 |
History
A 44-year-old male presented to the office for a routine eye exam. He reported that his vision was fine at distance but that he now needed reading glasses. He denied previous surgery or any history of glaucoma, but he did say he incurred a blunt trauma—hit in the face with a football—to his right eye three years earlier. He denied systemic diseases and allergies of any kind.
Diagnostic Data
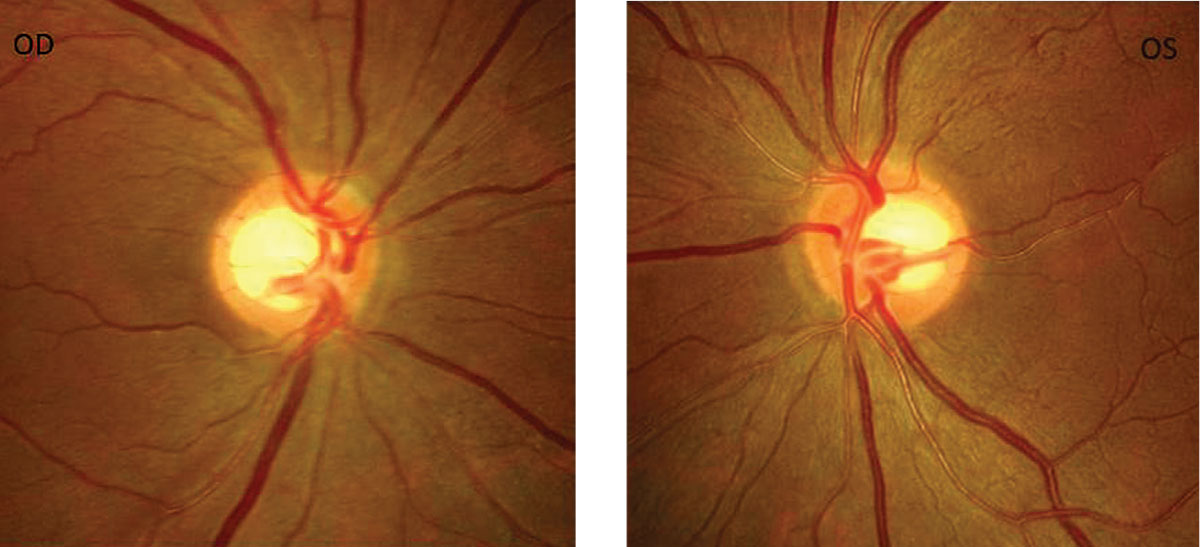
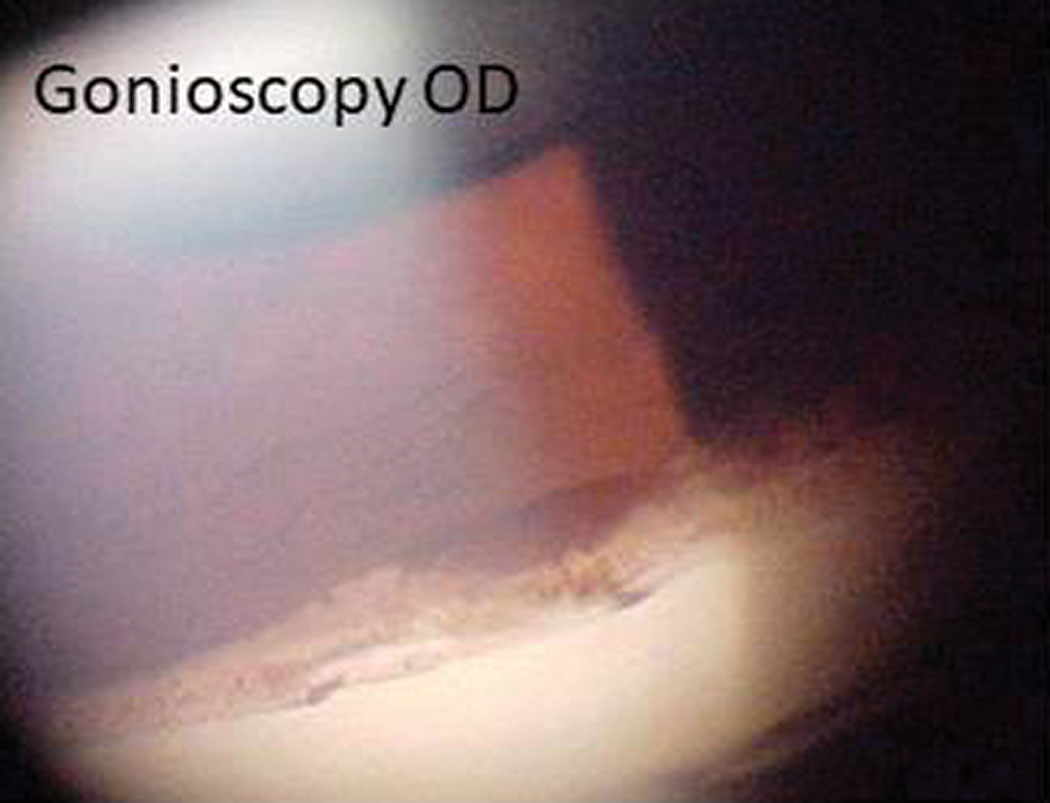
His best-corrected entering visual acuities were 20/20 OD and 20/20 OS at distance and near. Refraction uncovered mild hyperopia with presbyopia measuring +0.50/+1.75 OU. His external examination was unremarkable with no evidence of afferent pupillary defect. His biomicroscopic examination was essentially normal with some pigmentation granules observed on the endothelium, OD. Goldmann applanation tonometry measured 30mm Hg OD and 21mm Hg OS. The pertinent anterior and posterior segment findings are demonstrated in the photographs.
Discussion
Additional studies included color photodocumentation of the discs, central corneal thickness, automated perimetry and optical coherence tomography (OCT) OU to understand the structural and functional status.
The diagnosis in this case is angle recession with secondary open angle glaucoma in the right eye. Patients with angle recession glaucoma are asymptomatic until the glaucomatous disease has advanced to cause profound visual acuity loss, visual field loss or the intraocular pressure (IOP) has become extremely elevated. Even in these cases, pain is rare because the IOP often becomes raised gradually.
Patients with significantly elevated IOP (e.g., greater than 40mm Hg) may become symptomatic with pain and visual disturbances secondary to corneal decompensation. Angle recession glaucoma is more common in younger males, though any patient may develop this condition.1-3
 | |
 | After a little roughhousing injured his eye, a patient’s near vision got progressively worse for three years. Using this history, fundus photos and a gonioscopy exam, can you help identify why he suddenly needs reading glasses? |
