 |
Central serous retinopathy (CSR) is thought to be an idiopathic disorder typically found in the macula, characterized by a neurosensory detachment from the retinal pigment epithelium (RPE) and a localized pigment epithelial detachment (PED). Symptoms of CSR can include a loss of central vision, a central scotoma, micropsia, metamorphopsia, reduced color vision and reduced contrast sensitivity. Visual acuity may only be reduced moderately, and the refraction tends to reveal a hyperopic shift in most cases.1 Enhanced depth imaging optical coherence tomography (EDI-OCT), available for both spectral-domain (SD) and swept-source OCT, has demonstrated that patients with CSR tend to have thicker, larger diameter choroidal vessels (i.e., pachychoroid).
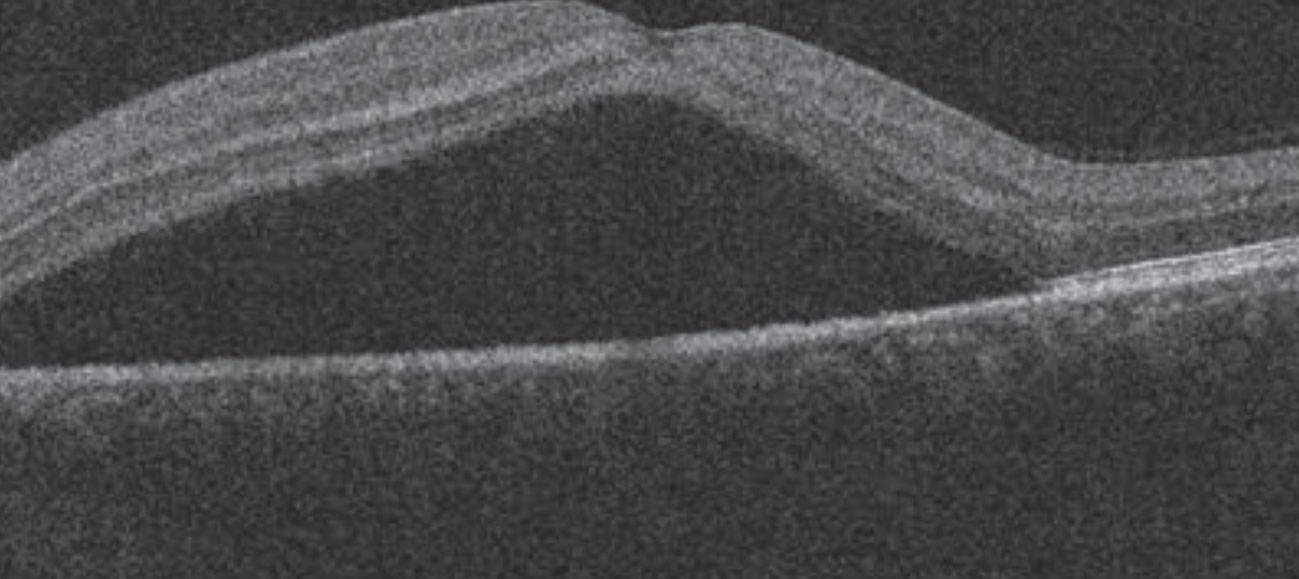 |
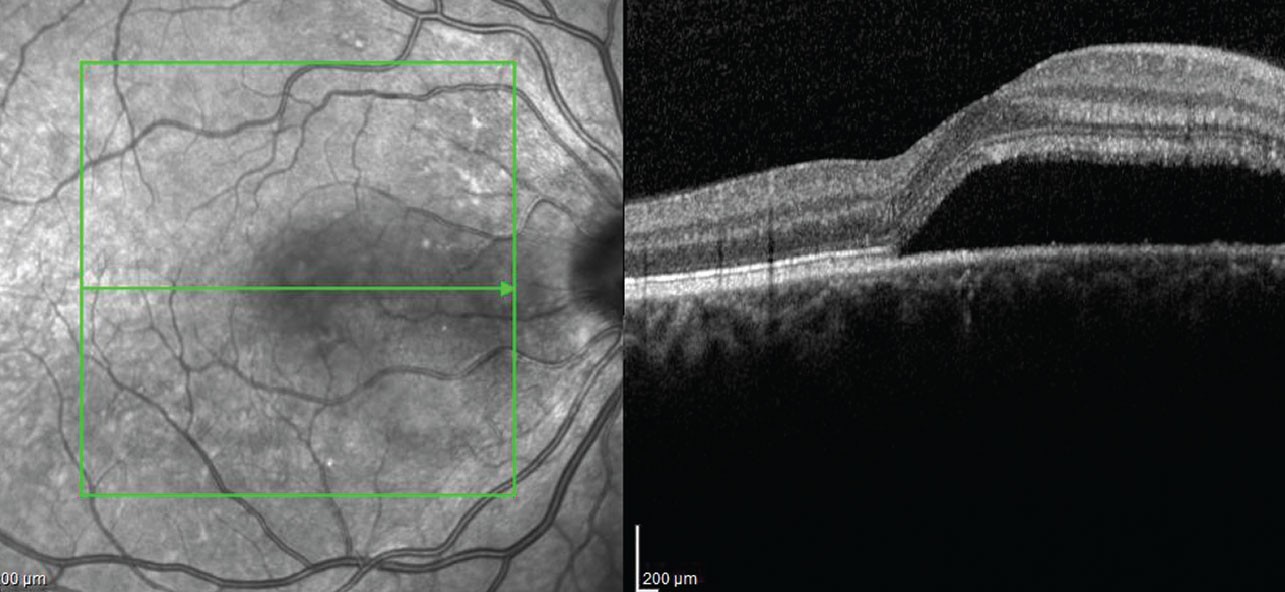
| Fig. 1. SD-OCT reveals a neurosensory detachment in the patient’s left eye. |
Risk factors associated with CSR include steroid use, increased caffeine consumption, higher stress levels (or a type-A personality trait), testosterone supplements, pregnancy, Helicobacter pylori ulcers, Viagra (Pfizer) use and obstructive sleep