|
|
 |
An 11-year-old Hispanic female presented with complaints of sudden onset of blurred vision and floaters in her right eye for the past two weeks. She also reported that her peripheral vision in that eye was reduced. She denied any pain or discomfort. The left eye was unaffected.
Her ocular history was unremarkable and she reported good health. She took no medications.
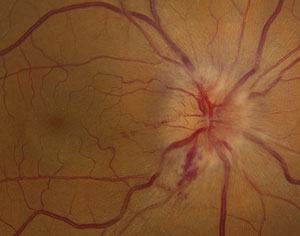
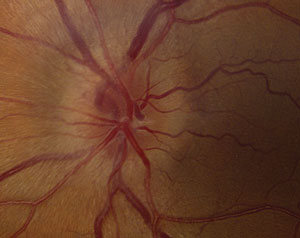
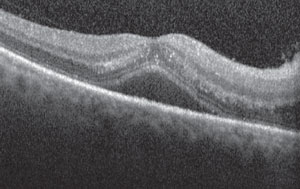
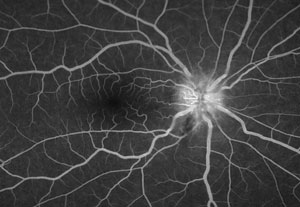
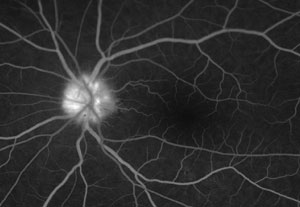
On examination, her best-corrected visual acuity was 20/30 OD and 20/20 OS. Confrontation fields were full to careful finger counting OU. The pupils were equally round and reactive, with a 1+ afferent defect in the right eye. Anterior segments were unremarkable.On dilated fundus exam, the vitreous was clear in both eyes. Exam of the right eye showed fundus changes (figure 1); the peripheral retina was normal. Fundus exam of the left eye showed a pink optic nerve with elevated disc margins (figure 2). The macula, vessels and periphery were normal. We performed spectral-domain optical coherence tomography (SD-OCT) (figure 3) as well as fluorescein angiography (figures 4 and 5) of the macular region of both eyes.
|
|
Figs. 1 & 2. Fundus image of the right eye (left photo) shows fundus changes. Fundus image of the left eye (right)
shows a pink optic nerve with elevated disc margins. |
Take the Retina Quiz
1. What do the fundus changes in the right eye show?
a. Swollen optic nerve.
b. Disc swelling and macular star.
c. Neurosensory retinal detachment.
d. Papilledema.
2. What additional testing would be most helpful in making the correct diagnosis?
a. Visual field.
b. Fasting blood glucose.
c. Blood test, including an ELISA for Bartonella henselae
.
d. Neuroimaging, including MRI.
|
|
| Fig. 3. SD-OCT image of the patient's right eye. |
|
3. What does the optic nerve of the left eye represent?
a. It’s normal.
b. Disc swelling.
c. Optic nerve drusen.
d. Ischemic optic nerve.
4. What is the most likely diagnosis?
a. Idiopathic intracranial hypertension.
b. Optic neuritis.
c. Neuroretinitis.
d. Papilledema.
5. What is the treatment for this patient?
a. Intravitreal Avastin.
b. Doxycycline PO.
c. Prednisone PO.
d. Weight loss.
For answers, scroll to the bottom.
Diagnosis
Our patient has optic nerve swelling and a neurosensory retinal detachment in the right eye and optic nerve drusen in the left. If you look closely at her macula in the right eye, you’ll also see that she has exudate in a “macular star” pattern. This presentation most likely represents a neuroretinitis caused by Bartonella henselae
, or cat-scratch disease (CSD). Our patient admitted to having two cats and one dog. However, she didn’t recall being scratched by her cats.
|
| Figs. 4 & 5. Fluorescein angiography OD (left image) and OS (right image). |
We ordered a blood work-up that included angiotensin-converting enzyme (ACE) and complete blood count with differential, IgG and IgM titers for Bartonella henselae, and antibodies for toxoplasmosis. She also underwent visual field testing, which showed an enlarged blind spot and an inferior arcuate-like defect in the right eye.
