 |
Q:
What are your options when a scleral contact lens patient complains of hazy, cloudy vision due to hypoxic corneal edema a few hours after lens application?
A:
Scleral lenses reduce the amount of oxygen that gets through to the cornea due to factors such as lens thickness and material, tear reservoir depth and the semi-sealed fit, according to Chelsea Bradley, OD, a clinical instructor at the Illinois College of Optometry. “When corneal edema occurs as a result of hypoxia, do everything you can to increase oxygen flux to the cornea,” she recommends.
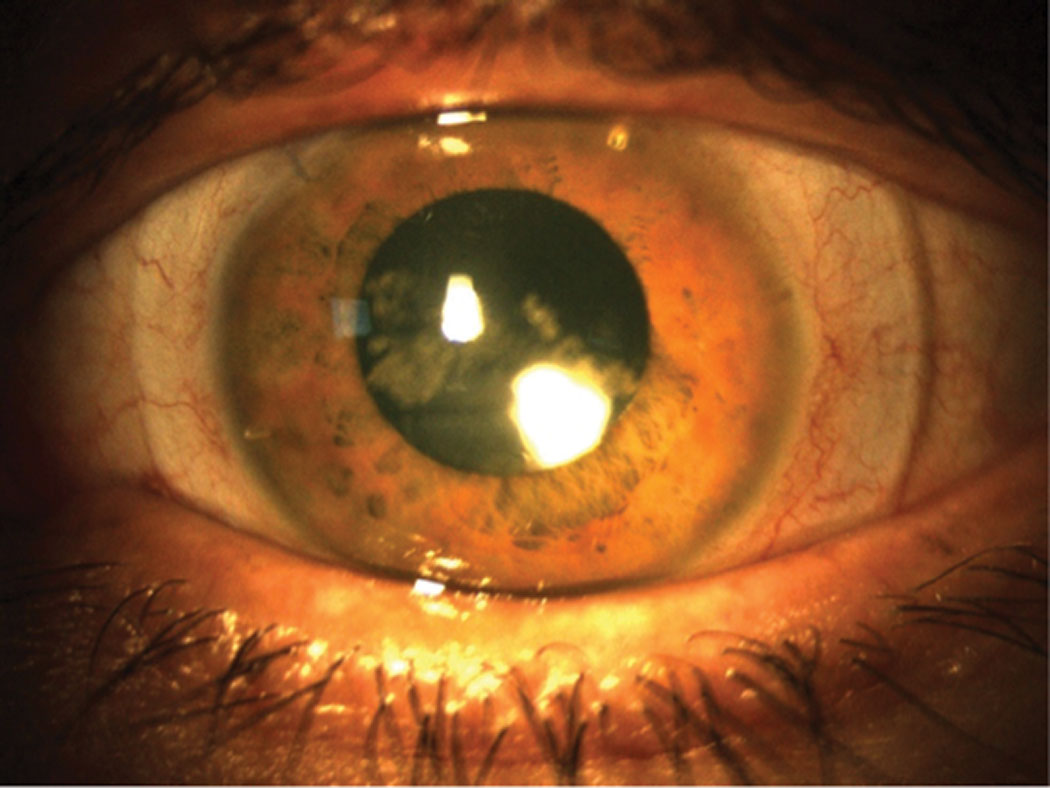 |
| A scleral lens with too much tear exchange can cause debris to collect in the bowl (seen centrally) and reduce the patient’s visual acuity. Click image to enlarge. |
Optimize the Fit
In a perfect world, Dr. Bradley says, the patient would switch to a lens modality with a higher rate of tear exchange and greater oxygen transmission, such as a corneal gas permeable, hybrid or soft lens. However, she notes that many scleral lens wearers have an advanced form of disease that takes other lens modalities out of the running, so changing the parameters of the scleral lens is generally the only option.
Dr. Bradley suggests taking these steps: (1) Fit the scleral to have as little central clearance as possible while still maintaining a healthy fit (typically about 100µm after settling), (2) order the lens with the highest Dk material possible (most labs have a hyper-Dk material option available for scleral lenses) and (3) decrease the center thickness of the lens as much as possible to increase the Dk/t value. She recommends implementing these changes to any lens causing hypoxic edema, as they often resolve the issue.
If the edema persists, Dr. Bradley says to consider flattening the haptics of the lens to achieve a looser fit and promote greater tear exchange. However, she adds that this could introduce more debris into the bowl of the lens and cause patient discomfort, lens fogging or both. She offers another option: performing fenestrations or channels on the lens to promote additional tear exchange. While this used to be the most common solution to scleral lens-induced hypoxic corneal edema, she notes that it fell to the sidelines with the invention of hyper-Dk materials, which typically allow enough oxygen to permeate.
In addition to making physical changes to the lens fit, Dr. Bradley says the patient can take breaks from scleral lens wear throughout the day when they have lower visual demands.
Graft Considerations
For patients who have corneal grafts, Dr. Bradley notes that the same rules apply for minimizing edema. However, in these patients, she cautions that hypoxia is not the only contributing factor; endothelial cell count is also important.
These patients should have an endothelial cell count of at least 800 cells/mm2 to lessen the risk of developing edema with scleral lens wear, according to Dr. Bradley. At an endothelial density lower than this, Dr. Bradley warns that many patients will develop corneal edema throughout the day, even if all the lens parameters are adjusted for maximum oxygen permeability.
Final Thoughts
“Hypoxic corneal edema from scleral lenses is almost always treatable by making one or several of these changes,” Dr. Bradley concludes.

