  |
Over many years of presenting continuing education courses, we have had the great fortune to meet thousands of our colleagues. We have always fielded questions from the audience and, when the same inquiries come up in several different audiences, we often incorporate them into future lectures. There are two questions involving intraocular pressure (IOP) that we have heard numerous times. The first is whether or not to lower IOP in eyes with optic disc drusen and visual field loss to prevent further neuronal compromise and progression of visual defects. The second is whether or not to lower IOP in ocular hypertensive eyes to prevent a possible retinal vascular occlusion.
In this month’s column, we attempt to shed scientific light on these two common conundrums.
Disc Drusen
Optic disc drusen (ODD) represent retained hyaline bodies in the optic nerve. Typically, patients with ODD present and remain without symptoms, with the finding disclosed only upon routine ocular evaluation. In some instances, the condition can present with mildly decreased visual acuity and visual field defects.1-5 An afferent pupillary defect may be noted if the condition is both significant and unilateral or asymmetric.2
The classic appearance of ODD involves unilaterally or bilaterally elevated optic discs with irregular or “scalloped” margins, a small or nonexistent cup and unusual vascular branching patterns (i.e., marked bifurcations and trifurcations) that arise from a central vessel core. There may be refractile hyaline deposits visible on the surface of the disc or in the peripapillary area, making the diagnosis clear. In younger patients, the disc elevation tends to be more pronounced and the drusen less calcified and discrete, making them less visible ophthalmoscopically—complicating diagnosis.
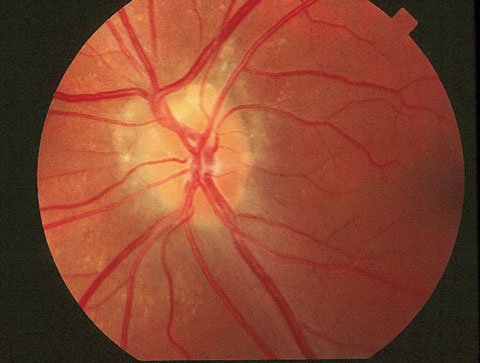 |
| This fundus image demonstrates an eye with superficial optic disc drusen. |
Within the optic nerve, the hyaline bodies are confined anterior to the lamina cribrosa and can compress and compromise the nerve fibers and vascular supply, leading to visual field defects and disc hemorrhages.2-6 Along with slowly developing optic atrophy in extreme cases and possible venous occlusion, disruption of the juxtapapillary tissue can result in choroidal neovascular membrane formation, leading to subretinal hemorrhage, with its attendant complications.7-9
While ODD is typically considered a benign condition, it can lead to modest visual compromise and, in rare instances, devastating vision loss.10-12 Although the condition is typically slow to advance, there is a risk of progressive vision loss or visual field loss over time.
A retrospective analysis of eyes with ODD, both with and without concurrent elevated IOP, reported visual field defects in 91% of ocular hypertensive eyes with ODD and 67% of normotensive ODD eyes, clearly showing that eyes with ODD and concurrent ocular hypertension had a greater prevalence of visual field loss.10 The researchers concluded that patients with elevated IOP and ODD should remain under close surveillance for disease progression and be treated appropriately to prevent additional visual field loss.10 Two other small reports also advocated IOP reduction in eyes with ODD and concurrently elevated IOP.12,13
This approach seems reasonable, in that the anomalous nature of the optic discs precludes accurate assessment for glaucoma, and pre-existing retinal nerve fiber layer (RNFL) and visual field loss from ODD can mask damage that may occur from elevated IOP. However, it is unknown if lowering IOP in these cases actually reduces the risk of progression of visual field loss.
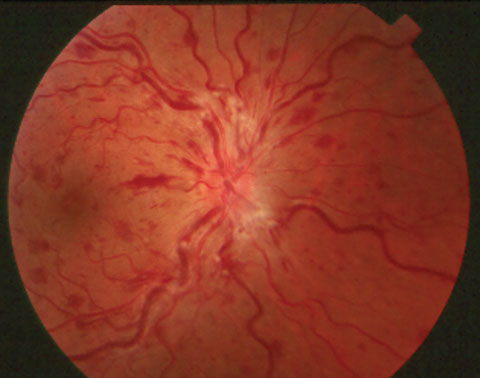 |
| This fundus image shows an eye with central retinal vein occlusion. |
Should any eye with significant ODD develop elevated IOP, consider offering the patient prophylactic pressure reduction. In the absence of elevated IOP, there is no evidence that IOP reduction will have any effect on preventing visual morbidity.10 There are no controlled clinical studies that show a benefit to lowering IOP in any eyes with ODD.
