Pediatrics in the Optometric PracticeFollow the links below to read the other articles from our report on pediatrics in the optometric practice: Testing Children for Accommodative and Convergence Disorders |
Amblyopia, a disorder of visual development that occurs in childhood, can have lasting effects in adulthood if not detected and treated in a timely manner. It occurs frequently, with a prevalence between 1% and 5% of the general population.1 The World Health Organization estimates 12 million children younger than age 15 are visually impaired due to uncorrected refractive errors and amblyopia.1 Research also suggests functional amblyopia is the leading cause of monocular vision loss in adults older than age 20.2 This vision loss can be prevented with timely diagnosis and treatment, and clinicians are capable of providing their amblyopic patients with good vision in childhood that can last throughout life.
This is not a rare condition, and eye care providers, particularly those caring for a pediatric population, must have the knowledge and tools to effectively treat amblyopia.1 While refractive correction and occlusion are mainstays, vision therapy is making new inroads.
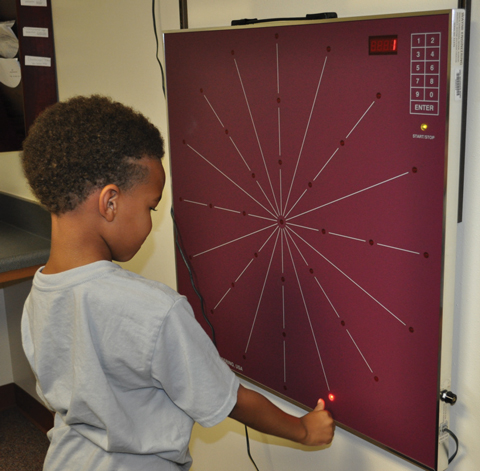 |
| This oculomotor activity addresses saccadic dysfunction with a Wayne saccadic fixator and a timed exercise with multiple setting and testing options. |
Ocular Effects
Although visual acuity is often the focus of management, amblyopia impacts many other elements of the visual system. Patients with amblyopia often have decreased oculomotor and fixation ability, accommodative skills, binocular summation, contrast sensitivity and stereoacuity.3 These deficiencies are often paired with increased spatial distortion and crowding effects, as well as suppression under binocular viewing conditions.2,3 Amblyopia can affect a child’s ability to function in a classroom setting and increase their chances for a vision-based learning problem.
 |
| Accommodative flippers are used in many vision therapy activities. |
Early detection is key in preventing long-term effects of amblyopia. The primary development of visual pathways occurs from birth to six to eight years of age.2 During this time, the visual system is most vulnerable to amblyogenic factors—the mechanisms that disrupt normal visual development. Such factors include optical defocus, strabismus, form deprivation or a combination of all three.2 If any of these are present at birth up to age eight when visual development is susceptible, amblyopia can develop.
Optical defocus. This is caused by uncorrected refractive error in one or both eyes. Anisometropic amblyopia is caused by a difference in refractive error between the two eyes, while isoametropic amblyopia is caused by high refractive error roughly equal between both eyes (Tables 1 and 2).2
Strabismus. Strabismic amblyopia is most commonly associated with an early-onset constant unilateral strabismus.2 The deviation causes the eyes to be presented with two different images, causing double vision and visual confusion. Rather than trying to reconcile these different images, the image from the deviating eye is actively suppressed.2
Form deprivation. This type of amblyopia results from a physical obstruction on the visual axis that prevents a sharp, clear image from forming in one or both eyes. The obstruction must be present from birth to approximately age eight.2 The most common cause of form deprivation amblyopia is congenital cataract, although it can also be caused by other conditions such as ptosis and corneal opacities.2
In addition to the mechanism driving development, amblyopia is categorized based on severity. The Pediatric Eye Disease Investigator Group (PEDIG) conducted a research series called the Amblyopia Treatment Studies (ATS), which provided not only a severity grading scale, but also guidance on treatment options for various age groups and visual acuities.
A thorough eye exam can help practitioners determine the presence and type of amblyopia. After the diagnosis, a typical treatment progression may include correction of refractive error with spectacles, occlusion therapy and vision therapy. PEDIG’s extensive research in various treatment modalities provides practitioners a more uniform and effective level of care, and can act as a clinical guidepost for treating patients with amblyopia.
