 |
Q:
I struggle with recommending scleral lenses following penetrating keratoplasty (PK); virtually all of my patients experience significant edema with prolonged wear. How can I maximize corneal oxygen flux and minimize edema and premature endothelial cell attrition with these lenses?
A:
“Post-PK patients are great scleral lens candidates, but their eyes are delicate and require careful consideration during the fitting process to ensure optimal corneal and graft health,” according to Andrew Fischer, OD, of Professional Eyecare Associates in Indiana. “We must minimize the risks that scleral lens wear may pose to these corneas.” These include corneal edema and endothelial cell attrition, which could ultimately lead to graft failure.
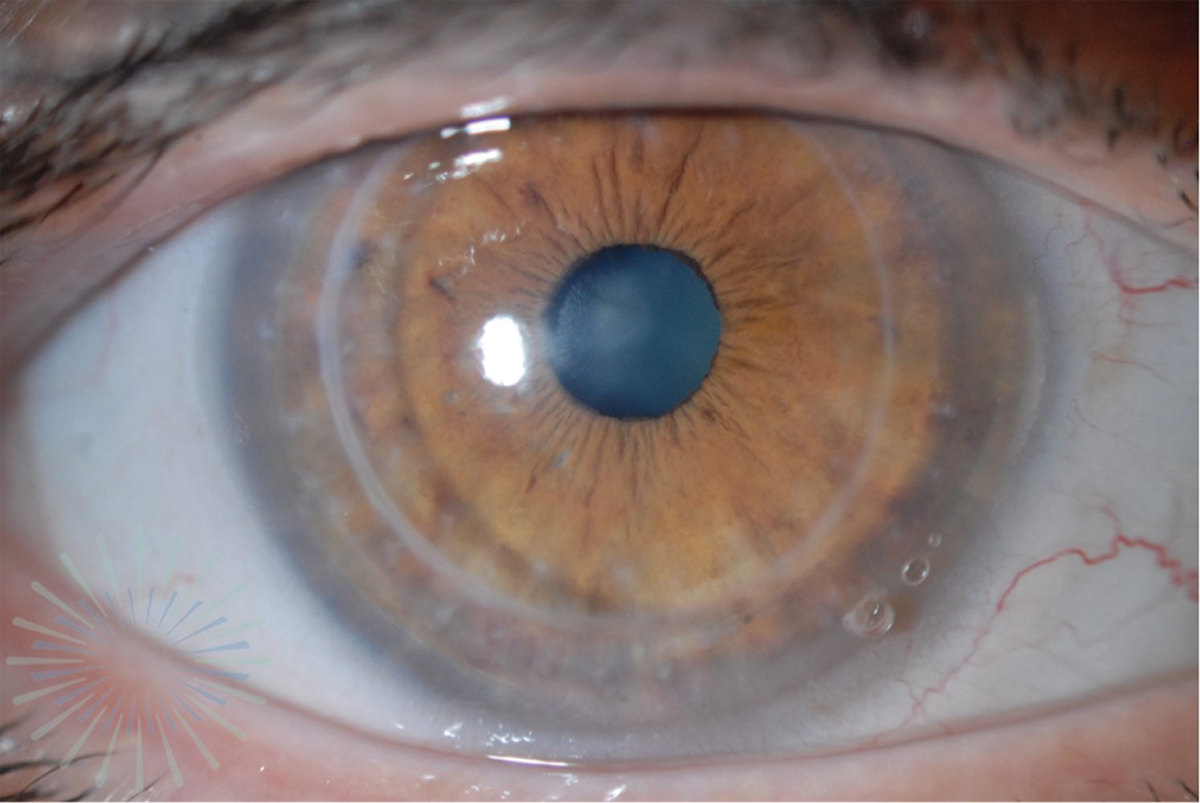 |
| A large-diameter scleral lens with a fenestration at 4 o’clock is fit on a post-PK patient. Photo by Kellen Riccobono, OD. Click image to enlarge. |
Parts of the Whole
When picking a lens, Dr. Fischer suggests first considering oxygen permeability. He notes that there are many gas permeable (GP) lens materials, with some of the newest achieving ratings over 160Dk. For post-transplant corneas, his motto is the more permeable the lens, the better.
Lens thickness also plays a role in oxygen transmission to the cornea, Dr. Fischer adds. His strategy is to ask his consultants to produce the lens he needs in a more permeable material and cut it with a thinner central thickness to help with oxygen flow. Additionally, minimizing lens clearance over the cornea can help maximize corneal health. Dr. Fischer typically aims for 100µm to 150µm of clearance for post-graft eyes. Many lens designs offer quadrant-specific customization, which gives even the most irregular corneas a suitable post-lens tear lake.
The next step is choosing the lens design. Dr. Fischer has found success with larger and looser lenses, which tend to be more stable on the eye and help minimize edema. If a patient experiences irritation and/or scratching, the lens is too loose.
Especially for post-graft corneas, Dr. Fischer is mindful of ensuring the lens is not excessively tight with zero tear exchange, as this reduces oxygen to the cornea. To check oxygen supply after the lens settles on the eye, he uses a fluorescein strip to “paint” the front surface of the lens under cobalt blue light and Wratten filters. He specifies that a small amount of tear flow is ideal and indicates there is oxygen flux under the lens, not just through the GP material.
While recent innovations may make this practice unnecessary, Dr. Fischer says lens fenestrations—small holes drilled through a lens to allow surface tears to exchange with the post-lens tear layer—can help promote increased tear and oxygen transfer. He advises patients who he fits with looser edge profiles or fenestrated lenses that they may occasionally experience mid-day fogging and that removing, refilling and reinserting the lenses may be necessary for optimal clarity.
Dr. Fischer cautions not to overlook elevated intraocular pressure (IOP) as a potential stressor on endothelial cells and corneal grafts. Unfortunately, he acknowledges that obtaining accurate IOP measurements in cases of corneal transplant patients can be difficult due to severe irregularity, varying pachymetry values and the presence of corneal edema. Dr. Fischer speculates that scleral lenses may elevate IOP during wear, though it is hard to assess to what extent. For patients who experience edema with scleral lenses, he highlights IOP-lowering medications as a possible solution to decrease endothelial stress.
“Scleral lenses are ideal for most eyes after a PK; they maximize vision, minimize the risk of mechanical rubbing forces from the lens and make long-term graft success more attainable,” concludes Dr. Fischer. Optimizing the fit with state-of-the-art materials and designs, and monitoring the eye, are vital to endothelial health, he emphasizes. However, in some cases, he warns that the endothelium may not be robust enough to keep a graft edema-free and a consultation for endothelial transplant may be the best option.