Retinal Vein Occlusion
The etiology of central retinal vein occlusion (CRVO) is thrombotic obstruction of the central retinal vein as it constricts through the lamina cribrosa. This may involve abnormal blood flow or blood constituents, atherosclerosis, vessel anomalies or a combination of these factors. Essentially, properties of blood and the vein itself act in concert to cause thrombus formation with subsequent impedance of venous blood flow from the retina.14,15
There are numerous ways that a thrombus forms within the central retinal vein. Blood flow, combined with vessel wall abnormalities, can stimulate vein thrombosis. Additionally, changes in blood constituents, such as hypercoagulability states, elevated viscosity and systemic states of decreased thrombolysis promote thrombus formation. External factors, such as papilledema (causing increased pressure in the optic nerve sheath), may cause further compression and contribute to occlusion.14,15 Potentially, elevated IOP could cause impedance of blood flow through the retinal veins, subsequently promoting thrombus formation and occlusion. Investigators note that CRVO and hemi-central retinal vein occlusion have a significant association with glaucoma and ocular hypertension; however, they also note that, paradoxically, few patients had high IOP in the eye with the vascular occlusion.16 In fact, IOP elevation was more likely to occur in the fellow, uninvolved eye.16 An old adage advocates treating elevated IOP if, for no other reason, to prevent a retinal vascular occlusion. However, it would seem that this practice would negate much of what we have learned from the Ocular Hypertension Treatment Study (OHTS) regarding lowering IOP in ocular hypertensive eyes to prevent glaucoma formation. Do we really want to lower IOP in every ocular hypertensive eye due to fear of retinal vascular occlusion (RVO)?
The most definitive answer to the question of prophylaxis against RVO comes from OHTS. Researchers included 1,636 ocular hypertensive participants—with a mean follow-up of 9.1 years—who had been randomized either to prophylactic IOP reduction or close observation. In a sub-analysis, they noted that 26 RVOs occurred in 23 participants, 15 in the observation group and eight in the medication group. They saw that the 10-year cumulative incidence of RVO was 2.1% in the observation group with untreated ocular hypertension and 1.4% in the medication group. Although the incidence of RVO was higher in the observation group than the medication group, this difference did not attain statistical significance.17 Based upon this evidence, we cannot justify recommending that ocular hypertension be treated to prevent against RVO. In fact, the 10-year incidence of RVO in ocular hypertensive eyes is really quite low.
|
1. Friedman A, Gartner S, Modi S. Drusen of the optic disc: a retrospective study in cadaver eyes. Br J Ophthalmol. 1975;59(8):413-21. 2. Rosenberg M, Savino P, Glaser J. A clinical analysis of pseudopapilledema: I, population, laterality, acuity, refractive error, ophthalmoscopic characteristics, and coincident disese. Arch Ophthalmol. 1979;97(1):65-70. 3. Katz B, Pomeranz H. Visual field defects and retinal nerve fiber layer defects in eyes with buried optic nerve drusen. Am J Ophthalmol. 2006;141(2):248-53. 4. Lee A, Zimmerman M. The rate of visual field loss in optic nerve head drusen. Am J Ophthalmol. 2005;139(6):1062-6. 5. Purvin V, King R, Kawasaki A, Yee R. Anterior ischemic optic neuropathy in eyes with optic disc drusen. Arch Ophthalmol. 2004;122(1):48-53. 6. Wilkins J, Pomeranz H. Visual manifestations of visible and buried optic disc drusen. J Neuroophthalmol. 2004;24(2):125-9. 7. Brown S, Del Monte M. Choroidal neovascular membrane associated with optic nerve head drusen in a child. Am J Ophthalmol. 1996;121(2):215-7. 8. Diduszyn J, Quillen D, Cantore W, Gardner T. Optic disk drusen, peripapillary choroidal neovascularization and POEMS syndrome. Am J Ophthalmol. 2002;133(2):275-6. 9. Romero J, Sowka J, Shechtman D. Hemorrhagic complications of optic disc drusen and available treatment options. Optometry. 2008;79(9):496-500. 10. Grippo TM, Shihadeh WA, Schargus M, et al. Optic nerve head drusen and visual field loss in normotensive and hypertensive eyes. J Glaucoma. 2008;17(2):100-4. 11. Gili Manzanaro P, Yangüela Rodilla J, Rodríguez Caravaca G.,et al. Decreased visual acuity from optic disc drusen. Arch Soc Esp Oftalmol. 2010;85(2):64-9. 12. Morris R, Ellerbrock J, Hamp A, et al. Advanced visual field loss secondary to optic nerve head drusen: case report and literature review. Optometry. 2009;80(2):83-100. 13. Spalding J. Visual-field loss with optic nerve drusen and ocular hypertension: a case report. Optometry. 2002;73(1):24-32. 14. Turello M, Pasca S, Daminato R, et al. Retinal vein occlusion: evaluation of “classic” and “emerging” risk factors and treatment. J Thromb Thrombolysis. 2009 Aug 11. [Epub ahead of print]. 15. Yau J, Lee P, Wong T, et al. Retinal vein occlusion: an approach to diagnosis, systemic risk factors and management. Intern Med J. 2008;38(12):904-10. 16. Hayreh S, Zimmerman M, Beri M, Podhajsky P. Intraocular pressure abnormalities associated with central and hemicentral retinal vein occlusion. Ophthalmology. 2004;111(1):133-41. 17. Barnett E, Fantin A, Wilson B, et al. The incidence of retinal vein occlusion in the ocular hypertension treatment study. Ophthalmology. 2010;117(3):484-8. |

