During every comprehensive eye examination, perusing the patient’s medical history is a crucial first step, even when they present without any visual complaints. Many of our patients are being treated for a systemic condition, and either the disease itself or its treatment regimen—or both—could come with ocular manifestations the patient may not be aware of.
While the more common systemic issues become second nature (think diabetes), other details in the medical chart are easily overlooked because they may not immediately seem related to the eyes. When we notice these less-obvious flags in the medical history or during the review of systems, we should adjust our approach to ensure we are looking more closely for the (sometimes subtle) ocular associations. Even when the subsequent exam shows that the ocular system remains unaffected, we should ensure our patients are acquainted with the possible systemic and ocular manifestations that they need to watch for.
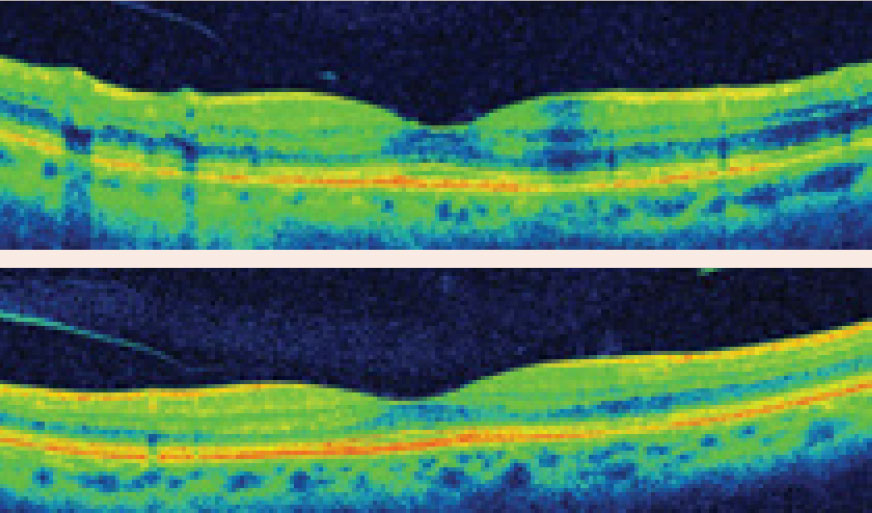
 |
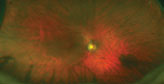
| This patient had a Hollenhorst plaque in the superior-temporal arcade of each eye and a cotton-wool spot inferior-temporal to the right optic nerve. He had 70% to 99% stenosis of the right carotid artery and insignificant disease on the left. His echocardiogram was unremarkable. He underwent right carotid endarterectomy. Click image to enlarge. |
Cardiovascular & Cerebrovascular Disorders
This includes the common metabolic trifecta: diabetes, hypertension and hyperlipidemia. These are so routine in my daily practice that it’s almost surprising when patients don’t have at least one of them, but their ever-increasing frequency doesn’t negate their importance. Every optometrist should already be well-versed in caring for patients with these comorbidities.
However, many other pertinent cardiovascular abnormalities might show up in your patient’s medical record and give you pause. It’s important that you educate these patients about cardiovascular optimization, including smoking cessation, and symptoms warranting emergency evaluation. Here are four of the more common ones:
Cerebral arteriovenous malformations (AVMs). These are a complex knot of directly fistulating arteries and veins, without a normal capillary bed in between. They can hemorrhage and cause significant morbidity and mortality associated with hemorrhagic stroke (cerebrovascular accident, CVA); in fact, they account for 2% of all hemorrhagic strokes.1
AVMs in or near the visual pathway can cause visual field defects associated with both mass effect from the AVM itself or from its bleeding, or from ischemia related to stroke. Occipital AVMs can cause headaches and visual symptoms similar to migraine auras. Brainstem AVMs may produce diplopia, abnormal extraocular function (cranial nerve III palsy, gaze palsy) and pupil abnormalities (anisocoria, light-near dissociation).2 As congenital malformations, these predominantly affect younger and otherwise healthy patients.1
- Think of: stroke.
- Look for: visual field changes.
