Eight-year-old Olivia reports to your clinic for the first time with her 6-year-old sister and her mother. Her referring doctor’s letter explains that her refractive error was -2.50DS OD/OS. He also indicates that the patient had no binocular vision or ocular health issues.
You begin your myopia management consult by giving your patient and her family an in-depth overview of your services while you walk them through your consent form. You specifically start by defining myopia as a condition that typically results from the eye being too long for its refractive components, which is known as axial myopia.
Myopia is less commonly refractive in nature, though refractive myopia can occur and if it does it typically results from the corneal power or lenticular power being too strong for the eye.1 This refractive status typically results in distance blur because a distance image is focused in front of the retina. While describing the condition—commonly known as nearsightedness—you make use of an eye model and ensure that everyone understands the anatomical basics.
You elaborate, explaining that myopia affects approximately one third of Americans and that the condition is likely caused by a mix of genetic, lifestyle, and environmental factors.2-4 You also clearly tell your young patient that anyone has a chance of becoming myopic and that she should not at all feel bad about the need to wear glasses.
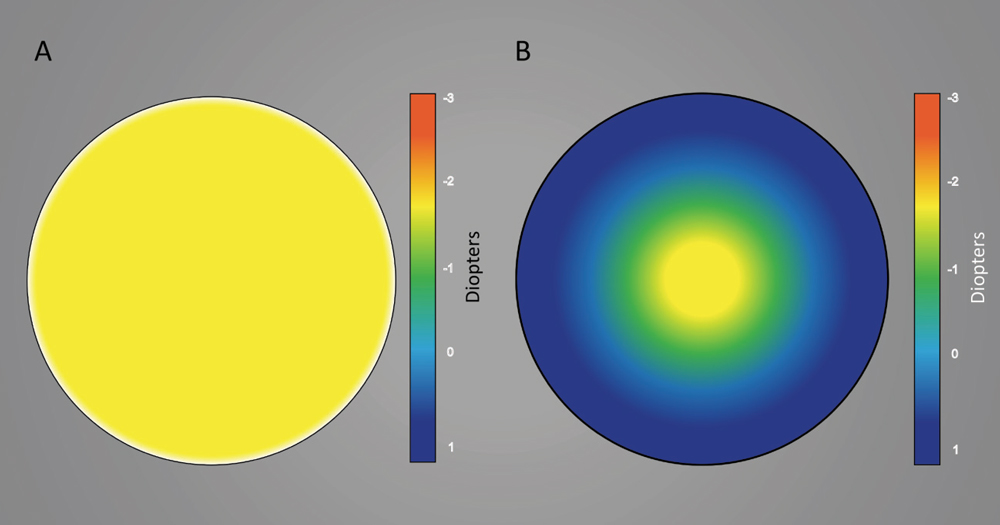 |
| This graphic shows representations of (A) a spherical contact lens and (B) a center-distance multifocal contact lens. Image: Keyur Savla, BS. Click image to enlarge. |
You notice that Olivia’s mother was also wearing glasses, and you ask if her father wears does, too. Olivia’s mother says no. You explain that anyone has a chance of becoming myopic, even children without myopic parents. However, having one myopic parent makes a child approximately twice as likely to develop myopia and those with two myopic parents are approximately five times more likely.5 You also explain that the prevalence of myopia has increased in recent years and that this is likely because of environmental factors such as people spending less time outdoors.5,6
At this point, Olivia’s mother asks if there is anything that she can do to help prevent her younger daughter from developing myopia. While research shows that approximately two hours per day outdoors may be able to stave off myopia development in at-risk patients, outdoor time has minimal effect on patients who have already developed myopia.7
However, you have good news for Olivia’s mother. You happen to provide special interventional techniques—namely low-dose atropine, overnight orthokeratology and multifocal soft contact lenses.1 These treatments are designed to slow the progression of myopia. By reducing Olivia’s overall refractive error, you hope to not only decrease her dependence on glasses and contact lenses, but also lower her risk of conditions such as glaucoma or a retinal detachment.8
These three techniques represent some of the latest developments in slowing myopia progression.
