Dry eye disease (DED) can be frustrating for both the patient, living with pain, and the optometrist, who has to dig for the precise pathogenesis of their patient’s symptoms to best target treatment. That diagnostic process can be costly and time-consuming. Every day the patient spends with burning dry eyes is a day they consider seeing a different optometrist. That’s why it’s vital to have an armamentarium replete with the most up-to-date technologies and techniques to deliver the relief your patients are seeking.
Luckily, optometrists—with a dose of patient cooperation—can handle most of these cases thanks to their clinical acumen as well as several innovative in-office procedures and at-home therapies that patients can be taught to apply. These therapies can be particularly accessible when DED is connected to an underlying disease.
The process begins with a clinical evaluation of the patient to help identify the precise lid disease causing their dryness. Second, the doctor must decide on a treatment protocol to address that underlying issue. Finally, the doctor should educate the patient on an effective management plan that makes use of the technologies and products available to them.
This article provides a guide through those three steps with a focus on lid disease treatment options that the OD can provide in-office, or that a patient can bring home to manage their own condition with optometric oversight.
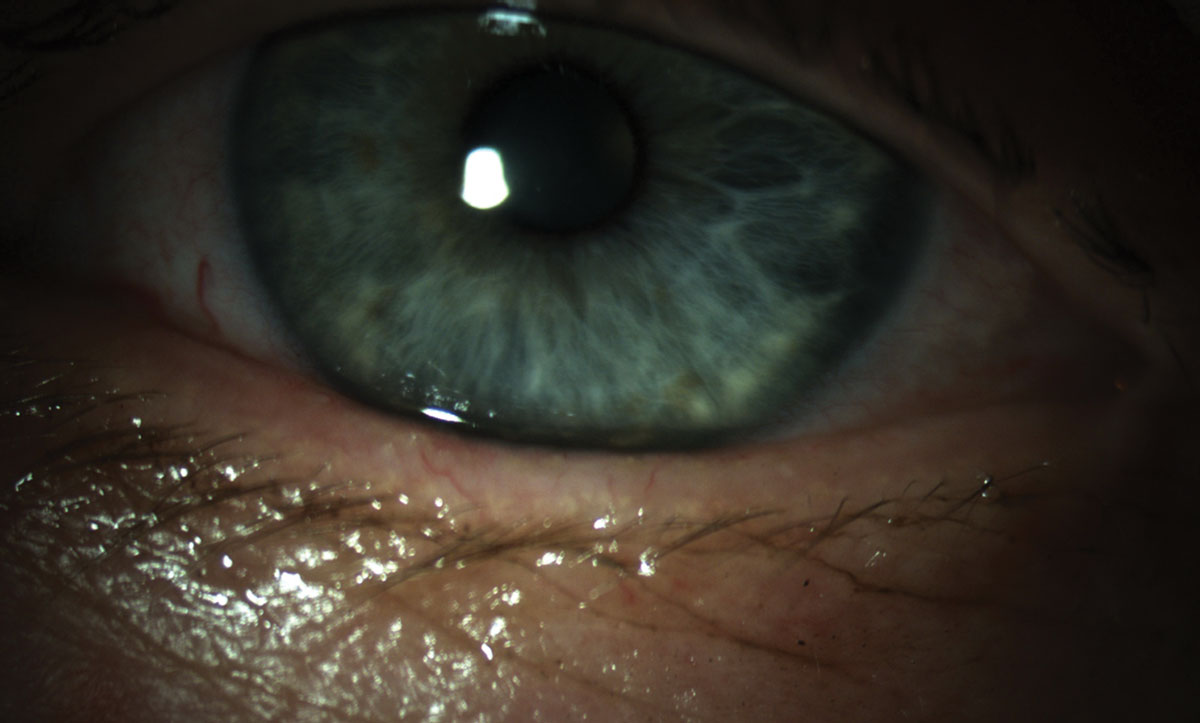 |
| Telangiectasias can be evidence of inflammation at the lid margin. Click image to enlarge. |
Identification
Any suspicion of lid disease is a good reason to evaluate the patient at the slit lamp. Note the apposition of the eyelid to the globe, presence or absence of lid debris and telangiectastias. Additionally, expressing the meibomian glands demonstrates the quality and quantity of the meibum being secreted.
