Optometrists understand that floaters are usually not indicative of a serious health issue, but for patients—particularly those experiencing posterior vitreous detachment (PVD)—this annoying phenomenon can be a source of irritation and stress. And patients experiencing an influx of floaters are not rare.
Research shows by the age of 50, 50% of patients will have had a PVD, by the age of 65, 65%, and so on.1 Although these visual disturbances don’t permanently damage visual acuity, patients may complain that they have deleterious effects on their visual functioning and affect their abilities to read or drive, for example.2
In addition to keeping the eye healthy, optometrists are tasked with keeping patients happy with their vision—a significant influence on their overall quality of life.3,4 And so, when a patient’s primary complaint is an influx of floaters, it’s necessary that optometrists take patient concerns seriously, even for a rather benign condition.
It’s on us to not only describe what’s happening within the vitreous of their eyes but also to explain what technologies and techniques eye care physicians have in their toolbox to address floaters and explain whether they’re appropriate patient candidates for these procedures.
This article describes the development of these pesky floaters, what patients can achieve from undergoing a procedure to address them, how to co-manage patients through the process and, with an eye toward the ODs, expanding scope of practice, how to remove floaters using nd:YAG lasers.
 |
| This patient is about to undergo nd:YAG vitreolysis which will address an influx of floaters. For some patients, this procedure can relieve an irritating visual disturbance. Click image to enlarge. |
Weiss Rings
When a patient first presents with a symptomatic floater, education is vital. First, carefully examine the macula and peripheral retina to rule out any underlying issues, such as retinal detachment, that could threaten vision. If no such condition is found, discuss the neural-adaptation process along with the recommendation that they wait four to six months before considering treatment.5
When we are young, hyaluronan keeps collagen fibrils separated in the vitreous cavity, maintaining transparency of the vitreous.6 As we age, the process of vitreous liquefaction starts a breakdown in the collagen molecules causing those fibrous structures to clump into networks.6 The resulting process, PVD, is often marked by fibroglial tissue that’s left free-floating over the optic nerve, called a Weiss ring. This ring and other vitreous opacities cast shadows onto the retina that are perceived as floaters.7
The histopathological make-up may continue to change, pushing the floater out of the symptomatic line of sight, another reason to wait approximately six months to consider referring for treatment of symptomatic vitreous floaters.5
It’s also important to note that the risk of a retinal tear or detachment after an acute PVD is highest in the condition’s first six weeks and diminishes at six months.8
Thorough patient education is key to their understanding of the need to wait before considering treatment since a fresh PVD can be a very dramatic experience for a patient. This discussion must also assure the patient that floaters do not cause blindness or permanent vision loss. Most times when patients return a month later for follow up, they usually are not as anxious or bothered as the initial visit. Therefore, treating all symptomatic patients for their floaters from a PVD would lead to overtreatment, creating unnecessary risk of surgical complications.
Treatments and Risks
Standard of care obligates us to review risks, benefits and alternatives of any procedure with patients before proceeding. Until nd:YAG vitreolysis, pars plana vitrectomy (PPV) was the only option. Although vitrectomy is essentially a “cure” for floaters, retinal tears or detachments, hypotony, postoperative infection and cataract formation are all risks.9 These risks have been reduced with the advent of small incision techniques, which employ 27g wounds.7
Another option to discuss with patients suffering from persistent floaters is nd:YAG vitreolysis, a laser technique commonly used for opacity of the posterior capsule following cataract surgery. This procedure is currently within optometry’s scope of practice in a few states. Like any procedure, patient selection is key. Whether an optometrist is performing it or referring to a surgical center, they must take into account the specific pathology of the patient’s vitreous and retina. The most important test for this decision is a complete exam with dilated funduscopy.10 Before performing any laser procedure, it is recommended that the patient be free of active retinal pathology or chronic ocular inflammation.10
During the posterior exam, it is helpful to document any large floaters, syneresis or a Weiss ring suspended in the vitreous.10 Factors to consider are: the floaters’ proximity to the nerve and macula, phakic vs. aphakic anatomical lens, the symptomatic floaters’ depth in the vitreous (more anterior or posterior), the floater’s size and density, and the amount of liquefaction of (or “the percentage of liquid in”) the vitreous.10 Additionally, literature states the importance of documenting loss in contrast sensitivity over decreased vision.10 Lastly, you also want to proceed with caution on a patient who has strong lenticular astigmatism or keratoconus because either of these can make focusing your target beam very difficult.10
 |
| The patient, mid-procedure, is undergoing nd:YAG vitreolysis.Click image to enlarge. |
Selecting for YAG Vitreolysis
First of all, the patient must be symptomatic. These patients will report persistent moving shadows or vision-obstructing clouds of accumulated vitreal networks. Floater selection is critical, too. For best success with YAG vitreolysis, the patient must have a well defined floater—such as a Weiss ring or opaque amorphous cloud. Patients with web-like floaters present all throughout the vitreous are not ideal candidates for YAG vitreolysis.
