities than ever before.
Nevertheless, some patients are still deemed non-candidates and consequently may suffer from debilitating progressive vision loss. Several years ago, LASIK eclipsed photorefractive keratectomy (PRK) as the primary mode for laser vision correction surgery. While the incidence of post-LASIK ectasia is low, with reported rates from 0.04% to 0.2%, clinicians are meticulous about screening patients’ corneal maps.1,2
When suspicious signs of potential preoperative keratoconus or other risk factors are found, the patient typically is considered a non-candidate. The same is true for patients with very thin corneas or those who require very deep excimer laser treatments for full ametropia correction. Fortunately, corneal collagen crosslinking (CXL) may allow certain patients with preexisting ectatic conditions or extremely thin corneas to enjoy the benefits of laser vision correction. Here, we’ll discuss how CXL may help expand the refractive surgery market in the near future.
CXL 101
For several years, corneal collagen crosslinking (CXL) has been employed to slow or halt ectatic disease by stabilizing the weakened corneal infrastructure.3 While not yet approved by the FDA, CXL has gained popularity around the world and in US clinical trials. Relatively long-term data over a four- to six-year period indicated that CXL is successful at stopping the progression of keratoconus.4In a corneal collagen crosslinking procedure, the clinician saturates the cornea with topical riboflavin applied to the surface and then exposes the tissue to a narrow spectrum of UV-A. The procedure creates a biochemical reaction when the riboflavin is photo-activated, resulting in increased covalent bonding between collagen fibers.5 This process increases the biomechanical strength and rigidity of the corneal stroma. CXL’s ability to arrest disease progression is well-documented, with published results showing a 98% to 100% success rate.6,7
It’s also worth noting that, in addition to keratoconus, practitioners abroad have used CXL to treat a wide range of conditions, including microbial keratitis and pseudophakic bullous keratopathy.8,9
Combined CXL and Laser Vision Correction
If the corneal stability achieved by CXL is permanent, could it be a cure for post-LASIK ectasia? In other words––could the procedure help broaden the market for laser vision correction by permitting some traditional non-candidates to undergo LASIK? It seems rather likely, but this notion is still in its infancy. Corneal collagen crosslinking typically induces some corneal flattening and hyperopic shift.10Therefore, these variables must be considered during a combined excimer laser surgery and CXL procedure to ensure accurate, predicable results. While the incidence of keratoconus in the general population is low—maybe as modest as 0.01%—it may be closer to 1% among refractive surgery candidates.4 While still a relatively low figure, it poses a clinically significant concern because many patients with keratoconus may seek surgery for ametropia correction. Clinical evidence suggests that the application of CXL in conjunction with surface ablation or LASIK could prevent regression in hyperopic patients, prove beneficial with femtosecond astigmatic keratectomy, provide enhanced biomechanical stability in the treatment of high-risk patients with keratoconic corneas––such as those with forme fruste or frank keratoconus. To date, many researchers have initiated successful protocols for combined laser vision correction CXL.11-14
• Hyperopia correction. In 2008, A. John Kanellopoulos, MD, introduced a procedure that included combined high-irradiance, short-exposure CXL and myopic LASIK––termed “LASIK Xtra” (Avedro, Inc.).14,15 Then in 2012, he and several colleagues described a second combination procedure involving hyperopic LASIK and prophylactic intrastromal CXL in the Journal of Refractive Surgery.15 In this study, 34 patients received combined hyperopic LASIK and CXL in one eye and only hyperopic LASIK in the other. The protocol for CXL was 0.1% sodium phosphate riboflavin solution delivered under the flap followed by a three-minute treatment with 10mW/cm2 UV-A light. The preoperative mean spherical equivalent refraction was +3.15D +/- 1.46D in the combined procedure group and +3.40D +/- 1.78D in the LASIK- only group. At a mean follow-up of 23 months, the average spherical equivalent refraction measured -0.20D +/- 0.56D in the combined procedure group and +0.20D +/- 0.40D in the LASIK-only group. The analysis showed that eyes that underwent hyperopic LASIK without CXL exhibited greater regression (+0.72D +/- 0.19D) than eyes that had the combined procedure (+0.22D +/- 0.31D).15
Although the sample size was limited, follow-up revealed a statistically significant difference in hyperopic regression between the two groups. This finding indicated that a larger volume of successful refractive outcomes is achievable with the application of combined hyperopic LASIK and CXL.
