 |
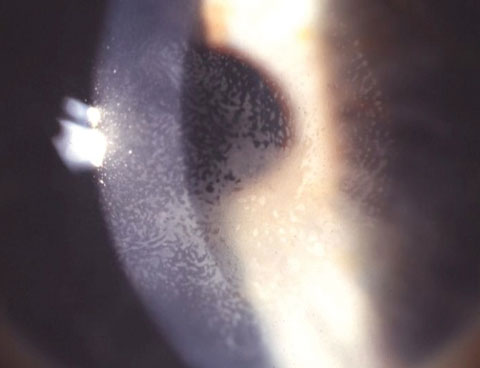
| Overlooking an inferior nerve fiber layer defect such as this could lead to litigation for failure to diagnose. Click image to enlarge. |
The general principles of how to protect yourself apply no matter the circumstances. However, the top three allegations all concern claims of lapses in diagnostic services, making this aspect of care particularly significant, especially given optometry’s role as the first point of contact for many patients. According to the National Provider Data Bank, the most common allegation in optometric malpractice—more than 35% of cases—is failure to diagnose.1 The next four most common allegations are delay in diagnosis, wrong or misdiagnosis, improper management and failure/delay in referral or consultation. In total, these five allegations account for two-thirds of all cases.1 Recent articles suggest glaucoma, retinal detachment and tumors are the conditions underlying most optometric malpractice claims.4-6
This article discusses how you can minimize your risk against malpractice in general, with emphasis on the optometrist’s role as diagnostician and initiator of an episode of care. Remember that a missed diagnosis in and of itself does not constitute malpractice, just as a correct diagnosis does not dispel medicolegal risk. Rather, perceived negligence with resulting damages is what triggers a claim.
Poor Outcomes Don’t Always Equal Malpractice |
| In a malpractice suit, the plaintiff is burdened with establishing four criteria: duty for the doctor to render care to the patient, negligence (i.e., breach of the standard of care), damages or injury (i.e., vision loss, disfigurement, disability) and a causal relationship between the negligence and damages. Suppose you diagnose bilateral amblyopia in a patient who is nearly emmetropic with 20/40 BSCVA. Four years later, the patient has light-perception vision in each eye and is diagnosed with retinitis pigmentosa by another doctor. Although you did not meet the standard of care by offering a logical diagnosis and the patient experienced visual damage leading to light-perception vision, there would not be proximate cause. Had you correctly diagnosed retinitis pigmentosa, the visual outcome would have been the same, since there currently is no effective treatment. Hence there would not be malpractice for failure to diagnose. |
Evolving Standard of Care
With scope of practice expansion and an ever-widening array of diagnostic modalities and treatments, standard of care is a moving target. It’s generally established by an expert witness who describes what a reasonably prudent practitioner would have done under a similar circumstance. This can often make or break a case, so it’s important your counsel selects the right individual with respect to background, experience and reputation.
“Standard of care can even be changed by a single judge in the event of litigation, as in Helling v. Carey, where the care given was well within the medical standard at the time, but the judge, in his ruling, literally changed the standard with his decision, i.e., requiring tonometry on patients even under age 40 since the test is inexpensive and harmless,” says Pamela Miller, OD, JD, of Highland, Calif.
For example, we may see an increase in suits regarding missed or delayed diagnosis of progressive keratoconus and post-LASIK ectasia due to the evolving standard of care created by the approval of the first corneal collagen crosslinking (CXL) system. Designed to slow or halt the progression of these conditions, CXL may prevent further loss of best-spectacle corrected visual acuity (BSCVA) if used at the earliest signs of progressing keratoconus or post-LASIK ectasia.7,8 Missing an early diagnosis for these conditions could lead to a malpractice suit, given this new opportunity to slow or halt progression of the disease in a milder state.