Atropine
Meta-analysis data indicates that 1% atropine can safely treat amblyopia and is also likely safe for myopia management.9 Atropine has also been used to slow myopia progression for years, though habitual use of 1% atropine results in photophobia and reduced accommodative ability.10
More recent research found that 0.01% atropine is able to slow myopia progression with minimal accommodative or photophobic side effects.10 They specifically found that when 0.01% atropine was compared with 1.0% atropine for slowing myopia progression that 1.0% atropine was able to slow refractive error progression to a greater degree than 0.01% atropine; however, when subjects stopped drops, the 1.0% atropine group’s eye growth rebounded, negating the majority of its treatment effect while the 0.01% atropine group had limited rebound, which resulted in an effective myopia management method (slowed refractive error progression by 59%).10,11
This seminal study has since been criticized for using a historical control group and for having minimal effect on axial length progression in the low dose atropine group.11 Nevertheless, another recent study shows that 0.025% and 0.05% atropine appear to have a clinically meaningful effect on both axial length and refractive error.12 While research shows the side effects with low-dose atropine are minimal, administering the drops before bed could further mitigate any potential side effects.10
The mechanism by which atropine slows eye growth is currently unknown. In the United States, low-dose atropine can only be obtained from a compounding pharmacy. Atropine can be used on even your youngest patients because parents can apply the drops.
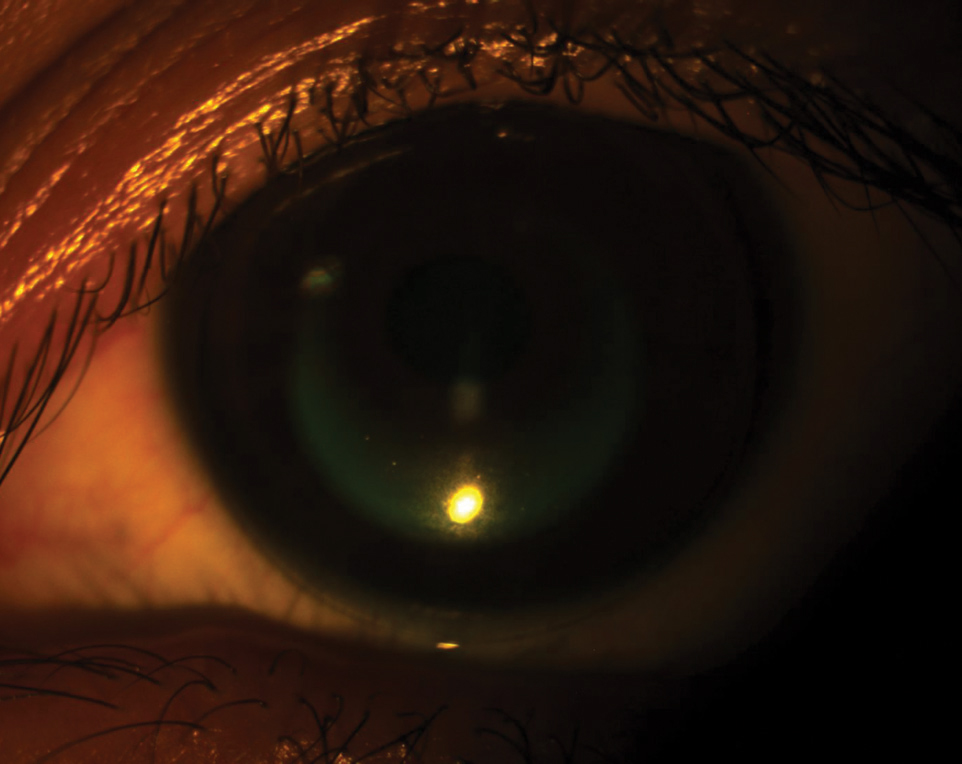 |
| This patient demonstrates a well-fit orthokeratology lens. Click image to enlarge. |
Orthokeratology
This technology was developed to mitigate daytime myopic refractive error. The lenses are worn while sleeping. When they are removed, the patient, ideally, should be able to see clearly at distance after corneal reshaping has taken full effect.1 Many patients can achieve full correction within about one week, though this does vary by the patient’s starting refractive error.1 Since the patient will have a refractive error that progressively decreases during the initial adaption period, patients should be given a series of daily disposable contact lenses with lessening powers to make up the refractive error difference. Daily disposable power should be selected based upon the patient’s refractive error after one night’s wear. Orthokeratology is now commonly used to slow myopia progression and researchers believe that it works by reducing the patient’s amount of peripheral hyperopic defocus.1
Our understanding of orthokeratology’s mechanism is largely based upon researchers who first laser ablated the fovea of the right eyes of Rhesus monkey while at the same time not damaging their left eyes.13,14 They then applied a myopia stimulus to each eye (experiment one used form deprivation/cloudy lenses while experiment two used minus lenses), and found they were still able to induce myopia in both eyes.13,14 These experiments subsequently suggested that the fovea was not essential for regulating refractive error development and that the peripheral retina may be more important for regulating emmetropization.
