 |
A 73-year-old Hispanic female presented with blurry vision and distortion in her right eye, which she said began about five years earlier. She reported a slow, steady progressive loss of vision in that eye. The left eye is near-perfect with only mild blurry vision but no distortion. Her past ocular history is unremarkable. Her medical history is significant for hypertension, for which she takes medication.
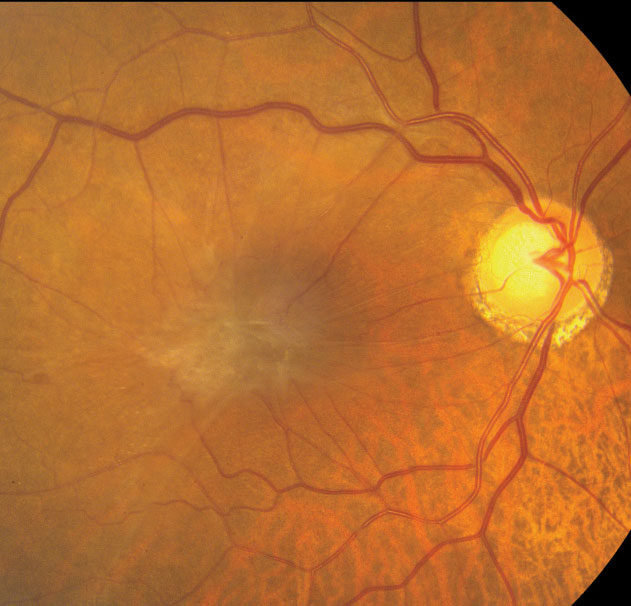 |
| Fig 1. This fundus photo shows the right eye of our patient. Can you spot the changes to the macula? |
On examination, her best-corrected visual acuity was 20/80 OD, 20/20 OS. Extraocular motility testing was normal. Her confrontation visual fields were full-to-careful finger counting and the pupils were equally round and reactive; there was no afferent pupillary defect. An Amsler grid showed a large area of central distortion in the right eye. Her anterior segments were remarkable for 1+ nuclear sclerotic cataracts OU. Tensions by applanation measured 14mm Hg OU.
On dilated fundus exam, she had large optic nerves and moderate-sized cups with good rim coloration and perfusion in both eyes. The macula in the right eye showed changes, however (Figure 1). Optical coherence tomography angiography (OCT-A) and spectral domain OCT were also performed (Figures 2 and 3). The peripheral was normal.
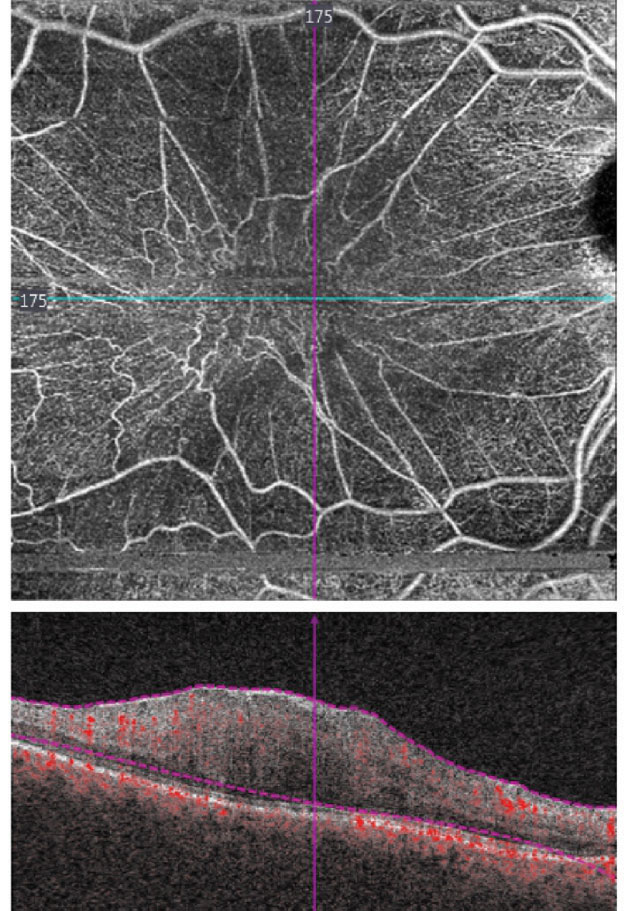 |
| Fig 2. What do these OCT angiography images reveal about the patient’s vision? |
Take the Retina Quiz
1. What does the SD-OCT show of the outer retinal layers?
a. Normal IS/OS junction.
b. Atrophy and loss of the photoreceptor interior and outer segment junction.
c. Choroidal neovascularization.
d. Ganglion cell loss.
2. What does the OCT-A show?
a. Extensive leakage of the retinal arteries and veins.
b. Extensive capillary dropout and ischemia.
c. Distortion and dragging of the retinal vasculature but no leakage.
d. Intraretinal neovascularization.
3. What is the correct diagnosis?
a. Epiretinal membrane.
b. RPE hamartoma.
c. Wet AMD with CNV.
d. VMT with macular edema.
4. What other findings do you expect to be present on your clinical exam?
a. Cystoid macular edema.
b. Posterior vitreous detachment.
c. Macular hole.
d. Peripheral retinal tear.
5. How should she be managed?
a. Observation.
b. Intravitreal anti-VEGF medication.
c. Intravitreal injection ocriplasmin.
d. Referral for pars plana vitrectomy and membrane peel.
For answers, see below.