Since angle recession does not occur spontaneously, there will be a history of antecedent blunt trauma to the involved eye, often occurring years earlier. In many instances the patient will have either forgotten the event or consider it trivial, such as a minor fall. Sports injuries and assault are the most common causes.4-6 In the case of abuse or assault, the patient may knowingly or unknowingly deny the trauma.6
Other signs of ocular trauma include corneal scars, Descemet’s membrane tears, corneal pigment, corectopia, iridodialysis, phacodonesis and cataract.7 Hyphema is a common comorbidity, with many cases of angle recession glaucoma associated with traumatic hyphema at inception.8-11 The vast majority of patients with traumatic hyphema have some degree of angle recession.5 Traumatic eye injuries can produce angle recession without ever manifesting glaucoma of any kind.
The rise in IOP typically occurs gradually and can be substantial. Interestingly, unexplained IOP rise is seen in 50% of untraumatized fellow eyes, occurring years after the inciting incident.12
Gonioscopically, the clinician will observe a deepening of the angle recess, revealing a larger section of visible ciliary body (excessive gray tissue posterior to the scleral spur). In minor recessions, a disruption of the insertion of the iris into the ciliary body can be seen and the ciliary body will appear more prominently compared with the views in rest of the angle or the angle in fellow eye. In major recessions, the iris root may be torn away, leaving a cleft, which extends into the ciliary body.7
Generally, in angle recession the ciliary body appears wider and the scleral spur appears whiter in the area where it has occurred. It may occur in quadrants or 360 degrees around.7 There may be areas of peripheral anterior synechiae at the lateral edges of the angle recession that obscure the clinician’s view of the total area that has been affected. For these reasons, in cases when gonioscopy is deemed necessary, it is always recommended that clinicians perform it in both eyes. This allows for assessment of both angles as well as inter-eye comparison.