Investigators now believe orthokeratology can slow myopia progression by approximately 50%.15-17 However, only a limited range of refractive errors are approved by the FDA for the correction of myopia (typically better than -6.00D of sphere power and 1.50D of cylinder power). Patients need to be mature enough to apply contact lenses to use orthokeratology, though these lenses are typically worn in the home, so parents can help with this technology.
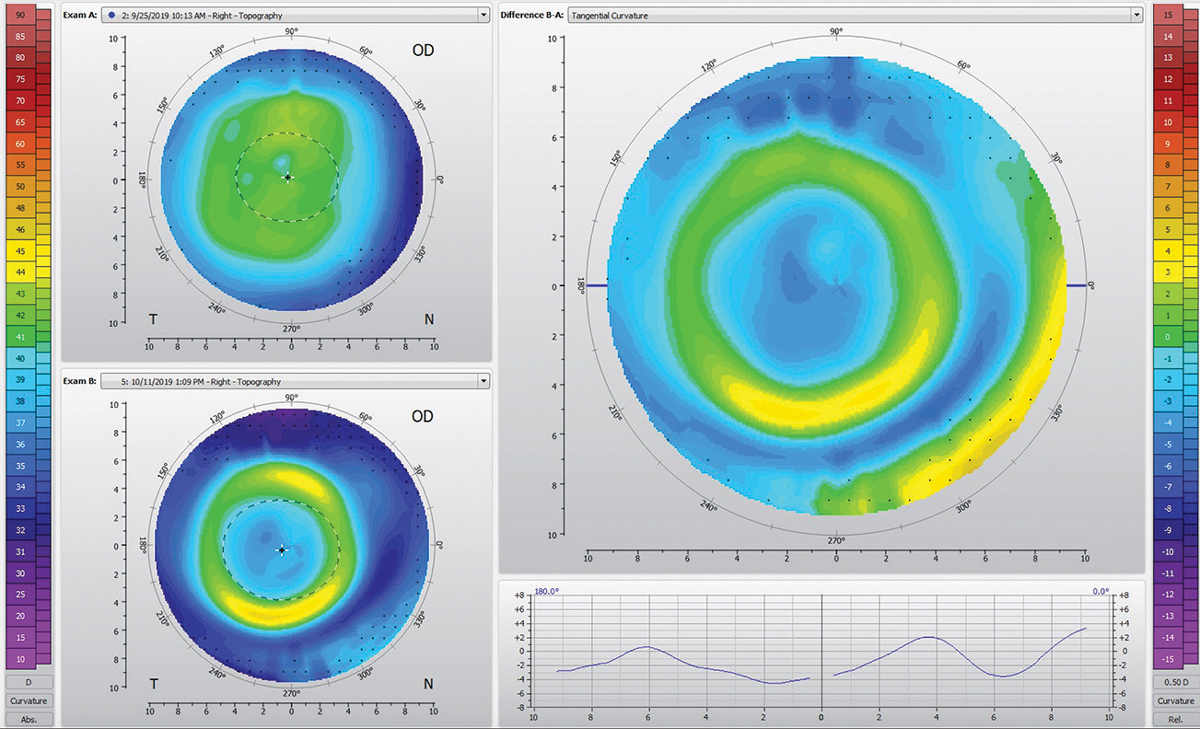 |
| This topography shows a well-fit orthokeratology lens. Click image to enlarge. |
Multifocal Soft Contact Lenses
Multifocal contact lenses were originally designed for correcting presbyopia, though soft multifocal lenses are now commonly used to manage myopia progression. Researchers believe center-distance, or extended depth-of-focus multifocal contact lenses, can slow myopia progression much like orthokeratology lenses, by reducing peripheral hyperopic defocus.18,19
The efficacy of multifocal contact lenses varies greatly by study, though the data again suggest that these soft contact lenses are able to slow myopia progression by approximately 50%.20,21
Multifocal contact lenses formally studied have been limited to spherical designs; however, in my experience, many people who have clinically meaningful astigmatism are still interested in trying contact lens-based myopia management. I’ve found that patients can be successfully fit in custom soft, multifocal, toric contact lenses.
