 |
Q: Have you ever treated a patient who had molluscum virus? How do you treat the ophthalmic concerns of such a patient?
A: A patient with molluscum contagiosum recently presented to our practice. She is a 21-year-old black female who reported redness, itching, tearing and burning for the previous three weeks. She said most of her symptoms were in her left eye but also occasionally occurred in her right.
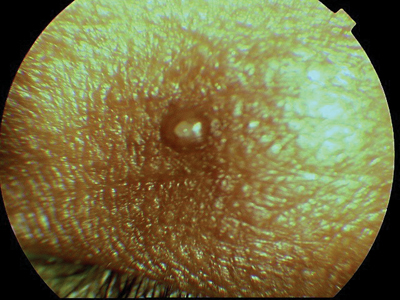
Upon examination, she had follicular conjunctivitis and punctate keratopathy, says Gerald W. Koss II, O.D., resident in ocular disease at Omni Eye Services, in Atlanta, who first examined her. On the adnexae around the eyes were multiple lesions characteristic of molluscum. These skin lesions are papular eruptions that are characteristically smooth and dome-shaped with an umbilication (i.e., indentation) in the center, Dr. Koss says. The umbilication has a waxy or cheese-like appearance, and the edges are pearlescent.
The lesions are usually 2mm to 4mm in size. But in immunocompromised patients, such as those with HIV, lesions can grow to more than a centimeter and can greatly increase in number, he says.
The lesions frequently appear in the eyelid margin, which can shed viral particles into the eye. This produces a follicular conjunctival response and epithelial keratitis. So, when the patient scratches the lesions, it can worsen the eye condition, Dr. Koss says. If the follicular conjunctivitis or punctate keratopathy are chronic, they can lead to more serious complications of pannus and conjunctival scarring.
 |
 |
|
Molluscum contagiosum lesions often appear on the lid margin (above) or elsewhere around the eye (below). |
Estimates of the worldwide incidence are 2% to 8%, with less than 5% of children in the United States infected.1 During the last 30 years, the incidence has increased, mainly through sexual transmission and particularly as a result of concurrent HIV infection.2 Between 5% and 20% of patients with HIV have symptomatic molluscum contagiosum virus.3,4
The condition is self-limiting, usually with an incubation period of two to seven weeks, Dr. Koss says. But the lesions can last up to a year before they finally disappear, and the patient is contagious all that time.
Dr. Koss treated this patients eye condition with Vigamox (moxifloxacin, Alcon) q.i.d. O.U. to stave off a secondary bacterial infection, along with Refresh Liquigel (Allergan) q1-2 hours. I also provided a lot of information about hygiene and the contagious nature of the pathogen, he says.
Q: Must the optometrist also refer the patient to a dermatologist or general practitioner?
A: Not usually. Well see her every week for about two to four weeks while we let the virus run its course, Dr. Koss says. However, if the lesions increase in size or in number during that time, well definitely send her for a workup and an HIV test.
If the patient scratches or worries the lesions, or is particularly concerned about her appearance, then she can be referred to a dermatologist who can remove the lesions.
1. Billstein SA, Mattaliano VJ Jr. The nuisance sexually transmitted diseases: molluscum contagiosum, scabies, and crab lice. Med Clin North Am 1990 Nov;74(6):1487-1505.
2. Becker TM, Blout JH, Douglas J, Judson FM. Trends in molluscum contagiosum in the United States, 1966-1983. Sex Transm Dis 1986 Apr-Jun;13(2):88-92.
3. Schwartz JJ. Myskowski PL. Molluscum contagiosum in patients with human immunodeficiency virus infection. A review of twenty-seven patients. J Am Acad Dermatol 1992 Oct;27(4):583-8.
4. Lombardo PC. Molluscum contagiosum and the acquired immunodeficiency syndrome. Arch Dermatol 1985 Jul;121(7):834-5.