PEDIG Studies Under the MicroscopeThe PEDIG’s Amblyopia Treatment Studies (ATS) are an integral part of amblyopia treatment paradigm. ATS 1, 2B, 4 and 10 deal with patients younger than 10 with moderate amblyopia. These studies determined:
PEDIG also determined that six hours of daily prescribed patching is as equally effective as full-time patching in severe amblyopes ages seven and younger.5 For older children (between the ages of seven and 13) with moderate to severe amblyopia, patching can improve visual acuity even if the amblyopia has been treated previously. For children age 13 to 18, patching can improve visual acuity only if the amblyopia has not been previously treated.6 Knowing the results of these studies provides a practitioner with multiple options for successful amblyopia therapy, even with difficult patients. 1. Pediatric Eye Disease Investigator Group (PEDIG). A comparison of atropine and patching treatments for moderate amblyopia by patient age, cause of amblyopia, depth of amblyopia, and other factors. Ophthalmology. 2003;110(8):1632-7. | ||||||||||
Spectacles
The first step to effective amblyopia treatment is correction of refractive error with spectacles. An accurate spectacle Rx is critical to ensuring a clear retinal image in each eye. The use of cycloplegics is necessary to obtain this information, particularly in pre-verbal children or those unable to successfully participate in the process of subjective refraction.
Skillful retinoscopy is especially useful to determine the presence or absence of anisometric or isoametropic amblyogenic risk factors. If amblyogenic risk factors are present, full-time spectacle wear becomes necessary for treatment.
Research shows spectacle correction alone can provide resolution in roughly 27% of patients ages three to seven with uncorrected anisometropic amblyopia.4 For patients with strabismic or combined aniso-strabismic amblyopia in the same age group, glasses alone were able to provide improvement of visual acuity of greater than two lines in 75% of patients, with 32% showing total resolution.5 Spectacles can be worn until a plateau occurs in visual acuity. If there is residual amblyopia, additional treatment is necessary.
 |
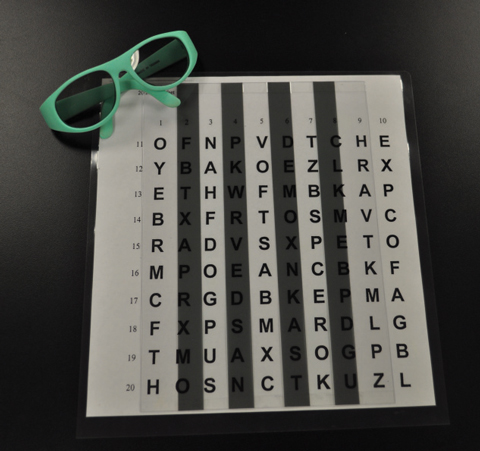
| This is an anti-suppression activity through Gerull Labs’ Opto App. It contains a library of activities that can be completed on an iPad without any additional equipment or with either a stereoscope or red/cyan glasses. This allows excellent cancellation and depth perception targets. Photo: Gerull Labs |
Occlusion
Total occlusion is achieved by patching of the better-seeing eye, while partial occlusion is achieved with atropine eye drops, Bangerter foils or contact lenses. All types of occlusion have the same guiding principle: occluding the better-seeing eye forces the amblyopic eye to work, allowing it to develop stronger neural connections in the visual cortex.2
Table 1. Anisometropic Amblyogenic Factors | |
| Condition | Diopters |
| Hyperopia | >1.00D |
| Myopia | >3.00D |
| Astigmatism | >1.50D |
Table 2. Isoametropic Amblyogenic Factors | |
| Condition | Diopters |
| Hyperopia | >5.00D |
| Myopia | >8.00D |
| Astigmatism | >2.50D |
Atropine. This is only effective if the sound eye is hyperopic. The atropine drop makes near vision blurry in the unaffected eye, forcing the child to rely on the amblyopic eye for near work. Atropine drops are an excellent alternative for patients who are noncompliant with eye patching therapy, as it is impossible to remove or peek around an eye drop once instilled. This treatment modality is excellent for high-energy patients who fuss with an eye patch, children with busy schedules or older patients with cosmetic concerns. This treatment option also promotes binocular vision. Drawbacks of atropine include being a prescription eye drop that needs to be filled and an intense stinging sensation on instillation. Light sensitivity is also an issue, as atropine produces a dilated pupil.