apnea. All of these risk factors can result in increased vascular permeability of the choroid, causing a localized PED, an accumulation of subretinal fluid or a neurosensory detachment.
When asking patients about any possible exposure to steroids, be sure to question them on the use of any products that may contain steroids, such as creams, inhalants, nasal sprays and joint injections. Research shows sleep apnea is present in up to two-thirds of patients with CSR and should be considered an associated risk factor, especially in patients who suffer from recurrent episodes of CSR or have chronic symptoms.2
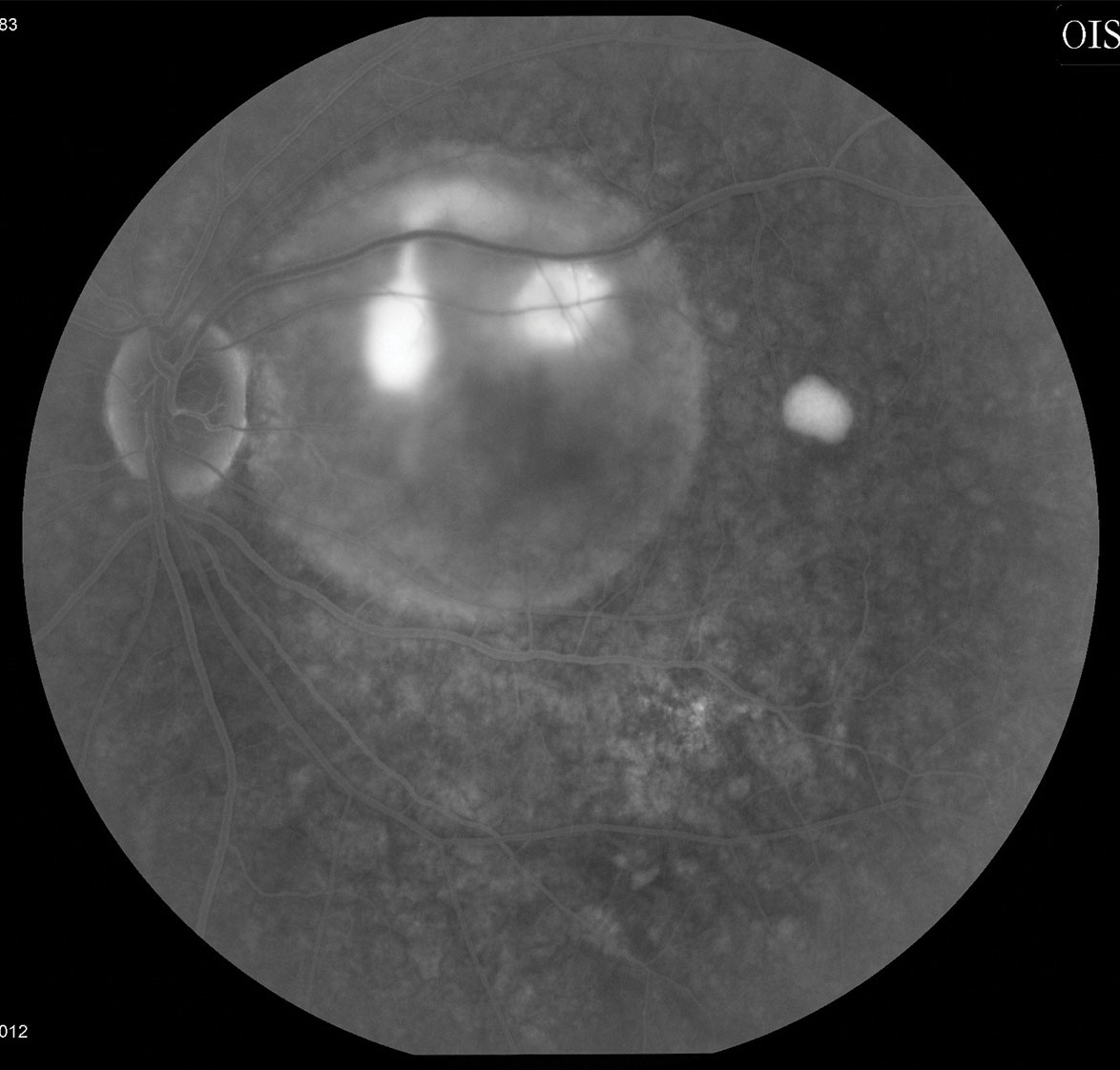 |
| Fig. 2. Fluorescein angiography shows focal leakage and a well-defined serous PED. |
In the clinical setting, CSR is classified as either acute or chronic (recurrent). In acute CSR, the visual symptoms are often self-limiting for one to four months; chronic CSR may cause more prolonged visual symptoms and a risk for permanent visual loss.