- Educate patients about: transient ischemic attack (TIA)/CVA symptoms, aura-like symptoms, visual field changes, headaches, diplopia and other neuro-ophthalmic findings.
Right the RecordUnless you work in a multidisciplinary hospital setting or integrated healthcare system, you may not have access to the patient’s entire medical record, and you must instead rely on the patient’s memory. Unfortunately, patients are often terrible historians. They may know their medications, but not their medical conditions/history—or vise versa. We all have those patients who say they don’t have hypertension because it’s controlled with medication, right? Thus, we have to sleuth out the diagnosis based on the medication prescribed, or the likely medication based on the diagnosis. In addition to hypotensives, here are two more examples: Levothyroxine. Think of underactive thyroid function, which may be due to a host of issues (autoimmunity, thyroiditis, etc.), including iatrogenic causes such as surgical removal of the thyroid or radioactive iodine treatment for hyperthyroidism. In patients on this thyroid hormone replacement with a history of hyperthyroidism/Grave’s disease, look for (most commonly) ocular surface exposure and EOM dysfunction and educate your patients about dryness and double vision as possible ocular manifestations of thyroid eye disease. Anticoagulants. Think AFib (though they are used for other indications as well), look for and educate patients about ocular cardiovascular-associated sequala and education the patient on possible complications of AFib such as stroke, mini-stroke, TMVL or subconjunctival hemorrhages from the drug’s use. |
Carotid artery stenosis or occlusion. Atheromatous plaques along the carotid arteries can lead to insufficient blood flow from the internal carotid to the ophthalmic and ultimately to both the inner retinal arterial and choroidal supply, which can also lead to general ocular ischemia (think hypoperfusion retinopathy, which can lead to ocular ischemic syndrome). These carotid atheromatous plaques can also ulcerate and lead to embolic strokes—both cerebral or intraocular (Hollenhorst plaques, which may cause retinal artery occlusions).
Optometrists must remember to educate patients on transient monocular vision loss (TMVL, also known as amaurosis fugax), particularly for these patients. This indicates transient ischemia to the eye and qualifies as a TIA, which should warrant emergency medical evaluation and stroke workup. Remember that the patient’s highest risk of having a CVA is within 48 hours of a TIA, so TIA/CVA symptoms (including TMVL) should be reviewed regularly with patients who are at increased risk.
Atrial fibrillation (AFib). When the atria fibrillate, they do not pump normally; instead, blood pools, putting patients at a higher risk of clotting. This can cause thromboembolic vascular occlusions (ophthalmic, cerebral), which can occur even when the patient is anticoagulated. TIA/CVA/TMVL warnings are also pertinent in these patients.
Valvular heart disease. Calcific stenosis of the mitral or aortic valves can produce embolic artery occlusions, and prolapse of these valves can lead to thromboembolic occlusions.
- Think about: ischemia, TIA/CVA/TMVL.
- Look for: ischemic anterior segment findings (neovascularization); retinopathy (micro-aneurysms, intraretinal hemorrhages, cotton-wool spots, neovascularization); vascular occlusions (embolic, thromboembolic); neurologic manifestations (non-arteritic ischemic optic neuropathy (NAION), cranial nerve palsies, TIA/CVA).
- Educate patients about: TIA/CVA/TMVL, diplopia, vision/visual field loss.
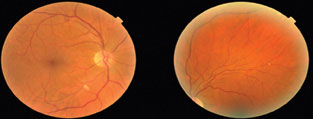
 |
| Papilledema may be seen in patients who have sleep apnea. Photo: Brad Sutton, OD. Click image to enlarge. |
Obstructive Sleep Apnea
While this systemic condition certainly carries a higher risk of systemic morbidity and mortality related to hypoxia, it’s also associated with ocular morbidity. Eye care providers often think only of floppy eyelid syndrome and dry eyes; however, though less common, several other ocular conditions are associated with obstructive sleep apnea (OSA), including NAION, primary open angle- and normal-tension glaucoma, retinal vein occlusions (RVOs) and central serous chorioretinopathy (CSCR).3,4
While the absolute risk of these ocular conditions is low, the relative risk is higher in OSA patients than it is in the general population.3 Mechanical changes related to connective tissue weakness and vascular mechanisms related to hypoxia and impaired autoregulation of blood flow are all associated with OSA and these ocular manifestations.4
- Think about: floppy eyelid syndrome, dry eye, glaucoma, RVOs, CSCR.
