Retina Changes May Foretell Brain Diseases
Eye exams can offer a window into the central nervous system, according to a new study.
By Bill Kekevian, Senior Editor
New research suggests retinal evidence of diseases of the central nervous system may present prior to changes to the brain, according to a report in Human Molecular Genetics. The study, which employed mouse models, posits that eye examinations could serve as a noninvasive screening tool for some brain diseases.
“This particular study found a correlation between retinal and neurologic disease using electroretinography and visual evoked potentials. Other studies have used OCT or fundus autofluorescence as a retinal screening tool for neurologic conditions,” says Denise Goodwin, OD, who teaches on neuro-ophthalmic disease at Pacific University. “Ultimately, the retina is an extension of neurologic tissue in the brain; therefore, the use of the retina to screen for these conditions makes sense. The same processes that cause damage in the cortex may contribute to death of the retinal nerve fiber layer.”
Using functional testing methods, such as electroretinography and visual evoked potentials, investigators from the University of Eastern Finland evaluated several disease types in mouse models, including Huntington’s disease, Alzheimer’s and neuronal ceroid lipofuscinosis (NCL). All three disease types showed functional impairments prior to anatomical changes. For instance, in the Huntington’s disease group, day and color vision changes were recorded while the mouse was presymptomatic, the report says. The Alzheimer’s group showed changes to their night vision, and the NCL group demonstrated impaired retinal ganglion cell function, similar to that seen in age-related macular degeneration.
According to Dr. Goodwin, a number of studies are showing a correlation between the retina and degenerative brain conditions.
Relying on these noninvasive measures may provide an opportunity for less expensive and quicker diagnostic methods, she adds.
“Because neuronal damage can occur well before symptoms of cognitive decline, early detection can have a critical impact in the lives of these patients, Dr. Goodwin says. “It is exciting to think that something as basic as a vision examination could allow for earlier detection and diagnosis of these disabling neurologic diseases.”
|
Leinonen H, Rossi M, Salo A, et al. Lack of P4H-TM in mice results in age-related retinal and renal alterations. Human Molecular Genetics. July 27, 2016. [Epub ahead of print]. Available at http://hmg.oxfordjournals.org/content/early/2016/08/17/hmg.ddw228. Accessed October 14, 2016. |
Is a Corneal Scar Treatment on the Horizon?
With severe corneal trauma, scar tissue and vision loss are often the unfortunate byproducts of the healing process. Current treatments, including topical steroids and surgical modalities such as keratoplasty and limbal stem cell and amnion transplantation, are subject to limitations such as increased risks for infection and transplant rejection.
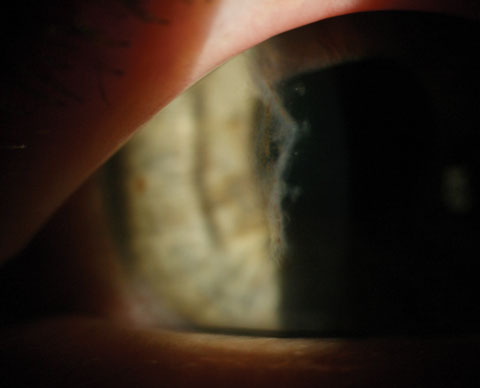 |
| Corneal scarring, as seen here, was nearly eliminated in MSC-treated animal corneas following injury. Photo: Elyse L. Chaglasian, OD, and Gregg Eric Russell, OD. |
In recent years, research suggests mesenchymal stem cells (MSC) have the ability to clear the corneal opacity that often forms following injury. Until recently, how the cells offer these benefits remained elusive.
A new study, published in Stem Cell Reports, sheds light on the mechanism of action that allows MSCs to clear cornea opacity following trauma. Researchers from Schepens Eye Research Institute of Massachusetts Eye and Ear found that hepatocyte growth factor (HGF), secreted by MSCs, is the key to their ability to encourage wound healing by interfering with the inflammatory response. Although the findings suggest the efficacy of HGF-based treatments to restore vision, according to a press release, the results were found use an animal model of corneal trauma, and more research is necessary to learn more about the process in the human eye.
HGF was applied topically to an injured animal model eye twice daily for up to seven days post-injury, and investigators used slit-lamp biomicroscopy to monitor corneal opacity. Corneas of HGF-treated mice showed reduced opacity at day five and, according to the researchers, near complete restoration of transparency on day seven, compared with the control group.
“Our results show that mesenchymal stem cells, in an inflamed environment, secrete high levels of HGF, which inhibit scar formation and restore corneal transparency,” senior author of the study, Sunil L. Chauhan, PhD, said in a press release. According to the researchers, MSC cells, when injected into the mice after being stimulated by immune system proteins to secrete HGF, migrated to the source of corneal injury via the bloodstream and induced corneal healing.
 |
But when the researchers suppress HGF gene expression using small interfering RNAs, Dr. Chauhan said in the press release, “the stem cells lose their capacity to inhibit scar formation.”
The researchers are hopeful for the implications the results have on future treatment options for severe corneal trauma. “That HGF alone can restore corneal transparency is highly significant and has tremendous translational implications for developing new treatment modalities,” Dr. Chauhan said.
|
Mittal SK, Omoto M, Amouzegar A, et al. Restoration of corneal transparency by mesenchymal stem cells. Stem Cell Reports. 2016. [Epub ahead of print]. |
Are Politics Seeping Into Your Exam Lane?
Are you confusing the exam lane with the voting booth? According to a recent study Yale researchers published in Proceedings of the National Academy of Sciences (PNAS), primary care doctors who fall on different sides of the aisle treat some of the more politicized health issues differently depending on their party affiliation. For instance, researchers say, Republicans rated “likely” the prospect of discussing the mental health consequences of abortion whereas Democrats expressed concern about the dangers of keeping a firearm in a home with a small child. Doctors on the left, according to the study, are also less concerned about marijuana use in otherwise healthy patients.