Children who use soft contact lenses need to show an elevated level of responsibility and be able to fully care for the contact lenses outside the home. Parents are frequently concerned that contact lenses are unsafe for young children, but research actually suggests that this younger age group is at a lower risk of developing a contact lens complication compared with college age adults, and both groups may find social benefit from wearing contact lenses.22
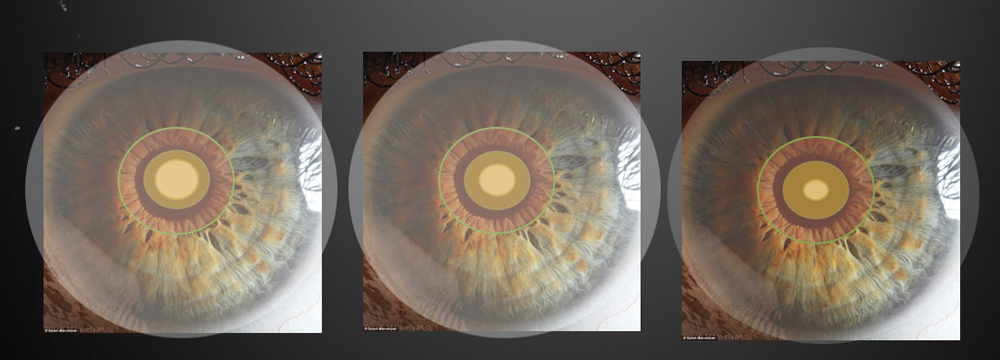 |
This series shows various multifocal zone sizes within a pupil. Photos: Robert L. Davis, OD. Click image to enlarge. |
Work Up
After discussing all of the options with Olivia and her mother, you indicate that you will not be able to fully determine what treatment option will work for Olivia until after you complete your myopia management evaluation. They agree to complete the evaluation, and you talk to Olivia to understand her visual needs. During this discussion, Olivia tells you she is an avid swimmer. You also evaluate her visual acuity, cover test at distance and near, accommodative amplitudes, pupil size, cycloplegic refractive error, corneal topography with a horizontal visual iris diameter measurement and axial length with non-contact biometry.
Binocular vision testing can help monitor atropine side effects and determine if a near add may cause multifocal contact lens wearers to decompensate. Refractive error and axial length testing are intended to monitor the patient’s myopia progression, and topography is necessary to order specialty contact lenses.23
After fully evaluating Olivia, you conclude that she could be a good candidate for all three myopia management options. Since she is motivated to wear contact lenses and because she is a swimmer, you determine that orthokeratology may be the best option for her lifestyle (lower risk of developing an eye infection compared to soft contact lenses).
