 |
Q:
What is the real significance of endothelial blebs and how do I best view them in my scleral lens wearers?
A:
These are edematous cells “visible under high magnification slit lamp examination or, preferably, through specular microscopy,” says Langis Michaud, OD, MSc, chief of the contact lens department at the University of Montreal. “Cell-warped apical surfaces cause the loss of the light ray reflection, making the cell appear black. Consequently, it is possible to observe a transient disappearance of endothelial cells from the mosaic observed in specular reflection.”
Blebs occur shortly after a contact lens is fit, creating hypoxic stress, and they disappear once the lens is removed or the cornea adapts to the lens, says Dr. Michaud. “This is called the bleb response, and it has been reported after lens wear with oxygen impermeable polymethyl methacrylate, rigid gas permeable, hydrophilic and, most recently, scleral contact lenses.” In a recent study, researchers found higher central tear fluid thickness was associated with a greater number of blebs during scleral lens wear.1
“This represents proof that hypoxic stress occurs during scleral wear,” says Dr. Michaud. He also believes it validates theoretical models that predict hypoxia will be generated if a scleral lens is too thick (>250µm) and its fit has more than 200µm of central clearance.2
Despite this, induced edema remains clinically invisible because it does not exceed 3% during lens wear and affects only the central cornea (except in compromised corneas).
“Some authors consider this induced edema as benign or not clinically significant, and others compare it to physiological edema,” says Dr. Michaud. However, he considers this misleading because the cornea recovers from physiological edema within an hour post-awakening. In sclerals, 1% to 3% of edema remains for the entire wearing period, and because the lenses are inserted shortly after awakening, the cornea can never recover, Dr. Michaud says. “Nobody can tell, at this point, how a cornea will react to this chronic hypoxic stress long-term, but corneal edema moved the entire soft lens industry to research and find highly permeable materials, so it should do the same for scleral lenses, where optimal designs are needed.”
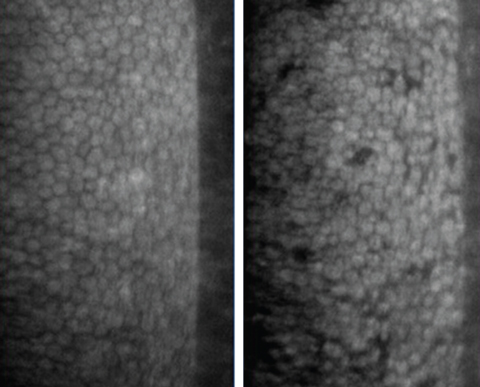 |
| At right, the black spots are endothelial blebs. At left, the same cornea without blebs prior to lens wear. Photos: Langis Michaud, OD, MSc |
Solving the Problem
To minimize hypoxic stress, Dr. Michaud offers these guidelines: keep the lens as thin as possible and align it in every quadrant to alleviate flexure; keep central corneal clearance under 200µm after lens stabilization; select the highest Dk material; and monitor clinical signs.
When monitoring, practitioners should perform pre- and post-fit global corneal pachymetry to establish comparative maps and track swelling; check for microcysts and bullae or loss of transparency, especially if the endothelial layer is compromised or if the cell count is reduced; note any increased symptomatology of glare and haloes, especially at lens removal; and observe the endothelial layer under high magnification slit lamp 15 to 20 minutes after lens wear to track the presence of endothelial blebs.
“Whenever possible, consider redesigning scleral lenses to alleviate hypoxic stress,” says Dr. Michaud. “In some cases, however, such as when the endothelial cell count is less than 1000 cells/mm2, you may need to consider options other than scleral lenses, especially in challenged graft patients.”
1. Giasson CJ, Morency J, Melillo M, Michaud L. Oxygen tension beneath scleral lenses of different clearances. Optom Vis Sci. 2017;94:466-75. |