Eyelid laxity can occur due to aging, eye rubbing, hyperelasticity, inflammation or blepharochalasis.1 Patients may experience symptoms such as foreign body sensation, photophobia or irritation. Poor lid apposition may cause lagophthalmos with resultant inferior corneal superficial punctate keratitis. Additionally, an increase in lid laxity can negatively affect blink performance, which is critical for providing and distributing meibum into the tear film. Laxity can easily be evaluated by the “snap” test. In this examination technique, the patient’s lid is lowered and quickly released under the slit lamp. The speed of recovery, or rebound, is noted and subjectively compared with normal.2
Also, be sure to note any lid debris residing at or near the lash margin. Blepharitis, demodicosis and hyperkeratinization are common findings and contributors to dry eye complaints. Research reports that more than 40% of patients in a primary eye care setting have blepharitis.3 Additionally, more than 35% of chronic blepharitis is associated with keratoconjuctivitis sicca (KCS) and meibomian gland dysfunction (MGD).4 Direct bacterial infection, often led by Staphylococcus epidermidis, results in an increase in exotoxins and subsequent release of proinflammatory cytokines into the tear film.5
Demodex mites, the most common ectoparasites on human skin, can also be observed at the lid margin. The risk of demodicosis increases with age and is seen more frequently in patients with concurrent skin conditions such as rosacea.6 The presence of Demodex mites results in pathognomonic cylindrical dandruff at the base of lashes, follicular distention and misdirected or broken lashes.6
Telangiectasias and lid margin erythema are among the most common findings for ocular rosacea.7 Identification of this condition’s findings may precede those of dermatological rosacea in approximately 20% of cases.7 Patients may also exhibit signs such as lid swelling, blepharitis and MGD with more serious cases having potential for corneal neovascularization and thinning.8
Expressability of meibum is an essential component of a complete anterior segment examination and is easily observable at the slit lamp. Digital pressure can be applied to release oil to the surface of the lid margin or a meibomian gland evaluator can be employed to provide uniform and consistent pressure to the lids. Quality and quantity of secretions can be recorded and monitored during therapy for improvement.