- Look for: lid laxity, ocular surface/dry eye findings; optic disc edema or pallor; subfoveal fluid; retinal hemorrhaging, venous dilation or occlusion.
- Educate patients about: dry eye symptoms, acute vision/visual field loss, metamorphopsia.
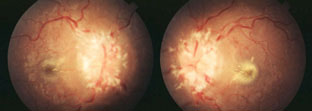
 |
| BCC of the upper eyelid, at left and the medial chanthus/nasal root, at right. Note the lesions’ pearly elevated margins. Click image to enlarge. |
Hematologic Disorders
Several conditions that affect the blood can have significant ocular manifestations:
Blood cancers. Leukemia can cause subconjunctival hemorrhages or retinopathy that appears similar to other common types of retinopathy (hypertensive, diabetic, ocular ischemic) with findings such as venous tortuosity and dilation, intraretinal hemorrhages, cotton-wool spots and Roth spots.
Hyperviscosity leading to RVOs is also possible. Ocular findings are present in up to 90% of patients with leukemia.5
Lymphoma, a remarkable masquerader, can affect any compartment of the eye, including the eyelids, ocular surface, lacrimal gland, any part of the uvea, vitreous, retina or even can infiltrate the optic nerve or orbit.
Monoclonal gammopathies indicate an overproduction of plasma cell immunoglobins. Monoclonal gammopathies of undetermined significance (MGUS) are seen in 3% to 4% of adults older than age 50 and are considered premalignant because they can progress with a 1% annual risk of progression to myeloma.6 Like lymphomas, MGUS and myeloma can affect nearly any part of the eye either by direct infiltration or related to the consequences of hematologic imbalance (hyperviscosity).
Deep stromal deposits of monoclonal proteins, crystalline keratopathy or copper deposits in Descemet’s membrane, maculopathy, vitritis, vasculitis and findings associated with relative hyperviscosity have been reported with MGUS.7-9 Similarly, myeoma can present as infiltration or deposition in various structures or solid plasmacytomas (plasma cell tumors). As with leukemias, hyperviscosity-related retinopathy can develop, and similar to lymphoma, myelomatous infiltration can occur throughout the eye and related structures.
