 |
 |
While cataract surgery alone can lower IOP, more advanced glaucoma patients need more aggressive IOP lowering.1 Combining minimally invasive glaucoma surgeries and cataract surgery can potentially provide this, and a greater safety profile than traditional filtration surgeries.
iStent
The insertion of a single stent and, at times, multiple stents (although not FDA approved) through the same corneal incision used during cataract surgery serves as a bypass through the trabecular meshwork. This allows greater physiological outflow and, therefore, lower IOP. A study revealed that 66% of eyes treated with cataract surgery and a glaucoma stent achieved a greater than 20% reduction in IOP without medications vs. 48% of eyes treated with cataract surgery alone.2 In addition, the overall safety profile was similar to cataract surgery alone.2,3
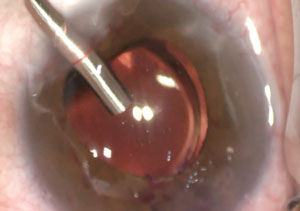 | |
| After iStent implantation, the surgeon inserts the ECP probe for the final step. |
Endocyclophotocoagulation
ECP uses a diode laser and video imaging integrated into a fiber-optic system delivered through a probe to ablate the ciliary body processes. The coagulation and scarring of the ciliary body processes leads to a decrease in aqueous production, resulting in a reduction in IOP. A study revealed patients who underwent either phacoemulsification alone or phacoemulsification combined with ECP showed greater benefit in the combined group with no increased risk of complications.4
Advantages
These surgeries complement each other well and address both inflow and outflow of aqueous. Patients with mild to moderate open-angle glaucoma and a cataract who are using multiple IOP-lowering medications are generally ideal candidates. Patient satisfaction can be high with ICE, as no external sutures, common with trabeculectomies, are placed and postoperative visual recovery is rapid. ICE also carries no risk of bleb-related infections or bleb leaks.
Postoperative Care
Postoperatively, ICE is managed with a typical post-cataract regimen of topical steroid, NSAID, plus a topical antibiotic for prophylaxis. IOP may fluctuate due to steroid use and viscoelastic issues. As IOP improves and stabilizes, the patient may reduce their dependence on glaucoma drops. The emergence of antibiotic-steroid injections, such as TriMoxiVanc/TriMoxi, is another option some eye care centers use. The injection of this combination medication can help avoid the postoperative inflammation common with ECP.
Dr. Schweitzer is a cornea, glaucoma, cataract and refractive surgery specialist at Vance Thompson Vision in Sioux Falls, SD.
1. Augustinu CJ, Zeyen T. The effect of phacoemulsification and combined phace/glaucoma procedures on the intraocular pressure in open-angle glaucoma. A review of the literature. Bull Soc Belge Ophtalmol. 2012;320:51-66.2. Samuelson TW, Katz L, Wells J, et al. Randomized evaluation of the trabecular micro-bypass stent with phacoemulsification in patients with glaucoma and cataract. Ophthalmology. 2011;118(3):459-67.
3. Fea AM. Phacoemulsification versus phacoemulsification with micro-bypass stent implantation in primary open-angle glaucoma: randomized double-masked clinical trial. J Cataract Refract Surg. 2010;36(3):407-12.
4. Berke SJ, Sturm RT, Caronia RM, et al. Phacoemulsification combined with endoscopic cyclophotocoagulation (ECP) in the management of cataract and medically controlled glaucoma: A large, long term study American Glaucoma Society 16th Annual Meeting. Charleston, SC. 2006 Mar 2-5. Abstract 22:47.

