AMD May be Underdiagnosed
New data suggests optometrists need to take a closer look at fundus images to catch the disease early.
By Rebecca Hepp, Managing Editor
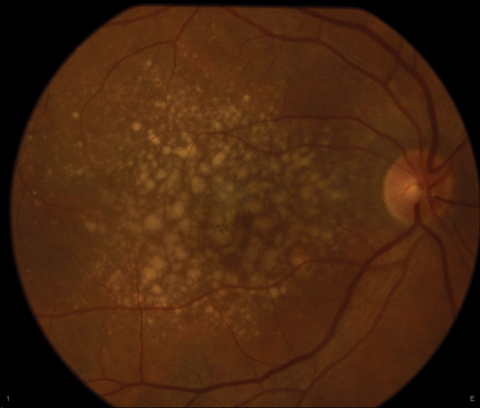 |
| More patients may have characteristics of early AMD than previously thought. Photo: Jay M. Haynie, OD |
After collating data from ophthalmology and optometry practices in Birmingham, Ala., researchers found that roughly 25% of 1,288 eyes deemed normal based on the most recent dilated fundus exam had characteristics of age-related macular degeneration (AMD) on fundus photography, as identified by trained raters.
The study included 644 patients 60 or older with normal macular health and no AMD diagnosis in the medical record. While 75.2% had no AMD, which correlated with their medical record, 24.8% had AMD, the researchers said. Of those undiagnosed with AMD, 10.0% had hyperpigmentation, 13.4% had hypopigmentation, 77.8% had small drusen, 78.1% had intermediate drusen and 30.0% had large drusen. The data further shows the lack of AMD diagnoses was associated with older age, male sex and lower education. The prevalence of undiagnosed AMD was no different between ophthalmologists and optometrists.
“This data is very unsettling; undiagnosed AMD in the setting of having had a dilated eye exam is unacceptable,” says Sara Weidmayer, OD, of Ann Arbor, Mich. “Primary eye care providers arguably should be able to detect clinical features of AMD based solely on a comprehensive dilated eye exam. While the authors suggest several possible causes for this lack of diagnosis, one that individual providers can strive to improve is their level of attention. Efficiency of care should not outweigh quality of care.”
The undiagnosed eyes with AMD with large drusen would have been treatable, the researchers conclude, highlighting the long-term impact of early diagnosis. They hope these findings help clinicians improve early detection and treatment.
“This data should be a call to action for primary eye care providers to heighten our awareness as we carefully examine to detect disease in our patients,” Dr. Weidmayer says.
| Neely DC, Bray KJ, Huisingh CE, et al. Prevalence of undiagnosed age-related macular degeneration in primary eye care. JAMA Ophthalmol. 2017;135(6):570-5. |
Visual Fields Vary with Cognitive Decline
Glaucoma patients and suspects with cognitive decline also have increased variable visual fields (VFs) over time, according to a new study. Researchers suggest screening for and monitoring cognitive dysfunction may be important when practitioners assess their glaucoma patients’ VFs.
To determine if, and to what extent, patients’ VFs vary, researchers monitored 115 patients for a mean period of 2.5 years with standard automated perimetry (SAP) and longitudinal assessment of cognitive ability using the Montreal Cognitive Assessment (MoCA).
They observed a statistically significant association between cognitive decline and VF variability over time. A five-point decline in the MoCA score was associated with an increase in VF variability. After adjusting for baseline MoCA score, SAP mean deviation, age, sex, race/ethnicity, educational level, income and number of SAP tests, each five-point decline in MoCA score was associated with an even greater increase in VF variability.
Mohammad Rafieetary, OD, of Charles Retina Institute in Germantown, Tenn., says practitioners should consider all the possible reasons behind test results.
“When clinicians rely on testing to diagnose and manage conditions, we should consider all the possible impelling factors affecting the results of the specific test,” says Dr. Rafieetary. This is even more important in those tests that rely on patient’s subjective input, he explains. “Visual fields as a psychometric test relies heavily on patients’ understanding of the test, cooperation during testing and reliability in responding to the stimuli. Therefore, it is justifiable to conclude that patients’ cognition will play a role in visual field results.”
Neurodegenerative conditions may directly affect the VF as well, according to Dr. Rafieetary. “Vision and visual perception are neuroprocessing functions; therefore, it is conceivable to assume that neurodegenerative conditions may directly affect visual field,” he says.
Lastly, practitioners should consider the possibility of glaucoma itself being a neurodegenerative disorder, Dr. Rafieetary says.
| Diniz-Filho A, Delano-Wood L, Daga FB, et al. Association between neurocognitive decline and visual field variability in glaucoma. JAMA Ophthalmol. May 2017. [Epub ahead of print]. |
Contact Lenses for Kids
Your pediatric patients may be better candidates for contact lenses than you thought, according to a new research review. After looking at large-scale epidemiological studies, hospital-based case series, long- and short-term prospective studies and multicenter retrospective studies, Mark A. Bullimore, MCOptom, PhD, from the University of Houston College of Optometry found the incidence of corneal infiltrates in children who wear contact lenses is no higher than it is in adults. Dr. Bullimore also suggests the incidence may be even lower in children ages eight to 11, according to the data.1  |
| Kids as young as eight may be able to safely switch from glasses to contact lenses, according to new data. Photo: Kathleen Elliott, OD |
This research suggests “children are capable of soft, gas permeable and orthokeratology contact lens wear,” says Jeffrey J. Walline, OD, PhD, associate dean for Research at The Ohio State University. “Although no single study provides a comprehensive examination of contact lens safety in children, a review of the literature provides consistent evidence of the safety of pediatric contact lens wear.”