We elected to treat her empirically with doxycycline PO 100mg BID until the results of the blood studies were available. The IgG results came back strongly positive. When we questioned the patient further, although she didn’t recall any cat scratches she admitted that she bites/chews on her fingernails, and related that quite often the cats lick her fingers. We surmised that was the likely route of her infection.
Discussion
The term neuroretinitis
is synony-mous with Leber’s stellate neuroretinitis
, a condition that was originally identified in 1916 by Theodor Leber, who described a clinical syndrome in which patients had unilateral vision loss in the presence of a macular star.1
He believed that the problem primarily involved the macula.
By 1977, Dr. J. Donald M. Gass showed that patients with macular star also had swelling of the optic disc before and often concurrently with the appearance of the star formation.1,2 Dr. Gass concluded that the condition was not primarily a maculopathy but rather an optic neuritis that affected both the optic nerve and retina. Thus, he called it a neuroretinitis.1,2
Neuroretinitis affects persons of all ages, but is more commonly seen between ages 30 and 40. It’s generally painless, but may include varying degrees of pain. Interestingly, about 50% of patients with neuroretinitis will report having had a preceding viral-like illness.1 As a result, for many years this condition was classified as a “post-viral neuroretinitis.” The condition tends to be self-limiting, for a period of six to eight weeks.1
The clinical features of neuroretinitis include disc swelling in the presence of an exudative maculopathy that resembles a star-like pattern. The exudate may not be present during the initial stages of the disc swelling, but appears within days to weeks as the optic disc swelling begins to resolve.
Other inflammatory signs may also be present, including anterior chamber cells and flare, vitreous cells and venous sheathing. Interestingly, even though our patient reported seeing floaters, she did not have any cells in the anterior chamber or the vitreous. In addition, she had also developed a neurosensory retinal detachment as result of the extreme amount of disc swelling.
Only 5% to 10% of patients with CSD develop ocular involvement, and only about 1% to 2% develop neuroretinitis.3 CSD is now recognized as the cause for the majority of neuroretinitis cases. Other infectious causes of neuroretinitis include syphilis, Lyme disease, Leptospira, toxoplasmosis and toxocariasis.
The link between CSD and neuroretinitis was found thanks to advances in biomolecular laboratory techniques in the 1990s, including specific serologic tests and polymerase chain reaction analyses.
Two types of serologic tests are used for the diagnosis of CSD. One is an indirect fluorescent assay specific for antibodies directed against B. henselae. It has a sensitivity and specificity above 90% but does not differentiate between IgM and IgG antibodies.4 The other commercially available serologic test is an enzyme-linked immunoassay for both IgG and IgM anti-B. henselae antibodies.
Oral doxycycline 200mg BID for two to four weeks has emerged as the treatment of choice for neuroretinitis even though the disease is self-limiting, and this is what we prescribed our patient. When she returned for follow-up in two weeks, she reported a significant improvement in her symptoms. The neurosensory detachment had resolved and her acuity had improved to 20/20. By six weeks, she said she felt entirely better and her visual fields were completely normal.
1. Smith CH. Optic Neuritis. In: Walsh & Hoyt’s Clinical Neuro-Ophthalmology. Miller NR, Newman NJ,eds, Vol. I. 6th ed. Philadelphia: Lippincott Williams & Wilkins; 2005: 293-347.
2. Dreyer RF, Hopen G, Gass JDM, Smith JL. Leber’s idiopathic stellate neuroretinitis. Arch Ophthalmol. 1984 Aug; 102(8):1140-5.
3. Suhler EB, Lauer AK, Rosenbaum JT. Prevalence of serologic evidence of cat scratch disease in patients with neuroretinitis. Ophthalmology. 2000 May;107(5):871-6.
4. Dalton MJ, Robinson LE, Cooper J, et al. Use of Bartonella antigens for serologic diagnosis of cat-scratch disease at a national referral center. Arch Intern Med. 1995 Aug 7-21; 155(15):1670-6.
1) b; 2) c; 3) c; 4) c; 5) b.