In an angle recession, blunt trauma to the eye forces aqueous laterally and posteriorly within the anterior chamber. This hydrodynamic force produces a tear between the longitudinal and circular muscles of the ciliary body. The longitudinal muscles remain attached to the scleral spur. Frequently, patients develop hyphema at the time of trauma due to tearing of the anterior and posterior ciliary arteries.2,7
Direct damage to the trabecular meshwork may result in ciliary body shutdown at first, resulting lower IOP immediately following the episode. Later, as the ciliary body recovers, normal fluid production is reinstated but, because of drainage insufficiency (blood, inflammation, pigment), the IOP rises.7 In these cases, immediate temporary treatment using topical aqueous suppressants is indicated.
As the inflammation, bleeding and other injury-related factors are resolved, the IOP control can be suspended.
Angle recession does not produce chronically raised IOP with all of its consequences (secondary open angle glaucoma) for quite some time following the initial injury.1,7,13
In angle recession glaucoma, the trabecular meshwork becomes damaged concomitantly with the occurrence of the angle recession. In the beginning, there may not be enough functional compromise to cause outflow dysfunction. It isn’t until there is a natural age-related decline in trabecular function that the true extent of the damage is unmasked as the IOP slowly and relentlessly elevates.
While angle recession following blunt ocular trauma is rather common, only approximately 6% of patients will develop glaucoma.3 The likelihood of developing glaucoma is related to the extent of the angle’s damage. Typically, greater than 180˚ of angle recession will result in glaucoma while less than 180˚ will not.9,14,15
The presence of hyphema at the time of injury greatly increases the risk of late-onset secondary open angle glaucoma either with or without angle recession.2,5,8 The presence of increased trabecular pigmentation, elevated baseline IOP, history of hyphema, lens displacement and recession of more than 180˚ of the angle are significantly associated with the occurrence of late traumatic and angle recession secondary open angle glaucoma.16
Small angle recessions can heal without sequelae. More significant injuries have associated degenerative atrophy, fibrosis and scarring of the trabecular meshwork and Schlemm’s canal. There can be obliteration of the intertrabecular spaces with or without closure of Schlemm’s canal years after injury with hyaline membrane development over the inner trabecular meshwork.7 As the outflow facility naturally decreases, the IOP may begin to rise.
The recession of the angle itself does not cause IOP elevation. Rather, widespread damage to the trabecular meshwork with the long-term changes seems to be the cause. Hence, the trabecular meshwork is not just damaged in the area of the visible recession but likely is damaged in a much larger portion that is either not visible or internal.
First-aid requires glaucoma medications that reduce aqueous production such as beta blockers, alpha-2 adrenergic agonists and carbonic anhydrase inhibitors. As the genesis of the glaucoma seen in angle recession is severe trabecular meshwork dysfunction, miotics are ineffective due to the disruption of the ciliary muscle-scleral spur dynamic.13 For this reason, laser trabeculoplasty is likewise ineffective.17-19 Prostaglandin analogs, which increase aqueous outflow through the uveoscleral meshwork, offer an excellent alternative for egress and can be very effective in IOP reduction in the cases that evolve into the chronic condition.7
In cases of recent trauma involving angle recession, vitreous hemorrhage and severe IOP elevation, combined trabeculectomy and vitrectomy is a viable surgical option with no incidence of recurrent vitreous hemorrhage or retinal detachment.20 Overall, trabeculectomy demonstrates a lower success rate in angle recession glaucoma compared to primary open angle glaucoma. Bleb fibrosis forms earlier and more significantly in cases with angle recession.21 For this reason, the use of antifibrolytic agents (e.g., mitomycin, 5-FU) are desirable in conjunction with trabeculectomy.22 Setons may also offer an alternative to cases requiring significant revision.
Remember these seven take-home points with regard to angle recession glaucoma:
- Open-angle glaucoma is generally a symmetric disease. In cases of unilateral or asymmetric glaucoma, inquire about a history of trauma.
- When performing gonioscopy, angle recession can best be identified by comparing two sections of the angle in one eye or by switching eyes.
- If there is 360˚ of angle recession, fellow-eye comparison will also help. That is why the procedure should always be done in both eyes.
- IOP levels in angle recession glaucoma can be quite dramatic. IOP exceeding 70mm Hg is possible.
- The IOP may take years to rise years after trauma. For this reason, patients with angle recession must be followed closely for their entire lives.
- Angle recession glaucoma may be an antiquated term; traumatic secondary open-angle glaucoma with angle recession may be a better term.