- Think about: infiltration, hyperviscosity, masqueraders.
- Look for: lesions anywhere or indication of orbital lesions, deposition or infiltration, uveitis, retinopathy.
- Educate patients about: visible lesions in or around the eye, floaters, eye pain, diplopia, TIA/CVA/TMVL (hyperviscosity), visual/visual field changes.
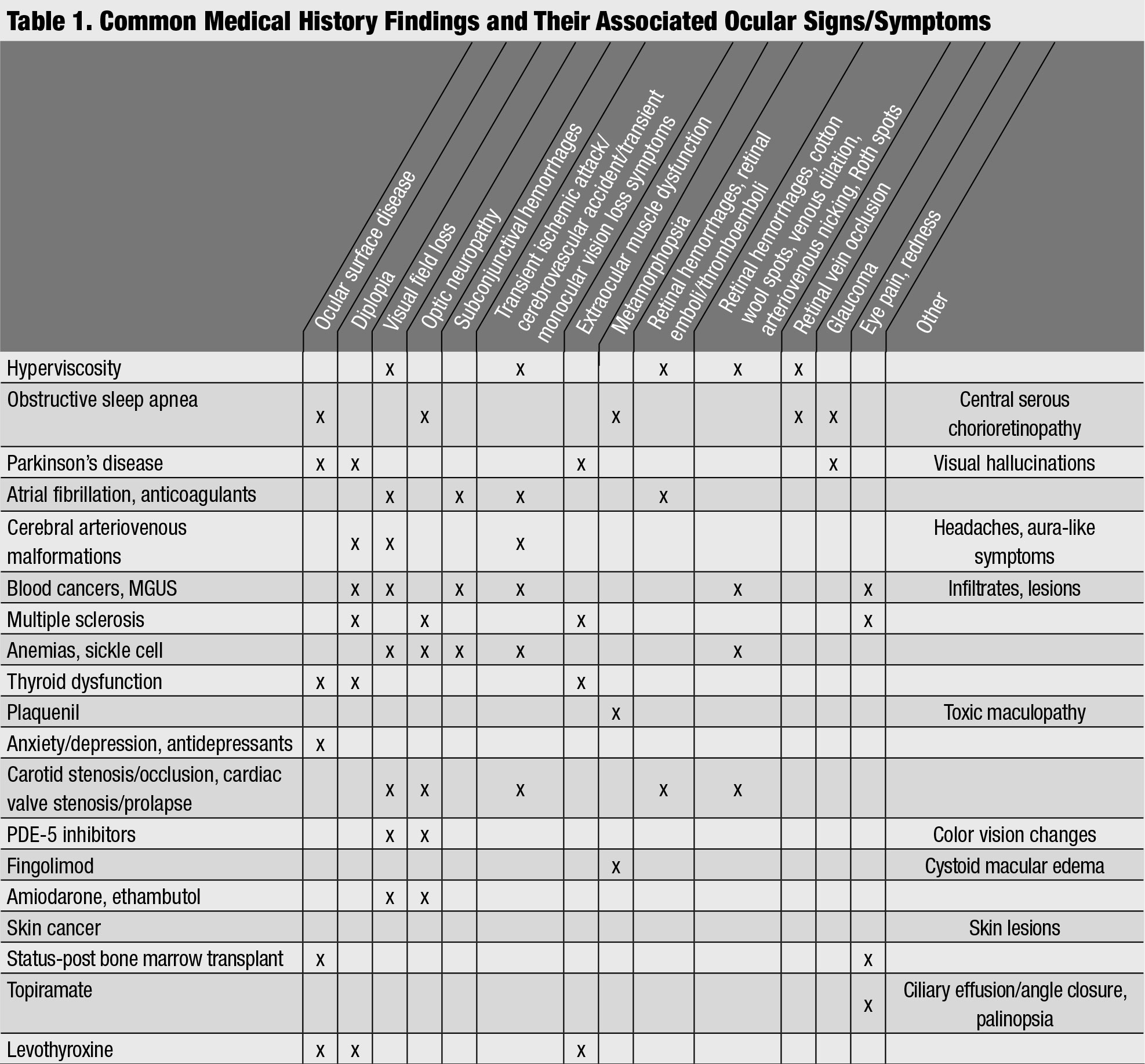 |
| Common Medical History Findings and Their Associated Ocular Signs/Symptoms. Click table to enlarge. |
Status-post bone marrow transplant (BMT). Patients may undergo BMT for a variety of hematologic malignancies. If the patient receives allogenic bone marrow from a donor (rather than allogenic marrow), there is risk for the development of graft-vs.-host disease (GVHD).10 Patients undergo conditioning to eradicate both tumor and host marrow cells prior to BMT, and this may include total body irradiation; those having had irradiation may also develop cataract.10 GVHD can present acutely with a hemorrhagic pseudomembranous conjunctivitis, and chronically may appear as a significant autoimmune, Sjögren-like keratoconjunctivitis sicca with lacrimal gland findings, ocular surface and corneal findings and cicatricial scarring.10
- Think about: GVHD, cataract.
- Look for: keratoconjunctivitis sicca, corneal stromal infiltrates, pseudomembranous conjunctivitis, cicatricial changes to eyelids and conjunctiva, cataract.
- Educate patients about: Blurry vision, dry eye symptoms.
Anemias. These indicate a reduced level of red blood cells (RBCs) or hemoglobin; while iron deficiency anemia is most common, other forms are possible, such as pernicious anemia (vitamin B12 deficiency), aplastic anemia (inadequate RBC production) or hemolytic anemia (increased RBC destruction).11 Anemia may lead to bleeding in or around the eye, such as subconjunctival hemorrhage, and retinopathy similar to that seen in leukemia.12 Pernicious anemia can lead to optic atrophy, which is seen as disc pallor.