Although CSR is thought to be self-limiting in most cases, treatment should be considered in some cases. These include monocular patients, those that need a more rapid recovery in visual acuity to perform work or vocational tasks, those that have had a poor visual outcome from chronic CSR in the fellow eye or persistent subretinal fluid beyond three to four months.
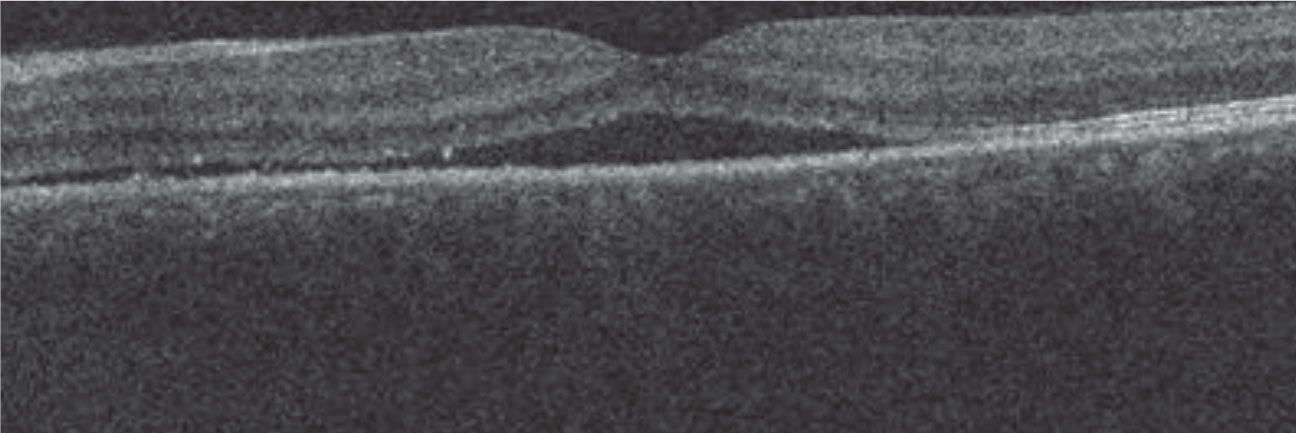 |
| Fig. 3. The patient’s neurosensory detachment was nearly resolved three weeks post-treatment. |
Treatment options for CSR include myriad systemic medications, such as the diuretics acetazolamide, eplerenone and spironolactone; the antibiotic rifampin; and the hormone supplement melatonin. Focal laser photocoagulation can also help with subretinal fluid absorption. Research also shows photodynamic therapy with the light-activated drug Visudyne (verteporfin, Bausch + Lomb) can be effective for CSR treatment.3
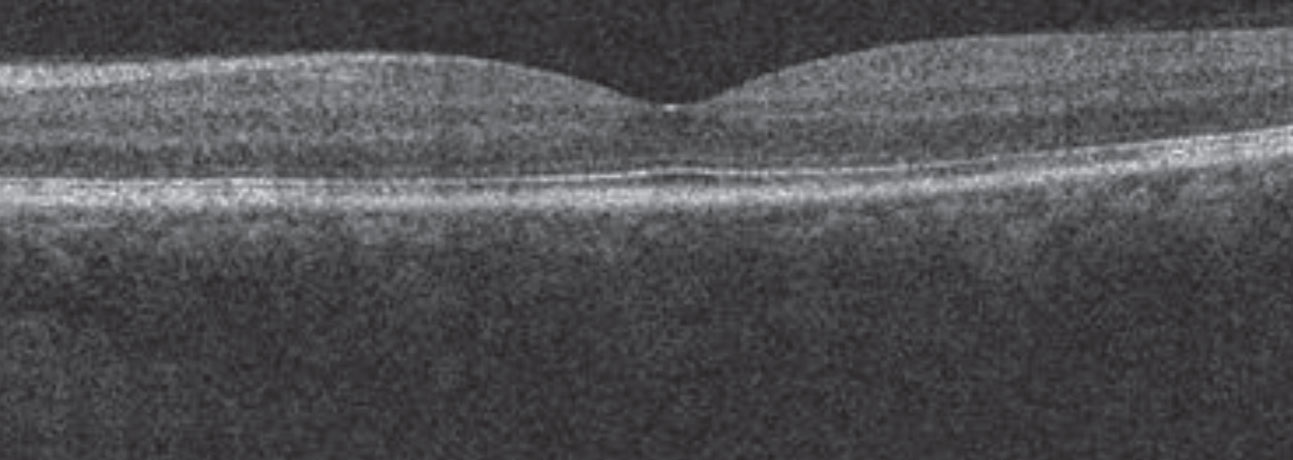 |
| Fig. 4. SD-OCT imaging of the patient’s left eye, pretreated with acetazolamide, one week after the Kenalog treatments. Note that the CSR remains inactive with no sub-retinal fluid detected. |
A Hairy Situation
Case by Dr. Haynie
A 42-year-old male presented to the clinic with a two-week history of vision loss in the left eye. His medical history included Kenalog (corticosteroid) injections in the scalp for the treatment of alopecia, an autoimmune disease characterized by hair loss. He reported that he developed vision loss three days after his treatment. His left eye’s entering visual acuity measured 20/60 and the intraocular pressure was 14mm Hg. Dilated examination revealed a serous macular lesion. OCT confirmed a neurosensory detachment with a pachychoroid; fluorescein angiography confirmed focal leakage and a well-defined serous PED (Figures 1 and 2). He was diagnosed with acute CSR secondary to the Kenalog injections.
Following a discussion of treatment vs. observation, he elected to be treated with oral acetazolamide 250mg QHS. At follow-up three weeks later, he reported some visual recovery to a level of 20/20- and OCT imaging confirmed near complete resolution of the neurosensory detachment (Figure 3).
As part of the management of CSR, I discussed avoiding any future Kenalog injections; however, he wanted to continue the treatment for alopecia. To avoid another acute CSR episode, I treated him with acetazolamide 250mg one week prior to his Kenalog treatment, which worked well long-term (Figure 4).