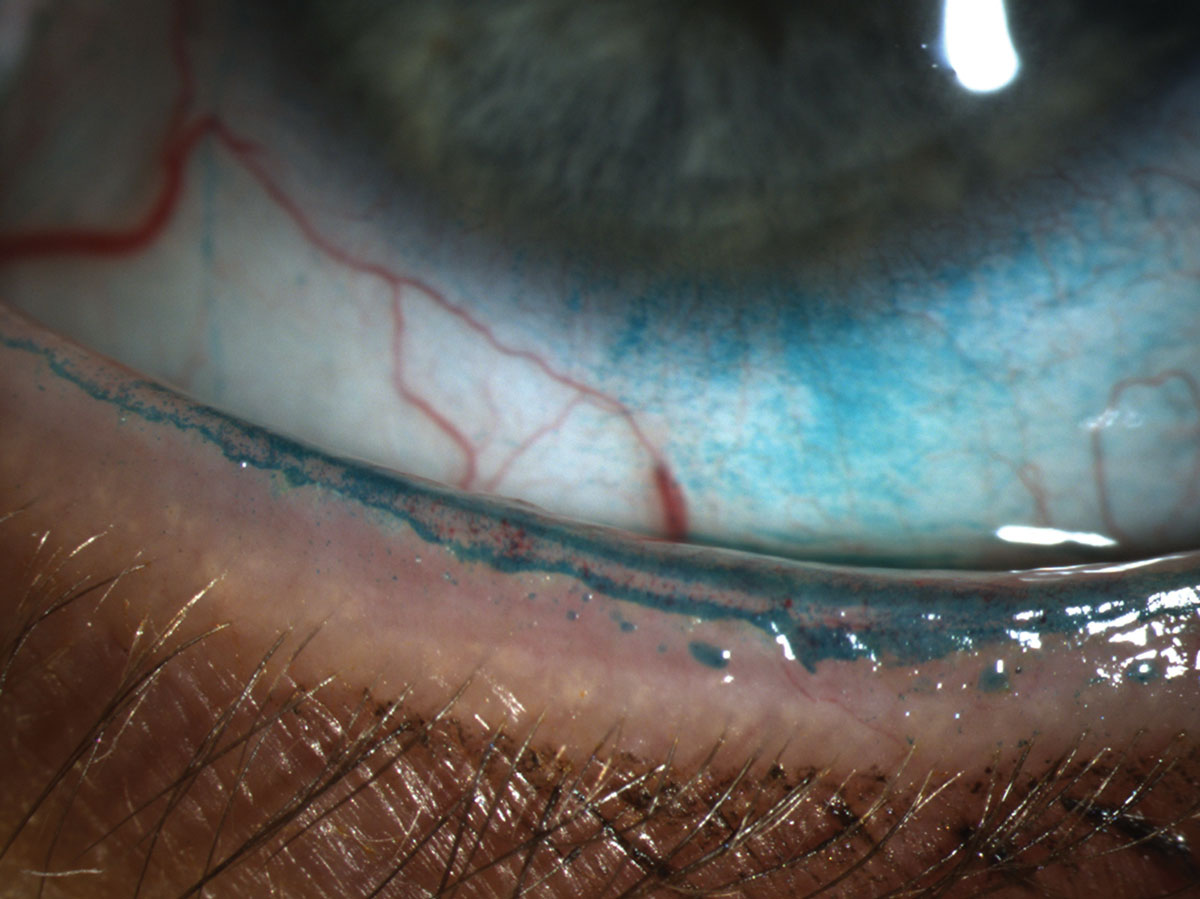 |
| Lissamine green instilled in the eye reveals a line of Marx that transects the meibomian gland orifice. Click image to enlarge. |
Mechanical Treatments
Lid debridement, or scaling, of the hyperkeratinized lid margin removes obstructive cells limiting meibum expression and contributing to gland obstruction. Instillation of lissamine green dye highlights the line of Marx (LOM), or mucocutaneous junction. In normal patients, the LOM naturally resides posterior to the meibomian glands but may move anteriorly in patients with MGD. Removing the layer of keratin can be beneficial.9
Microblepharoexfoliation can be performed using the BlephEx (BlephEx) or AB Max (Myco Industries) devices to mechanically remove biofilm, a potential contributor to DED, plus eyelid scurf and debris.10 The BlephEx procedure takes approximately six to eight minutes to complete all four lids and is well-tolerated by patients. The micro-sponge disposable tip removes debris from the eyelid surface and simultaneously exfoliates the lid margin. The AB Max device offers similar functionality plus a pulse mode designed to address hard-to-remove debris while gently massaging the lid margins, the manufacturer says.
Treat with Heat
Thermal treatments for MGD can be implemented in-office and, now, at-home as well. The fundamental principle behind each option is to provide a heat source to loosen the lipid-based meibum and make it more fluid for better incorporation into the tear film.
The most traditional device to deliver thermal therapy is a warming mask. These are highly accessible to patients, offer a great entry point into dry eye care for the newly diagnosed and are at an affordable price point. However, studies show not all warm compresses to be equally efficacious due to their inability to maintain a consistent temperature at 45°C (113°F) at the outer lid surface.11,12 This temperature is required to provide therapeutic heat to the meibomian glands.11,12 While warming masks can be recommended as an at-home option, their use can also be paired with in-office manual meibomian gland expression to provide greater release of impacted meibum relative to lid massage alone.
