 |
Q:
A keratoconus (KCN) patient of mine just passed away from myocardial infarction. A relative said she read that KCN patients are at a higher risk of cardiac problems. Is this the case or are there too many confounders to draw any conclusions?
A:
“KCN—a progressive ectatic disorder that causes thinning and steepening of the cornea—is a multifactorial disease with environmental, biomechanical and genetic factors,” says Katelyn Lucas, OD, of Price Vision Group in Indianapolis.
Dr. Lucas notes that while many diseases associated with KCN have an increased risk for cardiovascular comorbidities, a direct link between cardiac issues and KCN has not been found. She adds, however, that since KCN prevalence is listed as 1/2000 in some textbooks and between 1% and 5% of patients undergoing screening for refractive surgery show possible signs of KCN, it is not unusual to find KCN patients with almost any disease.1 Understanding the many risk factors that have been associated with KCN can be beneficial, she suggests.
Risk Factors
Eye rubbing is highly associated with the progression of KCN due to repetitive mechanical trauma that induces stress on corneal structures, in turn weakening and warping the cornea.2,3 Dr. Lucas recommends patient education, topical antihistamines and other allergy drops to mitigate the effects and help break the cycle of eye rubbing.
 |
|
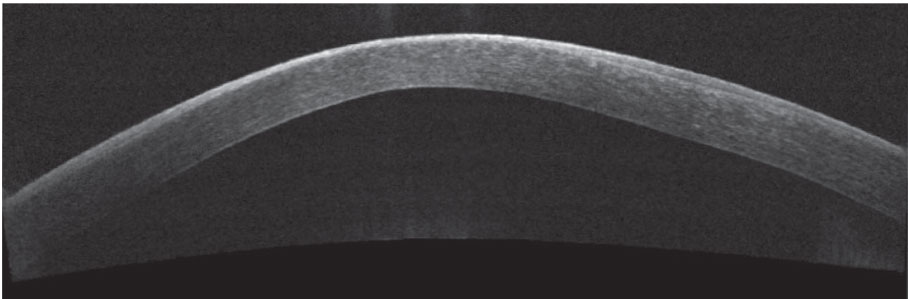
Corneal thinning and bulging are characteristic of KCN. Click image to enlarge. |
KCN is associated with various genetic conditions, including Leber’s congenital amaurosis (LCA) and Down syndrome, according to Dr. Lucas. She says eye rubbing is commonly seen in LCA and is believed to cause KCN in these patients. Patients with Down syndrome are six times more likely to develop KCN and are known to frequently rub their eyes due to atopy or allergy.4 A genetic variation in Down syndrome may affect collagen fibers and cause alterations in the cornea.5
Connective tissue disorders, such as Ehlers-Danlos syndrome (EDS), are linked to KCN, says Dr. Lucas. She notes that classic EDS is a type V collagen disorder, and the cornea is rich in type V collagen, making it a targeted tissue. She adds that brittle cornea syndrome is a type of EDS associated with steeper and thinner corneas that often result in KCN.
Obstructive sleep apnea (OSA) is more prevalent in KCN patients, and high-risk OSA patients are more likely to have more severe KCN.4 Dr. Lucas recommends screening for OSA in KCN patients due to its increased risk of morbidity and mortality.
Treatment Options
Most cases of KCN respond well to glasses and contact lenses, and in severe cases, specialty contact lenses provide excellent vision and comfort, Dr. Lucas says. When the cornea becomes too scarred or distorted for functional vision with contact lenses, however, she says a transplant is needed.
Traditionally, full-thickness transplants are performed for KCN. However, penetrating keratoplasties have a risk of rupture with minor trauma, unpredictable visual recovery and a limited lifetime, as corneal endothelial cells decrease over time, especially in grafted tissue.
Dr. Lucas suggests a deep anterior lamellar keratoplasty to preserve the patient’s own endothelium. This procedure decreases the risk of rejection, lowers the need for long-term steroid use, lasts longer and uses larger-diameter grafts.6
According to Dr. Lucas, crosslinking is the only treatment to slow or prevent KCN progression.
KCN is associated with systemic diseases, but there’s no evidence suggesting it’s linked to cardiac issues.
1. Nesburn AB, Bahri S, Salz J, et al., Keratoconus detected by videokeratography in candidates for photorefractive keratectomy. J Refract Surg. 1995;11(3):194-201. 2. Moran S, Gomez L, Zuber K, et al. A case-control study of keratoconus risk factors. Cornea. 2020;39(6):697-701. 3. Mazharian A, Panthier C, Courtin R, et al. Incorrect sleeping position and eye rubbing in patients with unilateral or highly asymmetric keratoconus: a case-control study. Cornea. June 10, 2020. [Epub ahead of print]. 4. Woodward MA, Blachley TS, Stein JD. The association between sociodemographic factors, common systemic diseases, and keratoconus: an analysis of a nationwide healthcare claims database. Ophthalmology. 2016;123(3):457-65. 5. Alio JL, Vega-Estrada A, Sanz P, et al. Corneal morphologic characteristics in patients with Down syndrome. JAMA Ophthalmol. 2018;136(9):971-8. 6. Nanavaty MA, Singh Vijjan K, Yvon C. Deep anterior lamellar keratoplasty: a surgeon’s guide. J Curr Ophthalmol. 2018;30(4):297-310. |