- Gonioscopy is never indicated immediately after blunt trauma, as it only adds to the patient’s discomfort, has the potential to dislodge a clotted hyphema (causing rebleeding) and serves no purpose toward the rendering of acute management. The examination can be completed after the sequelae of the blunt force injury have resolved.
Dr. Gurwood thanks Joe Sowka, OD, for his contributions to this column.
1. Ellong A, Ebana Mvogo C, Nyouma Moune E, et al. Post-traumatic glaucoma with irido-corneal angle injuries in Cameroon. Bull Soc Belge Ophtalmol. 2005;(298):21-8. 2. Jan S, Khan S, Mohammad S. Hyphaema due to blunt trauma. J Coll Physicians Surg Pak. 2003;13(7):398-401. 3. Salmon JF, Mermoud A, Ivey A, et al. The detection of post-traumatic angle recession by gonioscopy in a population-based glaucoma survey. Ophthalmology. 1994;101(11):1844-50. 4. Canavan YM, Archer DB. Anterior segment consequences of blunt ocular injury. Br J Ophthalmol 1982;66:549-55. 5. Filipe JA, Barros H, Castro-Correia J. Sports-related ocular injuries. A three-year follow-up study. Ophthalmology 1997;104(2):313-8. 6. Mermoud A, Salmon JF, Barron A, et al. Surgical management of post-traumatic angle recession glaucoma. Ophthalmology. 1993;100(5):634-42. 7. Tumbocon JA, Latina MA. Angle recession glaucoma. Int Ophthalmol Clin. 2002;42(3):69-78. 8. Girkin CA, McGwin G Jr, Long C, et al. Glaucoma after ocular contusion: a cohort study of the United States Eye Injury Registry. J Glaucoma. 2005;14(6):470-3. 9. Viestenz A, Kuchle M. Blunt ocular trauma. Part I: blunt anterior segment trauma. Ophthalmologe. 2004;101(12):1239-57. 10. Mortensen KK. Changes in anterior chamber depth and angle-recession, late complications to ocular contusion. Acta Ophthalmol (Copenh). 1978;56(6):876-82. 11. Herschler J. Trabecular damage due to blunt anterior segment injury and its relationship to traumatic glaucoma. Trans Sect Ophthalmol Am Acad Ophthalmol Otolaryngol. 1977;83(2):239-48. 12. Tesluk GC, Spaeth GL. The occurrence of primary open angle glaucoma in the fellow eye of patients with unilateral angle cleavage glaucoma. Ophthalmology 1985;92(7):904-11. 13. Pilger IS, Khwarg SG. Angle recession glaucoma: review and two case reports. Ann Ophthalmol. 1985;17(3):197-9. 14. Charfi Ben Ammar O, Chaker N, Soukah M, et al. Posttraumatic glaucoma. J Fr Ophtalmol. 2002;25(2):126-9. 15. Sihota R, Sood NN, Agarwal HC. Traumatic glaucoma. Acta Ophthalmol Scand. 1995;73(3):252-4. 16. Sihota R, Kumar S, Gupta V, et al. Early predictors of traumatic glaucoma after closed globe injury: trabecular pigmentation, widened angle recess, and higher baseline intraocular pressure. Arch Ophthalmol. 2008;126(7):921-6. 17. Goldberg I. Argon laser trabeculoplasty and the open-angle glaucomas. Aust N Z J Ophthalmol. 1985;13(3):243-8. 18. Lieberman MF, Hoskins HD Jr, Hetherington J Jr. Laser trabeculoplasty and the glaucomas. Ophthalmology. 1983;90(7):790-5. 19. Robin AL, Pollack IP. Argon laser trabeculoplasty in secondary forms of open-angle glaucoma. Arch Ophthalmol. 1983;101(3):382-4. 20. Wang XY, Hu RR, Shen LP, et al. Combined trabeculectomy and vitrectomy for intractable glaucoma with severe ocular contusion involving the posterior segment. Chin Med J (Engl). 2011;124(15):2316-20. 21. Mermoud A, Salmon JF, Straker C, et al. Post-traumatic angle recession glaucoma: a risk factor for bleb failure after trabeculectomy. Br J Ophthalmol. 1993;77(10):631-4. Manners T, Salmon JF, Barron A, et al. Trabeculectomy with mitomycin C in the treatment of post-traumatic angle recession glaucoma. Br J Ophthalmol. 2001;85(2):159-63. |