LipiFlow (Johnson & Johnson Vision) also offers an in-office thermal treatment. This closed-eye thermal device enables a hands-free 12-minute procedure that directly applies heat to the inside of the lid where the meibomian glands reside. Research shows a single LipiFlow treatment can provide lasting relief from signs and symptoms of evaporative DED for up to 12 months.13
In one study, 30 patients received the procedure and were evaluated at one month and one year.14 Eighteen returned for post-procedure evaluation at 12 months. At the visit, dry eye symptoms were scored and tear break-up time (TBUT) and meibomian gland function were measured. Patient symptoms and gland function continued to show significant improvement from baseline. However, the improvement in TBUT at one month was not maintained at the one-year follow up. LipiFlow improved dry eye symptom scores for 86% of treatment group subjects who received only one LipiFlow treatment and a sustained mean improvement in symptom score was noted from baseline.14
The iLux (Alcon) handheld device is a thermal treatment designed to allow the practitioner to visualize the meibomian glands through a magnifier during targeted expression. The operator actively controls the amount of heat and pressure during the treatment. Each treatment takes approximately 10 minutes (treating two zones/both eyes). It’s important to note the meibum may begin to melt within the gland and begin to release onto the lid margin prior to lid compression. Efficacy of the device was evaluated in a multi-center clinical trial with 142 subjects. The study found the iLux device provided efficacy for DED patients and showed non-inferiority to the predicate thermal device, LipiFlow.15
 |
| Pathognomonic cylindrical dandruff at the base of the lash due to demodecosis. Click image to enlarge. |
Another device, TearCare (Sight Sciences), uses adjustable thermal energy applied externally to the inferior and superior eyelids via adhesive strips. This thermal treatment takes 15 minutes to complete and is immediately followed by manual expression of the meibomian glands by the eye care provider. A hub controls temperature and is adjustable for patient comfort as needed. In addition, the instrument is portable in case you have multiple locations or need to move a patient from different rooms. As a safety feature, software within the hub continually monitors the thermal energy applied.
TearCare allows patients to keep their eyes open during the procedure, which may make them more comfortable and can encourage movement of melted meibum during the process.16
Pilot data from a single-center study shows improvement in subjects treated with TearCare relative to those treated with warm compress.16 Both signs and symptoms as measured by TBUT and Ocular Surface Disease Index (OSDI) significantly improved from baseline.16
A Bright Idea
Intense pulsed light (IPL) uses a non-laser high-intensity light source, or flashlamp, to create a broad wavelength of non-coherent light. The light pulse passes through a xenon gas-filled chamber with the energy pulse directed through a sapphire or quartz block. The operator controls the duration, intensity and spectral distribution of the pulse. While the mechanism of action of IPL has not been fully elucidated, studies show a reduction in cytokines in the tear film as compared with baseline values after IPL treatment.17,18 IL-17A and IL-6 showed statistically significant decreases post-procedure.17
More than 85% of patients with skin and eyelid inflammation also suffer from inflammatory ocular conditions.18 Patient selection for IPL procedures—such as those performed with the The M22 Optima (Lumenis)—is critical for safe and efficacious treatment. First, patients complete a skin survey to determine their skin type based on the Fitzpatrick Skin Scale, a six-point grading system used to determine the amount of pigment your skin has and your skin’s reaction to sun exposure. The patient should be counseled prior to treatment about potential adverse events and evaluation of their current medications. Before the procedure starts, a coupling gel is applied to the area to be treated.
A recent multi-center study with 40 enrolled subjects who underwent four treatment sessions three weeks apart found significant improvement in both the signs and symptoms of dry eye disease including TBUT, meibomian gland score and SPEED score.19
Eye-Light (Topcon) also offers IPL, as well as low-level light therapy (LLLT), which combines light modulation with optimized power energy (OPE). The unit treats both inferior and superior eyelids simultaneously without the need for a coupling gel. Instead, the Eye-Light has an internal cooling feature. The patient’s treatment parameters are managed by the unit’s software. The OPE uses a xenon flashtube to create a pulse with a 600nm wavelength and is applied to the periorbital area. The LLLT is delivered through a facemask containing an LED matrix designed to heat the upper and lower lids.