A Historical Perspective on Myopia “Control”By Paul Harris, OD Since the early days of A.M. Skeffington and the Optometric Extension Program, optometry had in its grasp a systematic examination and analysis system for understanding how function alters structure over time. Only now, through modern research, are the actual physiological mechanisms being revealed. However, the observations and associations, and in particular the clinical experience of seeing results of patients over many years of follow-up, at least suggested that myopia could be controlled. In those days, the term, “myopia control” referred to the application of lenses, at both distance and near, to guide the development of future refractive changes to either being stable (no new myopia added on over time) or to reduce the need for minus sphere powers at distance to restore standard visual acuity. Every optometrist who followed these guidelines took the time to take the extended data, reviewed patterns in the findings and performed some form of near-point retinoscopy, were then able to prescribe lenses that afforded a degree of myopia control. These same optometrists knew when they had little leeway to prescribe something other than what they measured, and then knew that the only way to stabilize progressive, or as it was called then “school myopia,” was to institute vision therapy, with emphasis in the areas of accommodation. This approach was fundamental to the teaching of Skeffington, Leo Manas, Nat Flax, Bill Ludlam and many other optometric luminaries over the years. While newer treatment methods such as low-dose atropine, orthokeratology lenses and soft multifocal contact lenses certainly show where optometry can go, it would do all a service to continue to include techniques which are a part of our heritage, and that many optometrists in the United States and worldwide continue to provide. When I teach about this more basic, fundamental approach at Southern College of Optometry, I call it “refractive engineering.” It seems to garner more interest when spoken about that way. The newer usage of the term “myopia control” seems to not be evolutionary, because the older methods all still work. Those new methods are here to supplement, not replace. At worst, I’m concerned that overreliance on today’s conception of myopia control could, one day, lead to a lack of exposure to the evidence base of traditional lens prescribing. My appeal to the profession is for us to remember our roots and not to cease to promulgate the knowledge and clinical acumen on which these advancements were built. |
You thoughtfully explain that Olivia will need to use her selected myopia intervention for several years to obtain clinically meaningful results. You prep her to anticipate the natural fall-off in motivation she’ll experience at some point, as the effort doesn’t “fix” her myopia—only helps slow it down. You let her know you and her parents are in this for the long haul with her. No one knows when myopia progression will stop, though I recommend using myopia management for as long as possible since research shows some patients’ eyes continue to grow into their 20s.24
When Olivia’s family decides to move forward with orthokeratology, you schedule Olivia for a dispense visit. There, you perform a normal orthokeratology lens evaluation, and you find that each lens yields a perfect bull’s eye pattern with 20/20 acuity OD/OS. You next fully educate Olivia and her mother on how to apply, remove and care for the lenses and you see her the following morning. At the next morning visit, Olivia presents without the lenses on with 20/30 visual acuity OD/OS and a -1.00 refraction OD/OS. The lenses also appeared well-centered via topography. You then provide Olivia with a set of -1.00DS and -0.50DS daily disposable soft contact lenses. You evaluate the lenses, and you send her home with the lenses after teaching her how to use them.
You next see Olivia again at one week, and you find that she is plano DS OD/OS at the end of the work day and that she has 20/20 visual acuity OD/OS with well-centered lenses as evaluated with topography. You subsequently find the same positive outcomes at one month and six months, and you find at six months when you repeat your full myopia management work up that Olivia has had minimal refractive error or axial length progression.
You then recommend at this point that Olivia should be monitored every six months with lens adjustments only made as needed. You also indicate that if Olivia shows signs of progression that you would consider adding atropine to the treatment plan because it has been found to provide additional slowing in a recent randomized clinical trial.25
Applying these myopia control techniques can be rewarding because you have the potential to preserve the quality of a patient’s vision. However, it is also challenging because myopia management is new to many regions of the United States. Therefore, it may be best to begin offering these services by recruiting patients from your own practice. The ideal patient is one who is getting their first pair of glasses because such a patient has potential to gain the most cumulative benefit.
Dr. Pucker is an assistant professor at the University of Alabama at Birmingham.
