 |
A 25-year-old woman presented for evaluation reporting daily, recurrent, predominantly left-sided headaches that had been worsening over the past two years. She indicated that the headaches interfered with her ability to work and were associated with blurry vision and eye pain. The patient denied any diplopia, motor or cognitive issues, but did report a “fluttering” sound that was more noticeable in her left ear. She also recalled that she had suffered transient visual “blackouts” since her teen years. According to her records, a previous optometrist had referred her for a neurological evaluation and magnetic resonance imaging (MRI) of the brain, but these scans were reportedly negative. Her medical history was positive for seasonal allergies and associated sinus congestion, but was otherwise unremarkable. The only medication that the patient admitted to using was an implanted birth control device.
Evaluation
The patient’s uncorrected visual acuity was 20/20 OD, OS and OU. Pupils were equal and reactive, without afferent defect. Ocular motilities were smooth and unrestricted. Visual fields by confrontation were full. Her blood pressure was 118/90 and she was 5’ 3” and weighed 200 lbs. Intraocular pressures (IOP) measured 18mm Hg OD and 20mm Hg OS. Dilated funduscopy revealed mildly elevated and hyperemic optic nerve heads in both eyes, with indistinct margins and a cup-to-disc ratio of approximately 0.2/0.2.
Prior records were obtained and the fundus photographs taken 21 months before were consistent with our funduscopic examination (Figure 1). B-scan ultrasonography had also been performed at the prior visit, which showed no evidence of buried optic nerve head drusen. While the patient had been referred for both MRI and neurologic consultation by the former optometrist, she admitted that she never followed up after learning that the MRI was “normal.” Given the overall presentation, we advised the patient that a neurologic assessment was imperative, and referred her for the appropriate clinical evaluation and testing.
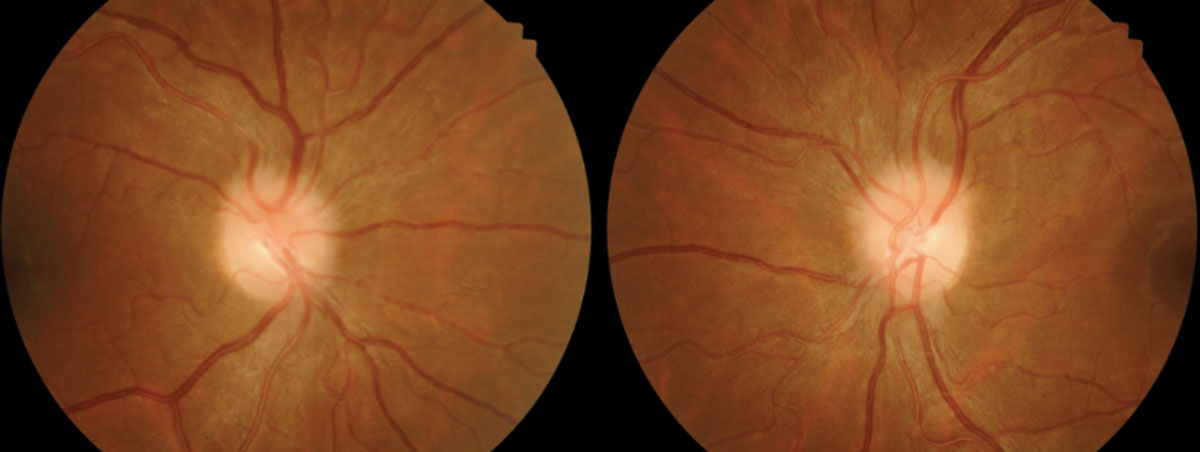 |
| Fig. 1. Fundus photos from January 2016. Note the blurred disc margins. Click images to enlarge. |
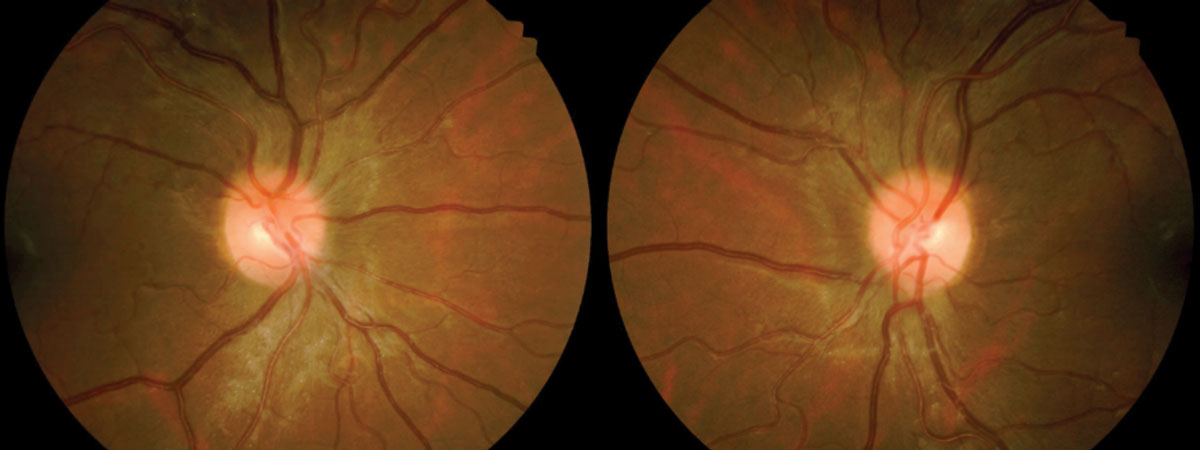 |
| Fig. 2. Fundus images from February 2018. Note disc edema resolution. Click images to enlarge. |
Diagnosis
This patient was diagnosed with pseudotumor cerebri (PTC), sometimes referred to as idiopathic intracranial hypertension (IIH). It is considered a diagnosis of exclusion. It is often suspected in cases of optic disc edema associated with headache, transient visual obscuration, intermittent horizontal diplopia, tinnitus, nausea and vomiting in young, overweight females.1-6 However, to rule out other conditions that may present similarly (e.g., brain tumors, hydrocephalus and cerebrovascular malformations), this diagnosis requires careful neurologic assessment and radiographic evaluation.1-5
