In the Pipeline: Line-field OCT
This new modality may soon provide clinicians aberration-free retinal images at the cellular level.
By Rebecca Hepp, Managing Editor
A newly developed optical coherence tomography (OCT) technique, line-field (LF) OCT, may simplify how clinicians image ocular cellular processes, according to new research.1
The new technique uses linear illumination with rapid frame rates to allow digital correct of aberrations over the entire 3D volume of the retina, according to lead author Laurin Ginner, a PhD student studying under Rainer Leitgeb, PhD.2 The result is in vivo, aberration-free retinal images at the cellular level without expensive hardware adaptive optics (AO).1,2 While researchers already know combining AO with OCT can provide high isotropic resolution in 3D, “complexities of adaptive optics together with its costs make the commercialization of such technology difficult,” the study says.1
“Line field-OCT holds substantial promise in the diagnosis and management of retinal disease,” says Carolyn Majcher, OD, assistant clinical professor at the Rosenberg School of Optometry. “The cellular resolution provided by line-field OCT is far superior to conventional OCT such that even individual photoreceptors, capillaries and nerve fibers can be distinguished and evaluated.2 Visualizing fine cellular details permits imaging of cellular physiologic and metabolic processes such as photoreceptor disc shedding and axonal transport.”1,3
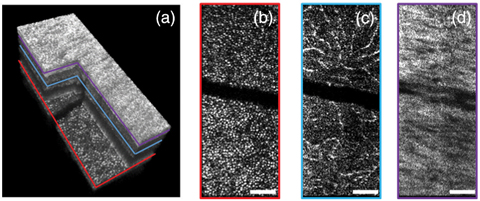 |
| This 3D volume of the retina is corrected for defocus and higher order of phase error (a). The photoreceptor layer is red (b), the outer plexiform layer is blue (c) and the nerve fiber layer is violet (d). The white scale bar denotes 100μm.1 Click photo to enlarge. Photo: Laurin Ginner, PhD |
The researchers are also able to refocus, realign and digitally process the image data to help provide the best results for proper diagnosis and treatment management.1
“This sort of ‘functional OCT imaging’ of the retina will aid clinicians in earlier detection of retinal and optic nerve diseases,” says Dr. Majcher.1 “Instead of waiting for cells to die off so that conventional thinning of the retina and nerve fiber layer can be detected, this technology will likely have the ability to detect pre-death cellular dysfunction. Prompt disease diagnosis and intervention before irreversible cell death occurs will result in greater visual preservation.”
The researchers further applied the correction technique to OCT-angiography and found it improved vessel definition blurred by motion artifacts and defocus.1
“This will prove useful in the diagnosis of retinal vascular diseases and neovascular disorders such as diabetic retinopathy, retinal vein occlusion, age-related macular degeneration, and many more,” says Dr. Majcher.
“The eye is the ‘window’ into the brain. Our hope is that the higher resolution will help to improve diagnostic accuracy in general,” said Dr. Leitgeb in a press release.2
1. Ginner L, Kumar A, Fechtig D, et al. Noniterative digital aberration correction for cellular resolution retinal optical coherence tomography in vivo. Optica. 2017;4(8):924-31. |
Should Patients Laser Away Floaters?
Patients who experience reduced visual quality due to floaters may have a treatment option, YAG vitreolysis,
according to new research.1
“It is an interesting and exciting area to think about because we all have numerous patients that have floaters,” says Nate Lighthizer, OD, associate professor and chief of Specialty Care Clinics at the Oklahoma College of Optometry. “We see these patients on a day-in-and-day-out basis and often it’s been frustrating because we historically haven’t been able to give them many great treatment options.”
 |
| YAG vitreolysis may be an effective treatment option for a Weiss ring, but some worry about adverse effects. Photo: Joseph W. Sowka, OD, and Alan G. Kabat, OD |
Researchers randomly assigned 52 patients to either YAG laser vitreolysis or a sham laser treatment. Six months post-procedure, 54% of the YAG group reported an improvement in visual disturbances compared with only 9% of controls. In addition, 53% of the YAG group reported significant or even complete resolution of symptoms.1
The researchers also found the YAG group reported improved general vision, peripheral vision, role difficulties and dependency compared with pre-procedure.1
“This study is one more step to provide more evidence that it’s a safe, effective procedure, and patients show reduction in their symptoms, which is ultimately what we want for these symptomatic and often frustrated patients,” says Dr. Lighthizer. “It is nice to possibly have a treatment option in between observation and vitrectomy surgery, and one that is better than doing nothing and much less invasive than the higher risk surgical option.”