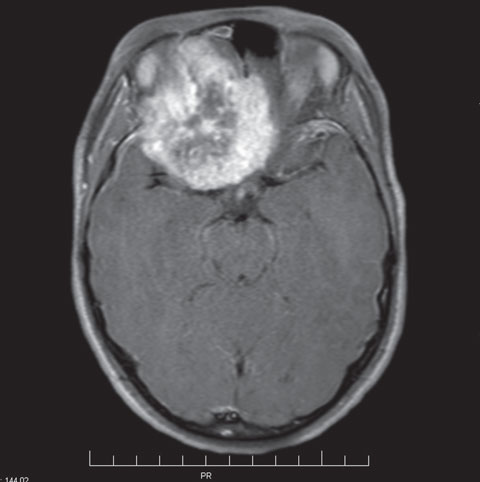
Case 1: Reduced Vision Due to Brain Tumor | ||
The next year, he returned with broken glasses and a complaint of headaches. BSCVA was 20/200 OD and 20/20 OS. Pupils were recorded as equal, round and reactive to light and accommodation with no afferent pupillary defect. Confrontation fields were full and non-contact tonometry as 9mm Hg OD, 13mm Hg OS. Biomicroscopy was unremarkable, and undilated funduscopy was recorded with cup-to-disc ratios of 0.2 in each eye and normal posterior segments. The optometrist diagnosed possible amblyopia in the right eye and accommodative spasm. The following year, he returned but was not examined because the public health insurance would not cover the costs of the exam. A year later, the patient was examined by a pediatric neuro-ophthalmologist on referral by his primary care physician. An emergently ordered MRI showed a mass larger than a golf ball pressing against his right optic nerve. Multiple surgeries successfully removed the meningioma, but he ended up with no light perception in the right eye. The patient’s family filed a malpractice claim against the optometrist. During discovery, the defendant OD produced a referral note indicating that he had referred the boy to ophthalmology. The patient’s mother denied receiving a referral or receiving any communication about the urgency of identifying the cause of her son’s reduced vision. As the plaintiff’s expert witness, I opined that the optometrist failed to meet the standard of care due to an inadequate attempt to identify the cause of BSCVA dropping from 20/20 to 20/200 over a year. Ambylopia was not a reasonable diagnosis since the patient previously had 20/20 acuity in that eye with no anisometropia, strabismus or media opacity. Accommodative spasm also was not a reasonable diagnosis given the unilateral nature of reduced vision and poor BSCVA. Regardless of whether or not an appropriate referral was made to an ophthalmologist, the OD should have performed a dilated eye examination, automated visual fields, rechecked for a relative afferent pupillary defect and ensured he was seen by an ophthalmologist while conveying urgency to the parent. Earlier detection of the meningioma would likely have averted this patient’s catastrophic vision loss. This case settled for an undisclosed amount. |
There are several precautionary steps you can take to protect yourself from malpractice suits.
(1) Assume a likeable chairside manner. Some of us are blessed with this natural demeanor, but some are not. Although personality is largely immutable, you can work on traits and habits conducive to communicating warmth and compassion. In one study, resident physicians received empathy training modules, after which patients rated a significantly improved physician empathy.9 Patient surveys can offer valuable feedback in guiding you. A strong patient-doctor relationship is protective against malpractice claims. “Patients don’t like suing doctors that they like,” says Michael G. Harris, OD, JD, MS, clinical professor emeritus at the UC Berkeley School of Optometry and attorney at law.
(2) Carefully document and ensure good communication. If your exam records don’t document a diagnostic test, it’s assumed that it was not done. Your duty as a practitioner is to maintain an accurate and complete record, which can be challenging in the age of electronic health records (EHR). It’s also important to communicate your diagnosis clearly to the patient, especially if there is potential for vision loss. For inconsequential findings, such as a benign iris nevus, it’s a judgment call whether to mention it. “It is important to document your advice and instructions regarding follow-up care,” Dr. Harris adds.
(3) Determine the cause of any reduced BSCVA, abnormal findings or worsening symptoms. For example, if you have a patient who presents with intraocular pressure (IOP) of 28mm Hg OD and 17mm Hg OS, then has IOP of 15mm Hg OU the next day, it is not acceptable to let the patient return in 12 months—you need to find out why there was an abnormal IOP to avoid missing a crucial diagnosis. In many instances, retinal imaging alone is not sufficient to rule out retinal pathology, as dilated examination is the standard.10
(4) Routinely administer automated screening visual fields, tonometry and dilated eye examination. A disproportionate number of conditions practitioners allegedly failed to diagnose could have been detected with these three measures. Liberal use of pupil dilation is perhaps the single most important action an optometrist can do to reduce the likelihood of a misdiagnosis that results in a malpractice claim.6
(5) Err on the side of over-referring. If your patient’s diagnosis is out of your expertise or comfort level, document the reason for referral and the name of the practitioner (if known) or type of specialist, and explain the rationale for the referral to your patient. It’s always a good idea to provide the doctor a referral letter or a copy of your exam findings and diagnosis. Especially with high-risk conditions, such as a macula-on retinal detachment or paracentral microbial keratitis, make sure you or your staff confirms the appointment was made and document the appointment time in your records. According to Dr. Miller, “When there is no consultation report received after the patient is referred, it is always a good idea to follow up with the patient and the physician.”
(6) Administer informed consent and document when patients decline dilation when medically indicated. Dilation is crucial to confirm myriad diagnoses. If the patient recognizes the increased risk and makes an informed decision to decline dilation, thereby hindering your ability to provide a definitive diagnosis, this should be memorialized by the patient’s signature with a date. “In some cases, you may want to use a specific informed consent document and have it signed by the patient and witnessed,” says Dr. Harris. Of course, the patient must be legally able to give consent; in the event the patient is a minor or impaired, the parent or guardian should sign the form.