While the pathophysiology of PTC is not completely understood, some things about the condition are well known. True IIH (which is a specific subset of PTC) occurs most frequently in obese young women between the ages of 15 and 45.1-6 Overall, the condition is rare, with a worldwide incidence of just 1 to 3 per 100,000, but the number of affected women outnumber men by a ratio of up to 9:1.6 Moreover, the incidence of IIH is approximately 15 times greater in women who are at least 10% above their ideal body weight.6 Certain medications—such as tetracycline derivatives, cyclosporine, lithium, naladixic acid, nitrofurantoin, oral contraceptives, levonorgestrel, danaxol and tamoxifen—may precipitate PTC in susceptible individuals.2,5 One study shows patients with mild visual loss could be controlled with a combination of acetazolamide and a low sodium diet.7 Additionally, patients taking acetazolamide had significantly improved papilledema, quality-of-life measures and lower cerebrospinal fluid pressure.7
Diagnostic Criteria for PTC (Modified Dandy Criteria)4
|
Background
The topic of birth control and PTC has drawn considerable interest over the years. Reports of neurological sequelae in association with oral contraceptives date back to the 1960’s.8-11 More recently, long-term implantable contraceptives such as Norplant (levonorgestrel, Wyeth-Ayerst) Jadelle (levonorgestrel, Bayer), Implanon and Nexplanon (etonogestrel, Merck) have likewise been implicated in some cases of PTC.12,13 Norplant was discontinued in the United States in 2002, and Jadelle (also known as Norplant II) was never marketed, but both of these products are available in other regions throughout the world. Implanon was discontinued in the United States in 2010 and replaced by Nexplanon, a newer version of the implant designed to reduce the risk of insertion errors. Although no direct cause-and-effect relationship has been established between any of these medications and PTC, the levonorgestrel-containing products do carry a specific warning regarding IIH. Implanon and Nexplanon appear to be safer in this regard, but cases of PTC have still been reported; the authors have suggested that the mechanism of PTC in association with etonogestrel-containing products may be rapid weight gain rather than direct hormonal influence.13
Treatment
Given that our patient displayed numerous features commonly associated with PTC, we felt confident that neurologic consultation was appropriate. After obtaining additional MRI studies of the brain and performing a lumbar puncture to assess the intracranial pressure (which ultimately was elevated), the patient was diagnosed with PTC and initiated on a therapy of oral acetazolamide (250mg QID). Due to a possible causal effect, she was also referred by the neurologist to her primary care provider for explantation of her subdermal birth control device. The patient returned to our clinic about five months after we had last seen her, reporting improvement in symptoms. Examination showed markedly improved disc edema, both on funduscopic evaluation and optical coherence tomography (Figure 2). Visual field testing showed no discernible pattern of loss.