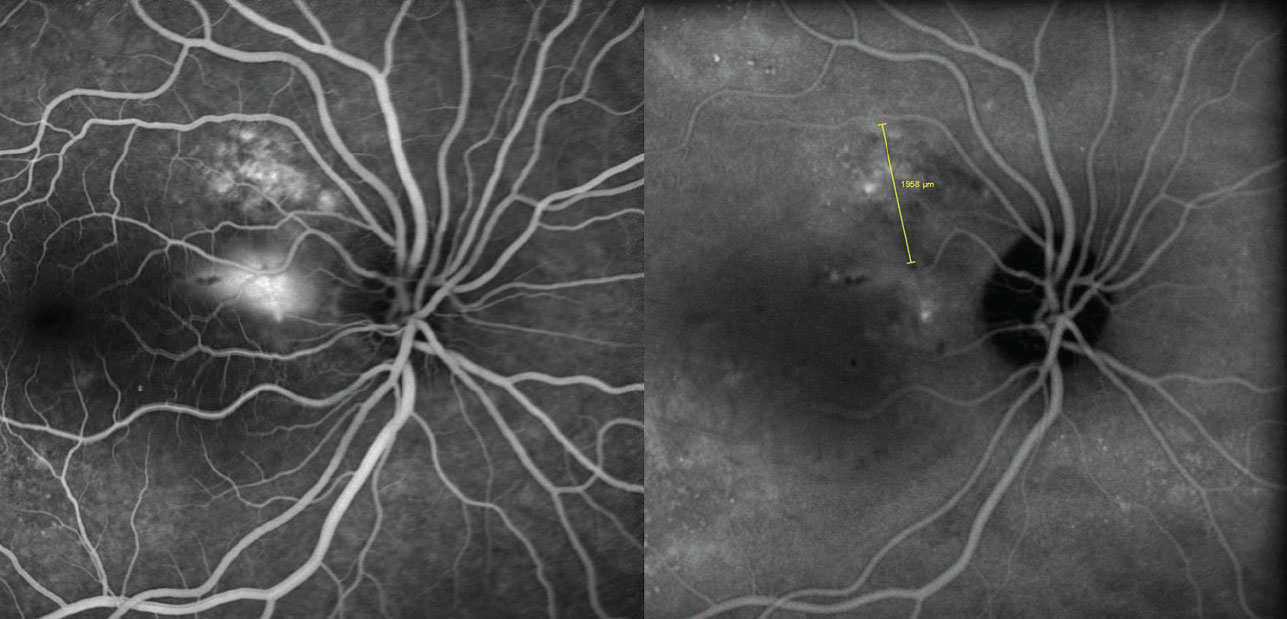 |
| Fig. 5. This patient’s ICG angiography reveals choroidal hyperpermeability. |
Lighting the Way
Case by Dr. Haynie
A 39-year-old female was referred for a retinal consultation after noting sudden vision loss in the right eye. Her history included a similar episode of vision loss the year prior, although it recovered spontaneously over two months. Her medical history includes osteoarthritis, gastroesophageal reflux disease and migraine syndrome. Her medications included Topamax (topiramate, Janssen Pharmaceuticals), Mobic (meloxicam, Boehringer Ingelheim) and Protonix (pantoprazole, Pfizer). Her visual acuity measured 20/50- in the right eye. Dilated examination revealed serous edema in the right eye involving the macula. Fluorescein angiography confirmed focal intense leakage, indocyanine green (ICG) angiography confirmed choroidal hyperpermeability in the peripapillary area of the choroid and SD-OCT confirmed a large neurosensory retinal detachment (Figures 5 and 6). These findings led to a diagnosis of recurrent CSR.
After discussing her treatment options, which could include observation, she elected to be treated with low-fluence photodynamic therapy based on the degree of vision loss and the recurrent nature of the condition. Six weeks following treatment, the neurosensory detachment had resolved (Figure 7). Fluorescein angiography and ICG angiography revealed cessation of the intense leakage with no evidence of activity (Figure 8). Her visual acuity improved to 20/20-.
 |
| Fig. 6. SD-OCT imaging uncovers a large neurosensory retinal detachment. |
Therapy Preferences
Commentary by Dr. Shechtman
Most CSR cases resolve spontaneously within three months without intervention. However, 30% to 50% of patients experience recurrence, which may be seen as guttering on fundus autofluorescence. Both recurrence and chronicity may lead to RPE atrophy in these patients, with associated permanent visual disturbance, in addition to increased risk of choroidal neovascularization.