• Astigmatism correction. In a separate study, Dr. Kanellopoulos and associates evaluated the use of same-day, combined surface ablation and CXL for the treatment of astigmatism and myopia in patients with keratoconus.16 The authors theorized that combined photorefractive keratectomy (PRK) and CXL might have a synergistic effect on thin ectatic corneas, because of the corneal remodeling that occurs during PRK.Their protocol began with a 6.5mm phototherapeutic keratectomy (PTK) of 50μm of epithelium. Then, topography-guided PRK using Pentacam HR (Oculus) was performed with a 5.5mm optical zone centered on the corneal apex using the Allegretto excimer laser platform (Alcon). Immediately afterward, the researchers applied 0.002mg/mL of mitomycin C for 30 seconds. Next, 0.1% sodium phosphate riboflavin solution was instilled into the cornea every two minutes over a 10-minute duration. Then, UV-A light irradiated at 5-mW/cm² was applied for 18 minutes. The study evaluated 325 total eyes––127 were treated in a conventional sequential fashion and 198 underwent a same-day, combined procedure. The sequential group exhibited a mean improvement in uncorrected visual acuity from 20/160 to 20/63. Those who received same-day surgery, experienced a mean improvement in uncorrected visual acuity from 20/180 to 20/40.16
Also, those in the same-day group achieved a statistically significant reduction in mean manifest refraction spherical equivalent and keratometry values.The researchers determined that PRK followed by same-day CXL actually prevents ablation of crosslinked corneal tissue––unlike when CXL is performed before PRK.16 Further, they noted that PRK and CXL are beneficial––both from a refractive and a therapeutic perspective––for patients with keratectasias. Finally, they determined that same-day, combined procedures yield better visual outcomes than sequential procedures.16
• Enhanced surgical stability. In a case series of 14 patients with keratoconus, researchers assessed the efficacy, predictability, safety and stability of a combined treatment that featured customized PRK and prophylactic CXL for residual refractive error correction after lamellar keratoplasty.17 The mean residual ametropia was -6.11D, with a range from
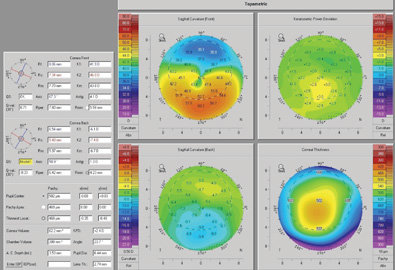 | ||||||
| Corneal collagen crosslinking could be used to prevent ectasia following LASIK,
as seen here. | ||||||
|
Corneal collagen crosslinking has been shown to slow or halt progression of keratoconus and post-LASIK ectasia. However, more research is required and existing nomograms need to be refined to more accurately predict procedural end points. While the incidence of keratoconus may be greater in a refractive surgery practice than in the general population, it’s still low. Thus, the potential to treat these patients serves to broaden the refractive surgery market––but only modestly. However, the possibility of improved uncorrected and best-corrected vision through simultaneous protective adjunct therapy is exciting.
Dr. Walker is a resident in refractive and ocular surgery at BVA Advanced Eye Care in Edmond, Okla., and nJoy Vision Oklahoma City in affiliation with Northeastern State University Oklahoma College of Optometry. Dr. Freeman is clinical director at nJoy Vision Oklahoma City and president of the Optometric Council on Refractive Technology (OCRT). He is also an adjunct assistant professor of optometry at Northeastern State University Oklahoma College of Optometry.
