 |
Q:
A 25-year-old presents with bilateral red eyes. He has a past history of chlamydia. Could the two be related?
A:
“When a patient presents with a red eye, you should keep sexually transmitted infections (STIs) in the back of your mind, but not necessarily at the top of your differential list,” Julie A. Tyler, OD, associate professor at the Southern California College of Optometry at Marshall B. Ketchum University, says. It is important to thoroughly review the patient’s systemic and social history along with the ocular complaints.
 |
|
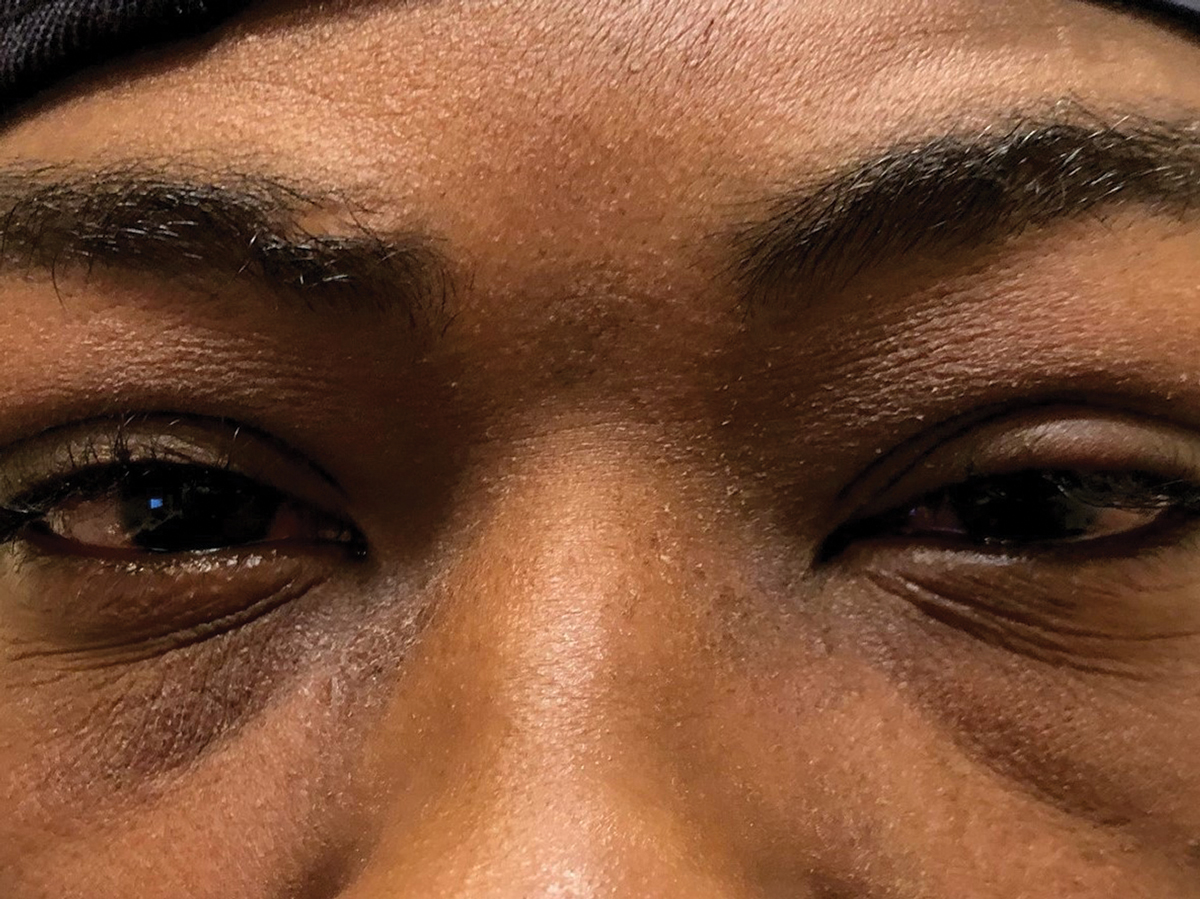
Fig. 1. This 25-year-old patient presented with swollen lids and preauricular nodes. Click image to enlarge. |
The hallmark of a gonorrhea-related conjunctivitis is hyperacute discharge and is less likely to be missed. Chlamydia, on the other hand, is often overlooked by presenting with characteristics of both viral and bacterial infections. “Ask the patient if they or their partner(s) have experienced any rashes, lesions or painful urination,” she says. “Also, check for a follicular response of the palpebral conjunctiva.”
You may find it awkward to ask patients about STIs, but do it anyway. If they feel uncomfortable discussing their sexual history or getting tested, seek out their primary care physician. If they are looking for anonymity, think about suggesting a community medical clinic.
Whatever you suspect, always rule out a viral etiology by making it standard protocol to check for preauricular nodes (PAN) on all red eye patients. If nodes are swollen and the patient has a red eye, suspect epidemic keratoconjunctivitis (EKC). Swollen lids can be a hallmark as well (Figure 1).
Check It Early
With EKC, early identification is important to try and prevent spread to the other eye or to other people. “Some practitioners recommend diluted Betadine (povidone-iodine 5%) lavage,” Dr. Tyler says. This can be quite irritating to the ocular surface and can create additional issues, so this treatment is not universally embraced.
Another option Dr. Tyler recommends is off-label use of Zirgan (ganciclovir 0.15%, Bausch + Lomb) ophthalmic gel to decrease the chance of developing corneal infiltrates.
Other supportive measures include topical steroids, especially if infiltrates or pseudomembranes are present, and lots of lubricants, along with cold compresses and isolation to prevent spread.
What’s the Difference?
Chlamydia is the most common STI in the United States and is the result of an intracellular obligate organism that presents with properties of bacteria and virus in the eye. Chlamydia trachomatis is the most common pathogen, but others include Chlamydia psittaci and Chlamydia pneumonia.
According to Dr. Tyler, there are many ways to assess for chlamydial infection that are more sensitive and specific than in the past—such as urine testing and even at-home tests. The preferred testing to identify chlamydia is nucleic acid amplification testing (NAAT), which is recommended because of its greater sensitivity. Ideally, direct tissue specimens, which may include conjunctival sampling, are preferred over urinalysis.
A variety of enzyme-linked immunosorbent assay tests are also available for chlamydial detection, such as MicroTrak (Syva Company), Chlamydiazyme (Abbott Laboratories), EIA (Pharmacia) and SureCell Chlamydia Test Kit (Kodak).
“Treatment of choice is a 1g, one-time dose of azithromycin, but doxycycline 100mg BID for one day and then 100mg daily for 21 days is also an alternative,” Dr. Tyler said. To be safe, the patient was referred to a local clinic where he tested negative for chlamydia. EKC, the original working diagnosis, was confirmed, and the patient was treated accordingly.
| 1. Elkhouly A, Kaplan A C Noteworthy neurological manifestations associated With COVID-19 infection. Cureus 12(7): e8992. |