Five Warming Mask OptionsIn the old days, patients were advised to devise their own warm compress by filling a damp sock with rice and warm it in the microwave. However, these homespun remedies can have a lot of variability. Some patients were advised to use other various household items—including hard-boiled eggs—and temperature and compression times. Some of these methods heated the lid, but sapped it of moisture, the exact opposite of the intended outcome. Today, the market offers several well-researched items specifically designed for lid therapies. 1. Bruder Moist Heat Eye Compress (Bruder): The company’s MediBeads technology stores water molecules that are continuously absorbed from the air. When microwaved, the absorbed water is released as a moist heat. The company notes a significant increase in TBUT after using the product.1 2. Eye Doctor Click and Go, and Eye Doctor Plus Moist Heat Compress (The Dry Eye Doctor): This company offers a deep roster of products related to dry eye. The instant mask doesn’t require an oven or microwave to heat up. It’s activated by clicking a disk inside the compress to generate the heat and stays warm for approximately 20 minutes. Eye Doctor Plus Moist Heat Compress does require oven or microwave heat, but can also be cooled in a freezer to help relieve allergies or headaches.2 3. EyeEco boasts a product line designed to treat different stages of dry eye and can be heated to specific temperatures. Its Dry Eye Relief Mask is for mild dry eye and heats to 104˚. Its Tranquileyes Advanced heats to 110˚ and provides moist-heat for 12 to 15 minutes for moderate DED. Finally, the Tranquileyes XL Advanced for severe patients heats to 102˚ to 110˚ and provides moist heat for 20 to 25 minutes.3 4. TheraPearl eye mask (Bausch + Lomb): This microwavable option can be used as a 20-minute warm compress for DED patients or stored in a freezer and used as a cold compress.4 5. Thermal-1 Touch (OcuSoft) is a portable heated eye pad worn like a pair of glasses by the patient. The heat applied to the eyelids is a pre-set and controlled temperature with adjustable bridge and temples. The treatment takes between five and 10 minutes to complete twice daily at home.5
|
Maintenance
In-office treatment effectively hits a “reset button” for patients. However, maintaining that initial success and protecting the patient’s financial investment is essential for long-term patient satisfaction. Achieving this necessitates the use of at-home hygiene products.
One such lid-cleansing formulation, Zocushield (Okra), is composed of an okra polysaccharide complex. The gel is digitally applied by the patient in a gentle, circular fashion along the lids and lashes. The product also has an in-office companion, the Zest treatment, which incorporates Zoculshield gel as part of a treatment kit.
NuLids (NuSight Medical) is a compact, cordless, at-home lid cleaning device. A sterile, disposable tip is attached to the end of the unit and a lubricating gel is added as an interface. The tip gently vibrates and is placed at the edge of each eyelid for approximately 30 seconds. A pilot study into the device enrolled 37 patients and found improvement in both signs and symptoms of DED.20 Notably, after 30 days of treatment, TBUT increased and OSDI decreased.20 While the device is held near the eye, risk of adverse events were deemed low.20
Combining consistent at-home hygiene with demonstrably effective in-office procedures can help keep patients’ ocular surface rich in tears and their meibomian glands clear and active, limiting both signs and symptoms of dry eye. Successful management of DED must include evaluation, treatment and continued maintenance of the lids—today’s technologies are making it easier than ever to accomplish those goals.
Dr. Hauser is the director of clinical affairs for Keplr Vision. She also practices clinical care at The Eye Specialty Group in Memphis, TN and is the founder of Dry Eye Coach.