“We linked the records of over 20,000 primary care physicians in 29 states to a voter registration database, obtaining the physicians’ political party affiliations. We then surveyed a sample of Democratic and Republican primary care physicians,” the study reads.
Respondents were asked to consider nine patient vignettes and rate the seriousness of each issue as well as their likelihood of engaging with patients about them. The results show remarkable difference only on the three politicized issues (abortion, marijuana use and firearms). Doctors were relatively in agreement over the nonpoliticized issues presented, such as tobacco and alcohol use and obesity.
|
Hersh ED, Goldenberg MN. Democratic and Republican physicians provide different care on politicized health issues. Proceedings of the National Academy of Sciences. October 3, 2016. [Epub ahead of print]. Available at www.pnas.org/content/early/2016/09/28/1606609113. Accessed October 14, 2016. |
Cat-Scratch Fever on the Rise
Optometrists practicing in the Southern United States, or those who see patients between the ages of five and nine, might be more likely to encounter the ocular side effects of cat-scratch disease (CSD), a new study suggests. Investigators from the Centers for Disease Control and Prevention and Emory University reviewed insurance claim databases from 2005 to 2013, and discovered approximately 12,000 outpatients were given a CSD diagnosis, and 500 inpatients were hospitalized for the disease.
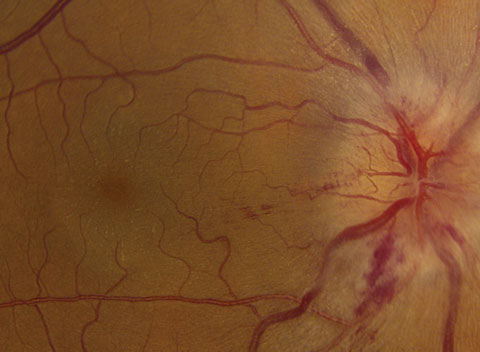 |
| If you look closely at the macula in this fundus photo, you’ll see exudate in a “macular star” pattern, a classic sign of cat-scratch disease. Photo: Mark T. Dunbar, OD. |
The study, recently published in Emerging Infectious Diseases, found the incidences of CSD were highest in southern states and among children between ages five and nine. Children younger than 14 accounted for 32.5% of all diagnoses and, although women and girls accounted for 62.0% of outpatient and 55.6% of inpatient diagnoses, inpatients were more likely than outpatients to be male and between the ages of 50 and 64.1
CSD is a zoonosis caused by Bartonella henselae, which is spread among cats by fleas; transmission to humans occurs via cat scratches, and possibly bites. While the predominant clinical feature of CSD is lymphadenopathy proximal to the site of the scratch or bite, some patients experience ocular effects such as neuroretinitis or parinaud oculoglandular syndrome. Other serious manifestations include osteomyelitis, encephalitis or endocarditis.2 While patients with typical signs of and history for CSD can be given a presumptive clinical diagnosis, diagnostic tests such as serology, PCR and culture can be useful for confirming the diagnosis when atypical.
Although the number of American households with cats has increased in recent decades, suggesting practitioners might see more of this diagnosis, the study found the annual incidence of outpatient CSD diagnoses steadily declined from 2005 to 2013. Still, optometrists should be aware of the ocular side effects of CSD and be prepared to treat these patients, and children in particular.3
|
1. Nelson CA, Saha S, Mead PS. Cat scratch disease in the United States, 2005–2013. Emerg Infect Dis. 2016 Oct;22(10). [Epub ahead of print]. 2. Florin TA, Zaoutis TE, Zaoutis LB. Beyond cat scratch disease: widening spectrum of Bartonella henselae infection. Pediatrics. 2008;121:e1413–25. 3. American Pet Product Manufacturers Association. New survey reveals pet ownership at all-time high. http://media.americanpetproducts.org/press.php?include=144262. Accessed October 19, 2016. |
In the news
Researchers have uncovered a unifying pathway involved in the damage to rods and cones, possibly leading to treatments for blinding diseases such as retinitis pigmentosa and dry AMD. The study, published in Cell Reports, found that defects in a key molecule pathway, NAD, are involved in several diseases of the retina. When they treated damaged photoreceptor cells in mice with a precursor molecule that boosts levels of NAD, degeneration of the cells ceased and vision was restored.
|
Lin JB, Kubota S, Ban N, et al. NAMPT-mediated NAD biosynthesis is essential for vision in mice. Cell Reports. 2016;17(1):69-85. |
A new encapsulated cell therapy, known as NT-501 ECT, might be a new glaucoma treatment in the pipeline. Currently in phase II trials, NT-501 ECT is a capsule filled with genetically modified human cells that secrete ciliary neurotrophic factor (CNF). The capsule is implanted into the eye, providing a slow release of CNF to help the retinal ganglion cells resist damage and protect the optic nerve. The trial will follow participants for two years to track any vision changes.
|
Goldberg JL. Study of NT-501 encapsulated cell therapy for glaucoma neuroprotection and vision restoration. Phase II trial. Available at https://clinicaltrials.gov/ct2/show/NCT02862938. Accessed October 17, 2016. |
The visual cortex plays a key role in promoting the plasticity of innate, spontaneous eye movements, according to a new study. Researchers studied eye movements in mice and found silencing the visual cortex significantly reduced optokinetic reflex activity, suggesting it is involved in mediating the plasticity between the optokinetic and the vestibulo-ocular reflexes.
| Liu B, Huberman AD, Scanziani M. Cortico-fugal output from visual cortex promotes plasticity of innate motor behavior. Nature. October 12, 2016. [Epub]. |