Based on three large prospective studies representing between 159 and 723 years of soft contact lens wear in eight- to 14-year-olds, the incidence of corneal infiltrative events is up to 136 per 10,000 years, Dr. Bullimore found. A large retrospective study found a rate of 97 per 10,000 years in eight- to 12-year-olds and 335 per 10,000 years in 13- to 17-year-olds.1
In comparison, Dr. Bullimore notes the incidence of symptomatic corneal infiltrative events in adults in the last decade was 432 per 10,000 patient years of mostly daily wear and 316 per 10,000 patient years for daily silicone hydrogel lens wear with monthly replacement.1
None of the prospective studies that included safety data report any cases of microbial keratitis. While one retrospective study found no cases of microbial keratitis in the eight- to 12-year-old participants, it found an incidence of 15 per 10,000 patient years in 13- to 17-year-olds. This rate is no higher than the incidence of microbial keratitis in adults wearing soft contact lenses on an overnight basis, according to Dr. Bullimore.1
Given the data, he concludes the incidence of corneal infiltrative events in children fit in contact lenses does not exceed the incidence in adults, and may even be significantly lower in children ages eight to 11. This lower rate found in eight- to 11-year-olds may be a result of patient behavior rather than biological factors, and may also be influenced by greater parental supervision, Dr. Bullimore said in the study.1
“Some of the improved safety of contact lens wear in children may be due to a large portion being fitted with daily disposable contact lenses,” adds Dr. Walline.
These findings could have a significant impact on special populations as well, Dr. Walline says. Take myopia control, for example.
Research suggests contact lenses can slow myopia progression from 25% to 72% compared with spectacles and come with a lower risk side effects compared with atropine use.2-8 Yet some practitioners may shy away from the modality for fear of increased adverse events in pediatric patients.
“Hopefully clinicians will begin to consider young myopic children as patients who are capable of independent contact lens care,” says Dr. Walline. “Clinicians may be more comfortable using contact lens myopia control methods, knowing that children can safely wear contact lenses.”
| 1. Bullimore MA. The safety of soft contact lenses in children. Optom Vis Sci. 2017;94(6):638-46. 2. Chia A, Lu Q, Tan D. Atropine for the treatment of childhood myopia: safety and efficacy of 0.5%, 0.1%, and 0.01% doses (Atropine for the Treatment of Myopia 2). Ophthalmology. 2012;119(2):347-54. 3. Sankaridurg P, Donovan L, Varnas, S, et al. Spectacle lenses designed to reduce progression of myopia: 12-month results. Optom Vis Sci. 2010;87(9):631-41. 4. Hasebe S, Jun J, Varnas SR. Myopia control with positively aspherized progressive addition lenses: a 2-year, multicenter, randomized, controlled trial. Invest Ophthalmol Vis Sci. 2014;55(11):7177-88. 5. Berntsen DA, Sinnott LT, Mutti DO, Zadnik K. A randomized trial using progressive addition lenses to evaluate theories of myopia progression in children with a high lag of accommodation. Invest Ophthalmol Vis Sci. 2012;53(2):640-9. 6. Anstice NS, Phillips JR. Effect of dual-focus soft contact lens wear on axial myopia progression in children. Ophthalmology. 2011;118(6):1152-61. 7. Sankaridurg P, Holden B, Smith E, et al. Decrease in rate of myopia progression with a contact lens designed to reduce relative peripheral hyperopia: one-year results. Invest Ophthalmol Vis Sci. 2011;52(13):9362-7. 8. Walline JJ, Greiner KL, McVey ME, Jones-Jordan LA. Multifocal contact lens myopia control. Optom Vis Sci. 2013; 90(11):1207-14. |
In the NewsTo better understand the relationship between retinal nerve fiber layer (RNFL) defects and disc hemorrhages (DHs), researchers screened 168,044 patients older than 20, and found that DHs located in the inferotemporal quadrant were associated with RNFL defects, even after adjusting for proximal location. After adjusting for quadrant location, they found DHs with the proximal end located at the cup margin were more likely to have accompanying RNFL defects compared with DHs located outside the disc. Yoo YC, Kim JM, Park HS et al. Specific location of disc hemorrhage is linked to nerve fiber layer defects. Optom Vis Sci. 2017;94(6):647-53. Using online surveys, investigators found that respondents experience dry eye symptoms more frequently in their work environment than at home. In addition, up to 70% said they experienced some inhibition of daily activity at work due to eye symptoms, and more than 5% experience symptoms most or all of the time. The researchers suggest these findings highlight the need for a multidisciplinary understanding of the negative impact of dry eye in work environments. van Tilborg MM, Murphy PJ, Evans KS. Impact of dry eye symptoms and daily activities in a modern office. Optom Vis Sci. 2017;94(6):688-93. After studying postmortem tissue of 30 patients, researchers discovered some brain tissue proteins continue to develop into midlife—specifically, the visual cortex matures until 36 years of age, plus or minus 4.5 years or so. The findings may impact how clinicians approach treatment options for patients with eye conditions such as amblyopia, the researchers conclude. Siu CR, Beshara SP, Jones DG, Murphy KM. Development of glutamatergic proteins in human visual cortex across the lifespan. J Neuroscience. 2017 May;2304-16. |