| 1. Smith MJ, Walline JJ. Controlling myopia progression in children and adolescents. Adolesc Health Med Ther. 2015;6:133-140. 2. Wu P, Huang H, Yu H, et al. Epidemiology of myopia. Asia-Pacific J Ophthalmol. 2016;5(6):386-93. 3. Wojciechowski R. Nature and nurture: the complex genetics of myopia and refractive error. Clin Genet. 2011;79:301-20. 4. Vitale S, Ellwein L, Cotch MF, Ferris FL, 3rd, Sperduto R. Prevalence of refractive error in the United States, 1999-2004. Arch Ophthalmol. 2008;126:1111-1119. 5. Jones LA, Sinnott LT, Mutti DO, et al. Parental history of myopia, sports and outdoor activities, and future myopia. Invest Ophthalmol Vis Sci. 2007;48:3524-3532. 6. Rose KA, Morgan IG, Ip J, et al. Outdoor activity reduces the prevalence of myopia in children. Ophthalmology 2008;115:1279-1285. 7. Xiong S, Sankaridurg P, Naduvilath T, et al. Time spent in outdoor activities in relation to myopia prevention and control: a meta-analysis and systematic review. Acta Ophthalmol. 2017;95:551-66. 8. Flitcroft DI. The complex interactions of retinal, optical and environmental factors in myopia aetiology. Prog Retin Eye Res. 2012;31:622-660. 9. Li T, Shotton K. Conventional occlusion versus pharmacologic penalization for amblyopia. Cochrane Database Syst Rev. 2009;CD006460. 10. Chia A, Chua WH, Wen L, Fong A, Goon YY, Tan D. Atropine for the treatment of childhood myopia: changes after stopping atropine 0.01%, 0.1% and 0.5%. Am J Ophthalmol. 2014;157:451-457 e451. 11. Bullimore MA, Berntsen DA. Low-dose atropine for myopia control: considering all the data. JAMA Ophthalmol. 2018;136:303. 12. Yam JC, Jiang Y, Tang SM, et al. Low-concentration atropine for myopia progression (LAMP) study: a randomized, double-blinded, placebo-controlled trial of 0.05%, 0.025%, and 0.01% atropine eye drops in myopia control. Ophthalmology. 2019;126:113-124. 13. Smith EL, 3rd, Ramamirtham R, Qiao-Grider Y, et al. Effects of foveal ablation on emmetropization and form-deprivation myopia. Invest Ophthalmol Vis Sci. 2007;48:3914-22. 14. Smith EL, 3rd, Hung LF, Huang J. Relative peripheral hyperopic defocus alters central refractive development in infant monkeys. Vision Res. 2009;49:2386-2392. 15. Aller T, Wildsoet C. Optical control of myopia has come of age: or has it? Optom Vis Sci. 2013;90:e135-137. 16. Cho P, Cheung SW, Edwards M. The longitudinal orthokeratology research in children (LORIC) in Hong Kong: a pilot study on refractive changes and myopic control. Curr Eye Res. 2005;30:71-80. 17. Walline JJ, Jones LA, Sinnott LT. Corneal reshaping and myopia progression. Br J Ophthalmol. 2009;93:1181-1185. 18. Berntsen DA, Kramer CE. Peripheral defocus with spherical and multifocal soft contact lenses. Optom Vis Sci. 2013;90:1215-1224. 19. Cooper J, O’Connor B, Watanabe R, et al. Case series analysis of myopic progression control with a unique extended depth of focus multifocal contact lens. Eye Contact Lens. 2018;44:e16-e24. 20. Walline JJ, Greiner KL, McVey ME, Jones-Jordan LA. Multifocal contact lens myopia control. Optom Vis Sci. 2013;90:1207-1214. 21. Anstice NS, Phillips JR. Effect of dual-focus soft contact lens wear on axial myopia progression in children. Ophthalmol. 2011;118:1152-1161. 22. Chalmers RL, Wagner H, Mitchell GL, et al. Age and other risk factors for corneal infiltrative and inflammatory events in young soft contact lens wearers from the Contact Lens Assessment in Youth (CLAY) study. Invest Ophthalmol Vis Sci. 2011;52:6690-6696. 23. Walline JJ. Myopia Control: A Review. Eye Contact Lens. 2016;42:3-8. 24. Group C. Myopia stabilization and associated factors among participants in the Correction of Myopia Evaluation Trial (COMET). Invest Ophthalmol Vis Sci. 2013;54:7871-7884. 25. Kinoshita N, Konno Y, Hamada N, Kanda Y, Shimmura-Tomita M, Kakehashi A. Additive effects of orthokeratology and atropine 0.01% ophthalmic solution in slowing axial elongation in children with myopia: first year results. Jpn J Ophthalmol. 2018;62:544-553. |