One reason for such positive study results is the careful patient selection process, said Jennifer Lim, MD, in a commentary.2 The researchers carefully screened for patients with symptomatic Weiss rings of at least six month’s duration and at least 3mm distant from the retina and 5mm from the posterior lens capsule.2 In addition, the procedure used energies just high enough for photodisruption of the Weiss ring. Together, these measures mitigated complications, Dr. Lim said.2
While promising, the results don’t necessarily confirm YAG vitreolysis is safe.2 Dr. Lim recommends opacities close to the lens and underlying vital structures not be treated with the YAG laser—at least until more studies can confirm these initial results.1,2
“The clinical data and scientific studies are telling us that we need to pick our patients appropriately,” adds Dr. Lighthizer. “Not all types of floaters will do equally well with this procedure, either. So we still have a lot to learn clinically about the procedure, but it is very exciting to finally have a treatment to offer our patients other than high-risk, invasive surgery.”
1. Shah CP, Heier JS. YAG Laser vitreolysis vs sham YAG vitreolysis for symptomatic vitreous floaters. JAMA Ophthalmology. July 20, 2017. [Epub]. |
Eye Docs Most Likely to Prescribe Branded Meds
Eye care practitioners prescribe more brand medications by volume than any other provider group, according to a recent analysis. In total, researchers found $2.4 billion in annual Medicare Part D prescription costs by optometrists and ophthalmologists in 2013, and the prescribers turned to branded medications 79% of the time.1 Glaucoma medications made up half of the ophthalmic drugs prescribed, at a cost of $1.2 billion, with dry eye medications coming in second, accounting for $371 million.1,2 These two categories, in addition to ocular inflammation and infection medications, made up 96% of drugs prescribed.1
The researchers conclude a switch to generics could reduce costs by $882 million a year.1 However, allowing Medicare to negotiate prices is the only long-term solution to high costs, according to the study authors. “If the cost of generic medications increase, such as what occurred in 2014 when the price of generic prednisolone acetate and generic phenylephrine soared, changing providers’ prescription patterns would not help to reduce costs,” says senior author Maria Woodward, MD.1
In on the Fight
While policy change is one solution to lower costs, Alan Kabat, OD, professor at Southern College of Optometry, says another option is keeping the doctor in charge.
“Optometrists are already under immense pressure to prescribe generic medications from much of their patient base due to cost concerns, and also from most third-party insurers, both governmental and commercial,” says Dr. Kabat. Even when branded medications are covered, they are typically in a higher tier, he says, requiring greater copay for the beneficiary. “Alternatively, insurance companies may require a prior authorization for a branded medication, with the doctor affirming that the patient has tried and failed with alternative treatment options, generics or legacy drugs.”
If health care were merely a dollars-and-cents matter, this would be an easy decision, says Dr. Kabat. But it is far more complex. “Physicians are trained to provide the best treatment option in any scenario. The drug or procedure that offers, for example, the greatest efficacy, the easiest dosing regimen or the least potential for complications is often not the least expensive. In effect, the current approach forces practitioners to choose between what is best and what is cheapest.”
“Lawmakers must recognize that physicians are the ultimate authority for determining which treatment option is most appropriate for each patient.”
In the end, he says, negotiating for better drug pricing directly with companies as a means to lower Medicare costs would be much more palatable to all parties involved than mandating which medications a doctor can prescribe.
| 1. University of Michigan. A switch to generic eye drugs could save Medicare millions. www.uofmhealth.org/news/archive/201707/switch-generic-eye-drugs-could-save-medicare-millions. Accessed August 18, 2017. 2. Newman-Casey PA, Woodward MA, Niziol LM, et al. Brand medications and medicare part D. Ophthalmology. 2017 July. [Epub ahead of print]. |
In the newsMore than 85% of adolescent (ages 12 to 17) contact lens wearers have at least one habit that increases their chances of an eye infection, according to a recent CDC Morbidity and Mortality Weekly Report. The most common risky habits in this age group were not visiting an eye doctor annually and wearing contact lenses while sleeping, napping or swimming. Patients ages 18 and older also reported ignoring proper lens and lens case replacement schedules. A new study confirms the additive effect of waiting five minutes between drop instillation for dilation drops. Although clinicians recommend patients wait five minutes between instilling different drops, the only human study to explore concurrent drop instillation found a 10-minute wait did not increase the combined effect. The results of this new study show waiting five minutes yielded a 5.6% relative pupil surface gain when instilling one drop of 10% phenylephrine and one drop of 0.5% tropicamide. Denion E, Charlot F, Béraud G. A 5-minute interval between two dilating eye drops increases their effect. Optom Vis Sci. 2017;94(8):838–44. Contact lenses coated with the mucin MUC5AC extracted from the stomachs of pigs no longer cause tissue damage to porcine eyes, according to a new study. Researchers found the mucin absorbs into the contact lenses, creating a lubricating barrier between the contact lens and the cornea. They speculate lubricating drops or soaking contact lenses overnight in a mucin solution will create the protective effects. Winkeljann B, Boettcher K, Balzer BN, Lieleg O. Mucin coatings prevent tissue damage at the cornea-contact lens interface. Advanced Materials Interfaces. 2017;1700186. [Epub]. |