While a variety of treatment options exist for chronic or recurrent cases of CSR, we find spironolactone 50mg QD and focal laser photocoagulation most effective in our practice. Studies show a relationship between mineralocorticoid (MR) receptors and choroidal vascular dilation, which collaborate to develop CSR. Thus, the use of an MR antagonist, such as spironolactone, can be an effective treatment option for chronic CSR. A recent study shows 83% of those treated vs. 8% of those observed had complete resolution of the CSR within two months. Given spironolactone’s status as a potassium-sparing diuretic, clinicians should consider evaluating the patient’s potassium level prior to its implementation.
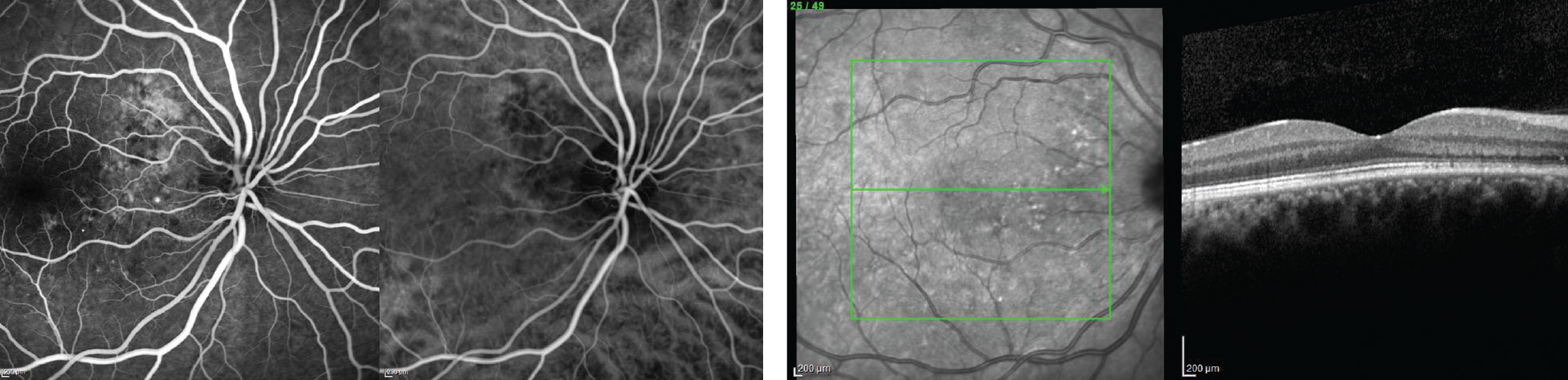 |
| Fig. 7. Six weeks after low-fluence photodynamic therapy, the patient’s neurosensory retinal detachment had resolved (left). Fig. 8. Treatment stopped the intense leakage, and no activity was noted six weeks after initiating therapy (right). |
In addition to spironolactone, focal laser photocoagulation applied to a “hot spot” seems to also be an effective option for patients with CSR. Fluorescein angiography is used to identify the presence of a hot spot, which shows up as hyperfluorescence at the site of RPE detachment. The focal RPE detachment must not involve the fovea. Although the treatment may lead to more rapid resolution, choroidal neovascularization may develop at the treatment site.
CSR can be a challenging condition to treat. Luckily, clinicians have many options that provide an opportunity to tailor therapy to the needs of each patient.
1. Wang M, Munch IC, Hasler PW, et al. Central serous chorioretinopathy. Acta Ophthalmol. 2008;86:126-45. 2. Yavas GV, Küsbeci T, Kaşikci M, et al. Obstructive sleep apnea in patients with central serous chorioretinopathy. Curr Eye Res. 2014;39(1):88-92. 3. Yannuzzi LA, Slakter JS, Gross NE, et al. Indocyanine green angiography-guided photodynamic therapy for treatment of chronic central serous chorioretinopathy: a pilot study. Retina. 2003;23(3):288-98. |