Bangerter foils. These can be applied to a spectacle lens of the sound eye to produce a blurred image at both distance and near. As vision improves in the amblyopic eye, practitioners can reduce the grade of blur by changing the foils. These also help promote binocularity and are excellent for older children with cosmetic concerns. However, a Bangerter foil should be used with caution on those suspected of noncompliance, as it could be quite easy to peek around the glasses.
 |
| Vectograms can help assess fusion and expand fusional vergence during therapy. They can reveal how the binocular system is functioning. |
 |
| Most activities incorporating a Marsden ball help address oculomotor dysfunction. This activity promotes hand-eye coordination and helps with spatial awareness. |
Vision Therapy
While traditional treatment for amblyopia improves monocular function by providing visual input to the amblyopic eye, vision therapy can assist in treating the underlying binocular dysfunction that accompanies amblyopia.6 By initiating vision therapy, the doctor can reduce the total amount of therapy time necessary.2,3,7 Additionally, adding vision therapy to occlusion, partial or total, is considered to be more effective than occlusion alone.6
Accessing Vision Therapy If your patient would benefit from vision therapy but you are unable to provide it in your practice, you can find a doctor who practices vision therapy by using the College of Optometrists in Vision Development’s (COVD) locate a doctor search function (http://locate.covd.org) or the Optometric Extension Program Foundation’s (OEPF) practitioner search map (http://oepf.org/page/map). To add vision therapy to your practice, you can start by attending OEPF clinical curriculum courses (http://oepf.org/clinical-curriculum) or COVD courses (www.covd.org/?page=annual_meeting). In addition, hiring an optometrist with advanced training or clinical experience in vision therapy can help you incorporate this treatment modality into your practice with confidence. |
Vision therapy can focus on increasing accommodation, improving accuracy of oculomotor skills, increasing vergence ranges, improvement of spatial perception, and breaking suppression and eccentric fixation.7,8 The treatment goal is for the patient to effortlessly function with sound visual skills at a high level of binocularity. This high level of binocularity helps improve vision and will prevent the regression of visual acuity after amblyopia treatment has stopped.2,3,6,9
While all aspects of the visual system need to be addressed, a skilled practitioner can tailor the vision therapy plan for each patient’s needs. Plans can be individualized to address those deficiencies observed in an exam, and the signs and symptoms reported by the patient.
Vision therapy consists of planned activities, individually prescribed and monitored to develop efficient visual skills and processing.10 It typically consists of a 45-minute weekly in-office appointment, and the patient is typically assigned 15 minutes of nightly homework. Most therapies range from several weeks to several months, depending on factors such as the number and severity of diagnoses and patient compliance and motivation. For vision therapy to succeed, compliance is essential, and it is important to stress to the patient the importance of attending weekly therapy sessions and completing the assigned homework. With new computer-based therapies, tracking homework is easier than ever.
 |
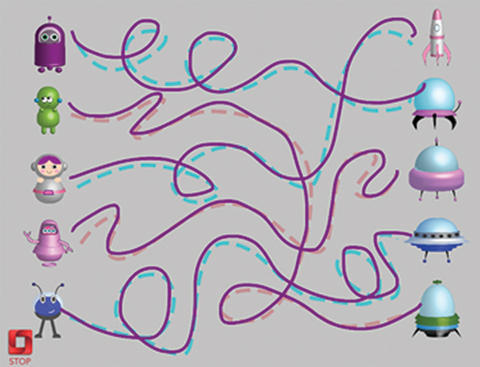
| In this anti-suppression activity, the patient uses a polarized bar reader with polarized glasses. |
Vision therapy uses lenses, prism, filters, occluders and specialized equipment during prescribed activities.10 Computer programs and interactive tablet apps have taken traditional vision therapy activities and turned them into new, interactive and exciting exercises for our patients. Another new development is the possibility of using virtual reality or binocular video games as a form of amblyopia treatment. PEDIG has been investigating the use of a binocular iPad game to determine if video game play can be as effective as patching. ATS 18 was designed to determine if amblyopic-eye visual acuity improvement treated with a binocular iPad game is as effective as part-time patching. For a younger cohort of patients, the study was inconclusive and unable to establish if iPad game play was worse than two hours of prescribed patching.11 Research is still pending for an older age group.