1. Chhadva P, McClellan A, Alabiad C. The impact of eyelid laxity on symptoms and signs of dry eye disease. Cornea. 2016 Apr; 35(4): 531–535. 2. Bashour M. Lower lid ectropion blepharoplasty workup. Medscape. emedicine.medscape.com/article/1281565-workup?src=refgatesrc1. December 22, 2015. Accessed October 14, 2019. 3. Lemp M, Nichols K Blepharitis in the United States 2009: a survey-based perspective on prevalence and treatment. Ocul Surf. 2009;7(2 Suppl):S1-14. 4. Nelson J, Shimazaki J, Benitez-del Castillo J, et al. The international workshop on meibomian gland dysfunction: report of the definition and classification subcommittee. Invest Ophthal Vis Sci. 2001;52(4):1930–1937 5. Putnam C. Diagnosis and management of blepharitis: an optometrist’s perspective. Clin Optom (Auckl). 2016; 8: 71–78. 6. Liu J, Sheha H, Tseng S. Pathogenic rold of Demodex mites in blepharitis. Curr Opin Allergy Clin Immunol. 2010;10(5):505–10. 7. National Rosacea Society. Ocular rosacea: what your eyes may be trying to tell you. www.rosacea.org/blog/2015/january/ocular-rosacea-what-your-eyes-may-be-trying-to-tell-you. January 20, 2015. Accessed October 14, 2019. 8. López-Valverde G, Garcia-Martin E, Larrosa-Povés J, et al. Therapeutical management for ocular rosacea. Case Rep Ophthalmol. 2016;7:237–42. 9. Korb D, Blackie C. Debridement-scaling: a new procedure that increases Meibomian gland function and reduces dry eye symptoms. Cornea. 2013;32(12):1554-7. 10. Rynerson J, Perry H. DEBS – a unification theory for dry eye and blepharitis. Clin Ophthalmol. 2016;10:2455–67. 11. Blackie C, Solomon J, Greiner J, et al. Inner eyelid surface temperatures as a function of warm compress methadology. Opt Vis Sci. 2008;85(8):675-83. 12. Murakami DK, Blackie C, Korb D. All warm compresses are not equally efficacious. Optom Vis Sci. 2015;92(9):e327-33.. 13. Greiner J. Long-term (12-month) improvement in meibomian gland function and reduced dry eye symptoms with a single thermal pulsation treatment. Clin Exp Ophthalmol. 2013;41(6):524-30. 14. Blackie C, Coleman C, Holland E. The sustained effect (12 months) of a single-dose vectored thermal pulsation procedure for meibomian gland dysfunction and evaporative dry eye. Clin Ophthalmol. 2016;10:1385-96. 15. Tear Film Innovations. Randomized Comparison between iLux and LipiFlow in the treatment of meibomian gland dysfunction. clinicaltrials.gov/ProvidedDocs/32/NCT03055832/Prot_SAP_000.pdf. April 3, 2019. Accessed October 14, 2019. 16. Badawi D. A novel system, TearCare, for the treatment of the signs and symptoms of dry eye disease. Clin Ophthalmol. 2018;12:683–94. 17. Liu R, Rong B, Tu P, et al. Analysis of Cytokine Levels in Tears and Clinical Correlations After Intense Pulsed Light Treating Meibomian Gland Dysfunction. Am J Ophthalmol. 2017;183(11):81-90 18. Viso E, Millán AC, Rodríguez-Ares MT. Rosacea-associated meibomian gland dysfunction–an epidemiological perspective, Eur Ophthalmol Rev. 2014;8(1):13-16. 19. Dell S, Gaster R, Barbarino S, Cunningham D. Prospective evaluation of intense pulsed light and meibomian gland expression efficacy on relieving signs and symptoms of dry eye disease due to meibomian gland dysfunction. Clin Ophthalmol. 2017;11:817-27. 20. Schanzlin D, Olkowski J, Coble J, et al. Efficacy of self-administration of a personal mechanical eyelid device for the treatment of dry eye disease, dlepharitis and meibomian gland disease. NuSight Medical. east.visionexpo.com/__novadocuments/548696?v=636848314252030000. Accessed October 14, 2019. |