Sickle cell. This genetic disorder causes RBCs to take on a sickle- or crescent-shaped morphology, which can lead to microvascular occlusion and local ischemia. In the eye, this may be seen as non-proliferative or proliferative retinopathy.11
- Think about: bleeding, ischemia, retinopathy, optic neuropathy.
- Look for: hemorrhaging, ischemia, retinopathy, disc pallor.
- Educate patients about: abnormal bleeding/bruising, changes in vision.
 |
| This patient has a history of hairy cell leukemia and has had leukemic retinopathy for a number of years. |
 |
| Click images to enlarge. |
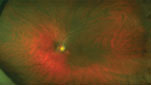 |
| He later developed a hemi-retinal vein occlusion in the right eye. |
Skin Cancers
These are common and often will crop up on the head and neck. A patient’s history of skin cancer should alert clinicians to screen for new concerning spots. Of all head/neck basal cell carcinomas (BCCs), 20% are periocular.13 Squamous cell carcinomas (SCC) are second to BCC for eyelid malignancies, and melanoma and other malignancies can also present around the eye.13 Patients should engage in regular self-monitoring and dermatologic evaluations to screen for potentially cancerous lesions, and optometrists are charged with monitoring not just the periorbital region, but any skin in sight.
- Think about: new cancerous or pre-cancerous lesions.
- Look for: pearly raised lesions (BCC), raised keratin patches or ulcerated lesions (SCC), irregular, asymmetric pigmented lesions (melanoma) or other suspicious lesions.
- Educate patients about: any new, symptomatic (itchy, scaly, etc.) or irregular skin lesions.
Medications to Watch ForHydroxychloroquine
Fingolimod
Topiramate
Amiodarone
Ethambutol
PDE5 Inhibitors
Antidepressants
|
Parkinson’s Disease
This is known to have many ocular and visual manifestations. Due to motor slowing, incomplete and delayed blink and lagophthalmos are common, along with a reduction in tear secretion, which all lead to dry eyes and exposure keratopathy. Dry eyes are seen in up to 60% of Parkinson’s disease (PD) patients.14 Given the slow progression, it’s not uncommon for PD patients to present with significant signs but few symptoms.
Visual hallucinations are a frequent symptom, occurring in 16% to 40% of PD patients, and up to 88% of PD patients who have dementia.15 Visuospatial and visuoperceptual impairment also commonly develop as PD progresses. Clinical experience suggests PD patients by-and-large aren’t informed that these things can, and likely will, happen to them, and many don’t report these symptoms unless specifically asked. Uncovering these symptoms is important not only because it’s treatable—with donepezil, for example, for visual hallucinations, or with neurorehabilitation—but also because it helps predict prognosis.16
Abnormal saccades, pursuits and extraocular movements are common, as is diplopia, particularly related to convergence insufficiency.14 Additionally, research suggests an increased incidence of open-angle glaucoma and non-glaucomatous retinal nerve fiber (RNFL) thinning in PD patients.14
Carbidopa-levodopa is a common first-line agent for PD and its presence in the medical history will clue you in to PD as a diagnosis.
- Think about: ocular surface disease, extraocular muscle abnormalities, visuospatial/visuoperceptual abnormalities and visual hallucinations, glaucoma and/or non-glaucomatous RNFL thinning.
- Look for: lid and blink changes, lagophthalmos, dry eye and exposure keratopathy, glaucoma, RNFL thinning.
- Educate patients about: dry eye symptoms, visuospatial/visuoperceptual symptoms, diplopia, visual hallucinations.
 |
| This patient is s/p BMT and has GVHD with symblepharon formation. Click image to enlarge. |
Depression and Anxiety
The link between the eye and these mental health concerns is not as obvious, but several studies have identified an association between depression, anxiety and antidepressant use and an increase in the prevalence of dry eye disease and subjective dry eye symptoms.17,18 While objective findings are often lacking, these patients can be quite symptomatic. In addition to treating their ocular symptoms with dry eye therapies, be sure to support and encourage mental health care.