Amblyopia Management2These treatment options are in no specific order and are determined by doctor and patient needs: Anisometropic Amblyopia
Isoametropic Amblyopia
Form Deprivation Amblyopia
These patients need their visual acuity and binocular development followed closely the first year. Strabismic Amblyopia
|
Vision therapy activities used to address accommodation should increase accommodative accuracy, ability, amplitude and reaction time. Research shows incorporating lenses into accommodative activities, as in monocular accommodative rock and binocular accommodative rock, is more effective than activities that stimulate accommodation using a target distance as in hart chart near-far rock.7
To assist patients in developing normal eye movements and central fixation, the therapy plan can incorporate ocular motor activities to improve eye-hand coordination, accuracy of pursuits, saccades and fixation.2 To improve the patient’s spatial processing, the patient can complete word searches or hidden picture activities.
It is important to incorporate anti-suppression activities in amblyopia treatment, as patients with amblyopia have a complete, but suppressed binocular system.12 Anti-suppression activities help promote binocularity in normal viewing conditions, improve fusion, expand vergence ranges and develop stereopsis.6,12 To help lower suppression, the amblyopic eye participates in anti-suppression techniques that require it to become more competitive with the non-amblyopic eye.8 Under artificial viewing conditions where the amblyopic eye is not suppressing, information from the two eyes can be combined normally.12 There will be overall improvement the longer the patient is binocular in an artificial environment.12 Some practitioners suggest introducing anti-suppression therapy early in the treatment plan to allow the amblyopic eye to function in a binocular state and encourage more natural binocular connections.3
So far, vision therapy has not been evaluated in randomized clinical trials.13 PEDIG considered a clinical trial and completed a pilot randomized controlled trial of office-based active vision therapy. Unfortunately, there was insufficient recruitment and difficulties with assessing home therapy. PEDIG concluded that a successful clinical trial would need broader eligibility requirements, better methods to assess home therapy and the ability to customize vision therapy based on patient data.13
Some studies have looked at perceptual activities with amblyopic children and adults. Perceptual learning studies in children show improvement in visual acuity and contrast sensitivity. Similar improvement was observed when comparing perceptual learning with patching in children. However, perceptual learning required less treatment time to achieve similar results.14,15 Additionally, a growing number of studies suggest a substantial plasticity in the visual system of adults with amblyopia. Perceptual learning techniques with adults show improvement with visual detection, stereo information and contrast sensitivity function.14-16
Many case reports demonstrate that vision therapy works for treating amblyopia in adults and children.17,18 While amblyopia treatment has a decreased effect for adults compared with children, documented case reports show improvement of vision and binocular function after treating adult amblyopes with vision therapy.2,3
The goals for amblyopia therapy should not be based solely on visual acuity, but also on the function of the binocular system. Amblyopia treatment should not be considered complete until the visual acuity of the amblyopic eye is normalized under binocular viewing conditions.8 To achieve good binocular vision after amblyopia treatment has stopped, it is important to treat all aspects of the binocular system.12 With this therapy approach in mind, practitioners can be confident their patients with amblyopia will receive the best care and achieve the best visual outcomes.
Dr. Tison is an assistant clinical professor and chief of pediatrics at the University of the Incarnate Word Rosenberg School of Optometry. She is an attending doctor in the Pediatrics, Vision Therapy and Primary Care Clinics.
Dr. Nicklas is a staff optometrist at St. Louis Children’s Hospital in the department of Ophthalmology and Visual Sciences. She is residency trained in pediatrics and vision therapy.
1. Braverman RS. Introduction to Amblyopia. American Academy of Ophthalmology. 2015. www.aao.org/pediatric-center-detail/amblyopia-introduction. Accessed August 24, 2017. |