(7) Stay up-to-date. Clinicians should remain current with continuing education and certifications, as diagnostics evolve with new technology, clinical practice guidelines and court precedents. For example, the availability of anti-VEGF injections for treating wet age-related macular degeneration now opens up the possibility of increased malpractice exposure for ODs who fail to diagnose this in a timely fashion.11
(8) Have adequate professional liability insurance. Most practitioners should have at least a $2 million occurrence limit and a $4 million aggregate limit. A personal umbrella policy will not cover excess liability beyond your professional liability insurance. When you end or switch your professional liability insurance, it is wise to obtain or confirm the existence of “tail coverage,” which extends the time after you drop the policy when you can still report claims brought against you. “If you retire, make certain you are still covered for any actions that may arise out of the time you actually saw patients,” says Dr. Miller. “Beware of the statute of limitations, especially with respect to minors you saw during your practice years.”
 |
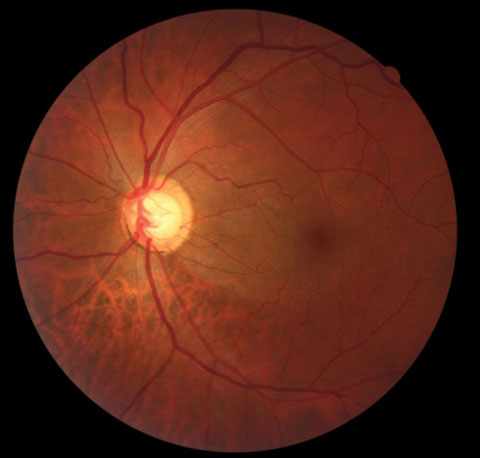
| Research suggests retinal detachment, as seen here, is a common condition underlying optometric malpractice claims. Click image to enlarge. |
If You Are Sued
The patient, their attorney, or your state board may notify you of a malpractice suit for failure to diagnose. In these situations, contact your professional liability insurance carrier without delay and provide the requested documentation. Never contact the patient or the patient’s attorney without first consulting your professional liability insurance to avoid jeopardizing your case. Any information you share can be used against you. Your professional liability insurance will assign you an attorney to guide your legal defense.“You may not agree with the advice given to you by the insurance company’s attorney, especially if you are advised to settle a case which you think has no merit,” says Dr. Harris. “You can hire your own private attorney, but this is usually extremely expensive and not worthwhile. It is usually best to heed the insurance company’s attorney’s advice even if you disagree with it.”
| Should You Apologize? |
| If a patient has a poor outcome, it can be tempting to apologize. However, it’s best to seek your legal counsel’s opinion first. Apologizing when you did nothing wrong may compromise your defense. In a survey of nearly 1,400 physicians who were sued, when asked, “Would saying ‘I’m sorry’ have helped?” 93% answered “no.”1 A better approach may be to express compassion for your patient’s situation. In the majority of instances, any communication after a claim is made between you and the patient should be through each party’s legal counsel. |
While you review your patient’s records, know that adding supplemental notes or making deletions to the records after learning about the suit is fraught with danger. Such changes to the records are discoverable and can look suspicious. “Tampering with records can lead to other serious legal action and sanctions from your state board,” says Dr. Harris.
However, if you do recall pertinent information, Dr. Miller says, “it’s best to add it as a separate informational sheet that is dated, signed and includes the reason for the addendum. This makes it clear that it is not part of the original patient record, but allows for your input.”
Expect a Marathon, Not a Sprint
Malpractice suits are time-consuming and disruptive to your schedule, as 78% last more than a year, and 39% last more than three years.12 Additionally, 28% of physicians sued spent more than 40 hours in preparation of their case and 30% of those going to trial spent 40 hours or more in court and trial-related meetings.12But most cases will settle. In an analysis of 518 optometric cases, 98% were the result of negotiated settlements and only 2% the result of court judgments.1
Case 2: Symptoms from Macular Edema Blamed on LASIK | ||
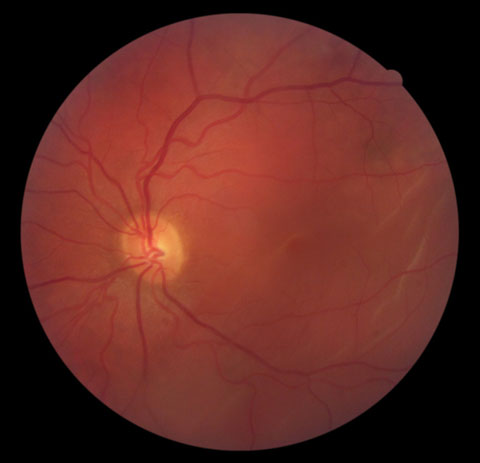
| A 35-year-old woman underwent uncomplicated, successful bilateral LASIK for moderate myopia. Her ocular history was significant for a retinal condition as a teenager, which she remembered as macular degeneration. However, the preoperative dilated eye examination failed to show any retinal pathology. At the one-month postoperative visit, unaided visual acuities were 20/20 in each eye, and biomicroscopy was unremarkable aside from meibomian gland secretions under the left flap. At the three-month postoperative visit, unaided visual acuities had not changed. Biomicroscopy was unremarkable except for epithelial ingrowth under the left flap edge periphery. At nine months postoperatively, the patient presented complaining of “split vision” in the left eye with symptomatic onset about one month prior. Unaided visual acuities were 20/20 in each eye. Amsler grid for the right eye was normal, but metamorphopsia was present in the left eye. The patient was referred to a retinal specialist.