- Think about: dry eye symptoms, which often outweigh signs.
- Look for: ocular surface disease.
- Educate your patient about: dry eye symptoms, appropriate mental health care.
The conditions reviewed here are just a small sampling of the many things we see in our patient’s medical record that should get our optometry wheels turning. Almost any systemic revelation can connect back to the eyes in some way. It’s important that we embrace whole-body care to help our patients stay healthy and happy.
Dr. Weidmayer practices at the VA Ann Arbor Healthcare System in Ann Arbor, MI.
1. Hernesniemi JA, Dashti R, Juvela S, et al. Natural history of brain arteriovenous malformations: a long-term follow-up study of risk of hemorrhage in 238 patients. Neurosurgery. 2008;63(5):823-31. 2. American Academy of Ophthalmol. Arteriovenous Malformations. www.aao.org/bcscsnippetdetail.aspx?id=2a0d8631-c747-4fc5-bb4d-cbd2329c121a. Accessed November 19, 2019. 3. Yang HK, Park SJ, Byun SJ, et al. Obstructive sleep apnoea and increased risk of non-arteritic anterior ischaemic optic neuropathy. Br J Ophthalmol. 2019;103(8):1123-28. 4. Santos M, Hofmann RJ. Ocular manifestations of obstructive sleep apnea. J Clin Sleep Med. 2017;13(11):1345-48. 5. Talcott KE, Garg RJ, Garg SJ. Ophthalmic manifestations of leukemia. Curr Opin Ophthalmol. 2016;27(6):545-51. 6. Rajkumar SV, Dimopoulos MA, Palumbo A. International Myeloma Working Group updated criteria for the diagnosis of multiple myeloma. Lancet Oncol. 2014;15:e538-48. 7. Karakus S, Gottsch JD, Caturegli P, Eghraria AO. Monoclonal gammopathy of “ocular” significance. Am J Ophthalmol Case Rep. 2019;15:100471. 8. Balderman SR, Lichtman MA. Unusual manifestations of monoclonal gammopathy: I. ocular disease. Rambam Maimonides Med J. 2015;6(3):e0026. 9. Chan TYB. Vitritis and retinal vasculitis as presenting signs of monoclonal gammopathy of unknown significance with progression to multiple myeloma. Can J Ophthalmol. 2010;45:82-3. 10. Bray LC, Carey PJ, Proctor SJ, et al. Ocular complications of bone marrow transplantation. Br J Ophthalmol. 1991;75:611-14. 11. Reynolds SA, Rodman J. Hematological disorders and the retina. Rev Optom. 2009;146(9). 12. Tarlan B, Kiratli H. Subconjunctival hemorrhage: risk factors and potential indicators. Clin Ophthalmol. 2013;7:1163-70. 13. Silverman N, Shinder R. What’s new in eyelid tumors. Asia-Pac J Ophthalmol. 2017;6(2):143-52. 14. Ekker MS, Janssen S, Seppi K, et al. Ocular and visual disorders in Parkinson’s disease: Common but frequently overlooked. Parkinsonism Relat Disord. 2017 Jul;40:1-10. 15. Kurita A, Koshikawa H, Akiba T, et al. Visual hallucinations and impaired conscious visual perception in Parkinson disease. J Geri Psych Neur. December 6, 2019. [Epub ahead of print]. 16. Kurita A, Ochiai Y, Kono Y, et al. The beneficial effect of donepezil on visual hallucinations in three patients with Parkinson’s disease. J Geriatr Psychiatry Neurol. 2003;16(3):184-8. 17. Van der Vaart R, Weaver MA, Lefebvre C, Davis RM. The association between dry eye disease and depression and anxiety in a large population-based study. Am J Ophthalmol. 2015;159(3):470–474. 18. Kitazawa M, Sakamoto C, Yoshimura M, et al. The relationship of dry eye disease with depression and anxiety: a naturalistic observational study. Transl Vis Sci Technol. 2018;7(6):35. |