1. Randleman JB, Russell B, Ward MA, et al. Risk factors and prognosis for corneal ectasia after LASIK. Ophthalmology. 2003 Feb;110(2):267-75.2. Rad AS, Jabbarvand M, Saifi N. Progressive keratectasia after laser in situ keratomileusis. J Refract Surg. 2004 Sep-Oct;20(5 Suppl):S718-22.3. Koller T, Mrochen M, Seiler T. Complication and failure rates after corneal crosslinking. J Cataract Refract Surg. 2009 Aug;35(8):1358-62. 4. O’Brart, DP, Kwong TQ, Patel P, et al. Long-term follow-up of riboflavin/ultraviolet A (370nm) corneal collagen cross-linking to halt the progression or keratoconus. Br J Ophthalmol. 2013 Apr;97(4):433-7.5. Sung HW, Chang WH, Ma CY, Lee MH. Crosslinking of biological tissues using genipin and/or carbodiimide. J Biomed Mater Res A. 2003 Mar 1;64(3):427-38.6. Raiskup-Wolf F, Hoyer A, Spoerl E, Pillunat LE. Collagen crosslinking with riboflavin and ultraviolet-A light in keratoconus: long-term results. J Cataract Refract Surg. 2008 May;34(5):796-801.7. Wittig-Silva C, Whiting M, Lamoureux E, et al. A randomized controlled trial of corneal collagen cross-linking in progressive keratoconus: preliminary results. J Refract Surg. 2008 Sep;24(7):S720-5.8. Makdoumi K, Mortensen J, Crafoord S. Infectious keratitis treated with corneal crosslinking. Cornea. 2010 Dec;29(12):1353-8.9. Ghanem RC, Santhiago MR, Berti TB, et al. Collagen crosslinking with riboflavin and ultraviolet-A in eyes with pseudophakic bullous keratopathy. J Cataract Refract Surg. 2010 Feb;36(2):273-6.10. Copeland RZ, Afshari NA. Copeland and Afshari’s Principles and Practice of Cornea. 1st ed. New Delhi, India: Jaypee-Highlights Medical Publishers, Inc., 2012. 11. Kanellopoulos AJ. Comparison of sequential vs same-day simultaneous collagen cross-linking and topography-guided PRK for treatment of keratoconus. J Refract Surg. 2009 Sep;25(9):S812-8.12. Kymionis GD, Kontadakis GA, Kounis GA, et al. Simultaneous topography-guided PRK followed by corneal collagen cross-linking for keratoconus. J Refract Surg. 2009 Sep;25(9):S807-11.13. Nguyen MK, Chuck RS. Corneal collagen cross-linking in the stabilization of PRK, LASIK, thermal keratoplasty, and orthokeratology. Curr Opin Ophthalmol. 2013 Jul;24(4):291-5.14. Kanellopoulos AJ, Pamel GJ. Review of current indications for combined very high fluence collagen cross-linking and laser in situ keratomileusis surgery. Indian J Ophthalmol. 2013 Aug;61(8):430-2.15. Kanellopoulos AJ, Khan J. Topography-guided hyperopic LASIK with and without high irradiance collagen cross-linking: Initial comparative clinical findings in a contralateral eye study of 34 consecutive patients. J Refract Surg. 2012 Nov;28(11 Suppl):S837-40.16. Kanellopoulos AJ, Binder PS. Management of corneal ectasia after LASIK with combined, same-day, topography-guided partial transepithelial PRK and collagen cross-linking: The Athens Protocol. J Refract Surg. 2011 May;27(5):323-31. 17. Spadea L, Paroli M. Simultaneous topography-guided PRK followed by corneal collagen cross-linking after lamellar keratoplasty for keratoconus. Clin Ophthalmol. 2012;6:1793-800.