The patient filed a complaint claiming damages in excess of $500,000 against the optometrist who provided her postoperative care, alleging negligence and failing to refer her for treatment of epithelial ingrowth. As the expert witness for the defendant optometrist, I opined that the optometrist met the standard in providing postoperative care for this patient. Most cases of epithelial ingrowth are clinically insignificant and non-progressive. In such cases, monitoring is usually sufficient and referral is not required. However, if epithelial ingrowth is progressive and forming nests near the visual axis, it is appropriate to refer the patient back to the refractive surgeon to lift the flap, remove the cells and prevent keratolysis. In this case, I found that the patient’s symptoms were attributable mostly, if not entirely, to macular edema and not epithelial ingrowth or other interface debris. As this case is pending, additional information may come forth. |
Closing Arguments
Unfortunately, good doctors sometimes get sued for malpractice. It’s not possible to eliminate all medicolegal risk, but these measures can minimize your exposure. Patients generally don’t expect perfection from their doctor. We are all human and make mistakes. Yet, our patients expect us to be competent and render reasonably prudent care, and rightfully so.Dr. Chou serves as an expert witness for litigation involving optometric standard of care. He is a partner at EyeLux Optometry in San Diego and writes on a diverse range of industry topics.
Disclaimer: The content in this article is for general information only and does not constitute legal or professional advice or an opinion of any kind.
| 1. Duszak RS, Duszak R. Malpractice payments by optometrists: An analysis of the national practitioner database over 18 years. Optometry. 2011:82:32-7. 2. Kirkner RM. How to manage your malpractice risk. 2009 January. Available at www.reviewofophthalmology.com/article/how-to-manage-your-malpractice-risks. Accessed Jan. 23, 2017. 3. Weber P. Youg ophthalmologists on trial. The Ophthalmic Risk Management Digest. 2015;25(4):1-7. Available at www.omic.com/wp-content/uploads/2015/12/Digest-v25-n4-2015.pdf. Accessed Jan. 23, 2017. 4. Sherman J. Top triggers for malpractice suits. Optometric Management. July 1, 2001. Available at www.optometricmanagement.com/issues/2001/july-2001/top-triggers-for-malpractice-suits. Accessed Jan. 23, 2017. 5. Meszaros L. Navigating optometric litigation. Optometry Times. September 1, 2012. Available at www.optometrytimes.modernmedicine.com/optometrytimes/news/modernmedicine/modern-medicine-feature-articles/navigating-optometric-litigation?. Accessed January 23, 2017. 6. Classé JG. How to be sued for malpractice. Rev Optom. 2004;151(10): 29-34. 7. Avedro. Avedro receives FDA approval for Photrexa Viscous, Photrexa and the KXL system for corneal cross-linking. 2016. Available at www.avedro.com/en-us/press-releases/avedro-receives-fda-approval. Accessed Feb. 10, 2017. 8. Avedro. Avedro receives additional indication for Photrexa Viscous, Photrexa and the KXL system for the treatment of corneal ectasia following refractive surgery. 2016. Available at www.avedro.com/en-us/press-releases/avedro-receives-additional-indication-for-photrexa-viscous-photrexa-and-the-kxl-system-for-the-treatment-of-corneal-ectasia-following-refractive-surgery. Accessed Feb. 10, 2017. 9. Riess H, Kelley JM, Bailey RW, et al. Empathy training for resident physicians: a randomized controlled trial of a neuroscience-informed curriculum. J Gen Intern Med. 2012;27:1280-6. 10. Chou B. Limitations of the Panoramic 200 Optomap. Optom Vis Sci. 2003:10:671-2. 11. Sherman J. Optometrists should prepare for potential rise in AMD lawsuits. Healio: Primary Care Optometry News. November 2013. 12. Kane L. Medscape malpractice report: Did they deserve to get sued? 2013. Available at www.medscape.com/features/slideshow/malpractice-report/public#1. Accessed January 23, 2017. |