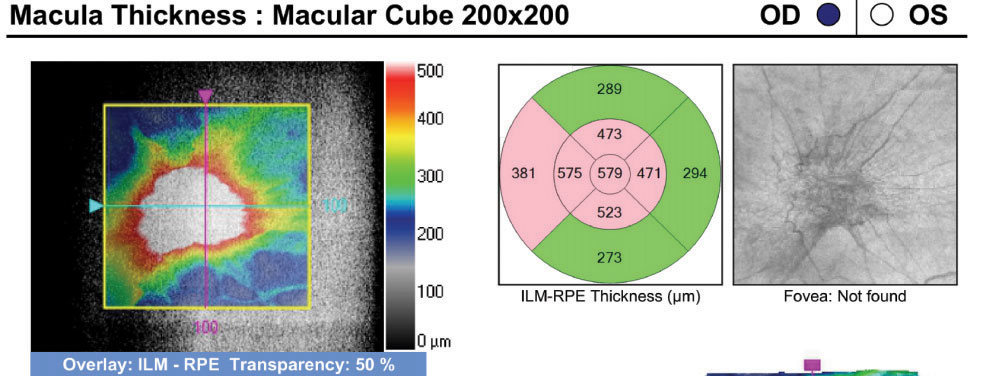 |
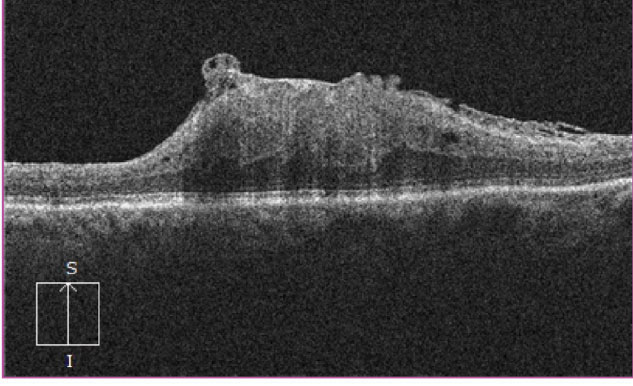
| Fig. 3. How can these OCT images of the patient’s right eye illuminate the etiology behind her visual distortion? |
Discussion
Our patient has a significant epiretinal membrane (ERM) in the right eye causing reduced acuity and central distortion of her vision. On the SD-OCT, we observed a complete loss of foveal depression and significant retinal elevation of the macula. The thickness map of the right eye measures 579µm of elevation compared with the normal thickness of 234µm in the fellow eye. Interestingly, we saw no intraretinal fluid or cystoid macular edema as one might expect with an ERM of this size. What’s more, the photoreceptor interior and outer segment (IS/OS) junction appears intact.
ERM are most commonly seen in the elderly population.1 In autopsy eyes, it was present in 20% of subjects older than 75 and in only 4% younger than 60.1 An ERM represents a fibrocellular member that grows on the surface of the retina. The membrane is made up of glial cells, retinal pigment epithelial cells, macrophages, fibrocytes and collagen cells.2 The initiating event in the development of most ERMs is often a posterior vitreous detachment (PVD). The traction on the retina from the PVD results in a small break or dehiscence in the ILM that starts the cascade. Therefore, it’s not surprising that up to 90% of patients with ERMs also have PVD.1 Our patient also had a PVD that was easily seen on clinical exam, which was purposely not disclosed. Other causes of PVD include uveitis, trauma and prior intraocular surgery.
Often, the highly reflective membrane can be easily observed on the inner surface of the retina on OCT. In our patient, it was not so easy to see on the horizontal line scan, probably because it is so tightly adherent to the retina. However, on the transverse cut, we see a lot of superficial irregularities that stand out.
Most ERMs will remain stable and not affect visual function to any great extent. Population studies show that 16% to 33% of patients with ERM will progress. For those patients who develop symptomatic ERM, pars plana vitrectomy with membrane peel is the treatment of choice. Surgical success is dependent on the extent and severity as well as the level of the visual acuity.
 |
Treatment
No definitive standard describes when surgery is recommended for ERM. For the majority, it is based on symptoms. If patients are asymptomatic, most surgeons elect to observe. When symptoms become intolerant or begin to affect quality of life, surgery is recommended. The SD-OCT may provide a good barometer for detecting structural changes within the retina, either at the level of the IS/OS junction or if patients develop fluid or cystic changes within the retina. Once this occurs, most retina specialists agree that surgery is warranted.
Generally speaking, better visual outcomes are achieved when there is better preoperative vision. The expectation for recovery of visual acuity following surgery is considered to be approximately 50% of what their preoperative acuity was. For example, patients with 20/60 acuity from an ERM would expect to achieve at least 20/30 or better as a final outcome.
Regardless of the preoperative acuity, most patients will achieve some level of improvement. In one study, 70% of ERM patients had improvement in visual acuity and over half achieved vision better then 20/40.1 Even though VA may remain unchanged for some patients after surgery, the perceived visual quality may be much better due to improvement in patients’ metamorphopsia.
Our patient did not have any cystoid macular edema and the IS/OS junction was intact so we were optimistic that PPV and MP would offer her the best chance for improving vision and providing relief of her metamorphopsia. However, given the size and density of the ERM, we were cautious on just how much she would improve. She elected to proceed with pars plana vitrectomy and membrane peel. One month following the surgery, her acuity improved to 20/40 and her metamorphopsia was much better. She is scheduled for a follow up exam in four to six weeks.
1. Dawson SR, Shunmugan M, Williamson TH. Visual acuity outcomes following surgery for idiopathic epiretinal membrane: an analysis of data from 2001 to 2011. Eye. 2014;28:219-24. 2. Smiddy W, Maguire A, Green W, et al. Idiopathic epiretinal membranes. Ultrastructural characteristics and clinicopathologic correlation. Ophthalmology. 1989;96(6):811-20. |