While PTC is uncommon, it remains of particular importance to optometrists because visual disturbances and headache are typically the primary symptoms, and papilledema is the most readily observable sign. While one cannot make this diagnosis without complete and thorough testing, the clinical scenario is often strikingly prototypical. We urge all readers to avoid jumping to conclusions and making this diagnosis in “a typical patient profile” without obtaining the necessary evaluations detailed here. Recognizing the crucial elements of the medical history and facilitating prompt and appropriate care is the key to successfully managing these patients.
1. Wall M. Update on Idiopathic Intracranial Hypertension. Neurol Clin. 2017;35(1):45-57. 2. Biousse V, Bruce BB, Newman NJ. Update on the pathophysiology and management of idiopathic intracranial hypertension. J Neurol Neurosurg Psychiatry. 2012;83(5):488-94. 3. Contreras-Martin Y, Bueno-Perdomo JH. Idiopathic intracranial hypertension: descriptive analysis in our setting. Neurologia. 2015;30(2):106-10. 4. Smith JL. Whence pseudotumor cerebri? J Clin Neuroophthalmol. 1985;5(1):55-6. 5. Wall M. Idiopathic intracranial hypertension. Neurol Clin. 2010;28(3):593-617. 6. Durcan FJ, Corbett JJ, Wall M. The incidence of pseudotumor cerebri: population studies in Iowa and Louisiana. Arch Neurol. 1988;45(8):875-7. 7. Wall M, McDermott MP, Kieburtz KD, et al. NORDIC Idiopathic Intracranial Hypertension Study Group Writing Committee. Effect of acetazolamide on visual function in patients with idiopathic intracranial hypertension and mild visual loss: the idiopathic intracranial hypertension treatment trial. JAMA. 2014;311(16):1641-51. 8. Salmon ML, Winkleman JZ, Gay AJ. Neuro-ophthalmic sequelae in users of oral contraceptives. JAMA. 1968;206(1):85-91. 9. Walsh FB, Clark DB, Thompson RS, et al. Oral contraceptives and neuroophthalmologic interest. Arch Ophthalmol. 1965;74(5):628-40. 10. Soysa ND. The oral contraceptive pill and benign intracranial hypertension. N Z Med J. 1985;98(784):656. 11. Finsterer J, Kues EW, Brunner S. Pseudotumour cerebri in a young obese woman on oral contraceptives. Eur J Contracept Reprod Health Care. 2006;11(3):237-40. 12. Alder JB, Fraunfelder FT, Edwards R. Levonorgestrel implants and intracranial hypertension. N Engl J Med. 1995;332(25):1720-1. 13. Kassen N, Wells CL, Moodley A. Pseudotumor Cerebri and Implanon: Is Rapid Weight Gain the Trigger? Neuroophthalmology. 2015;39(6):281-4. |