It’s also the optometrist’s job, whether they perform the procedure or refer, to prepare patients who are selected with reasonable expectations. In our pratice, we tell these patients that they may need more than one treatment. Often, Weiss rings can be treated in one session, with larger opaque floaters or amorphous clouds taking multiple treatment sessions with the laser.
Limit any treatment to pseudophakic patients to avoid any risk of cataract formation from the abundant amount of laser energy used in the process. Avoid patients with multifocal lenses, because the lens’s multiple focal points will divide the nd:YAG laser beam.
 |
| This photo shows our patient’s eye immediately following the procedure. At this point, the patient should wait in the office for at least 30 minutes so doctors can recheck their IOPs. Click image to enlarge. |
Performing the Procedure
For the laser vitreolysis itself, maximum pupillary dilation is of the utmost importance. In our clinic we use 1% tropicamide and 2.5% phenylephrine to help achieve that goal. When you look into a vitreolysis lens, your view shrinks tremendously, as if looking through a straw. Therefore, having maximum dilation will save time and effort while locating the floater in question.
Using the right vitreous laser lenses is crucial to success with nd:YAG vitreolysis. Unlike a noncontact fundus lens whose image is inverted, the Ocular Karickhhoff 21mm or 25mm Vitreous Lens (Ocular Instruments) or the Singh Mid-Vitreous Lens (Volk Optical) create the necessary upright, virtual image.
Next, sit the patient as comfortably as possible behind the laser with a technician holding their forehead against the headrest. The patient could also be strapped in, but not all are comfortable with this. If performing the procedure, it’s helpful to locate the floater with a 90D lens behind the laser to orient yourself prior to placing the vitreolysis lens on the patient’s eye.
Then, just like any other contact lens, use proparacaine and goniosol or genteal gel prior to placing the lens on the patient’s eye. Maximum illumination is recommended to aid in your detection of the floater. Similar to a nd:YAG capsulotomy moving the light tower orientation can sometimes provide you with different views of the floater. Generally speaking, the illumination tower off-axis facilitates better viewing of anterior floaters, while on-axis facilitates better viewing of the floater in the mid- to posterior vitreous. We also find doing this important in locating the floater to orient the patients field of gaze to improve the field of view.
Once the floater is in focus through the optics, verify that your aiming beams are lined up prior to firing. The offset on your laser should be zero for mid-vitreous floaters. The more anterior the floater gets, the more posterior offset should be used, and vice versa.
The nd:YAG laser works by vaporizing floaters caused by plasma formation. Therefore, at lower power levels, the vitreous would be fractionated but not vaporized. Research shows that 2mJ to 6mJ of energy will lyse vitreal membranes in rabbits safely if the membranes are at least 2mm in front of the retina.12 To discern a floater’s distance from the retina, investigators recommend first bringing the floater into focus. If the retina is also in focus simultaneously, the floater is most likely too close to the retina to treat. But if the retina is not in focus, it’s likely that floater is located anterior enough to avoid retinal damage during treatment.13 Higher energy is needed to reach more posterior floaters, which increases your risk of damage to retinal structures.
It is recommended that the patient wait in the lobby for at least 30 minutes to recheck pressure before sending them home. A small percentage of patients do experience intraocular pressure (IOP) spikes after treatment. It’s common to instill two drops of an aqueous suppressant, such as brimonidine or dorzolamide immediately after the treatment for IOP spike prevention. Some doctors will prescribe a topical steroid such as Pred Forte 1% (prednisolone, Allergan) QID for a week or Durezol (difluprednate, Novartis) BID for a week. Because the laser delivers energy to inert proteins, not living tissue, patients theoretically experience no induced inflammation. Therefore, the topical steroid is not medically necessary (though we still prescribe it at our office).14
After the treatment is finished, the patient does not have any restrictions. Notify them that they may see a few dark spots in their vision, from the gas bubbles created during the procedure. Follow-up visits are typically scheduled at one week, one month then four months. Dilate the patient at each of these visits to monitor the retina for any breaks. It’s best to wait close to six months before ever repeating vitreolysis to fully evaluate the success of the initial procedure.
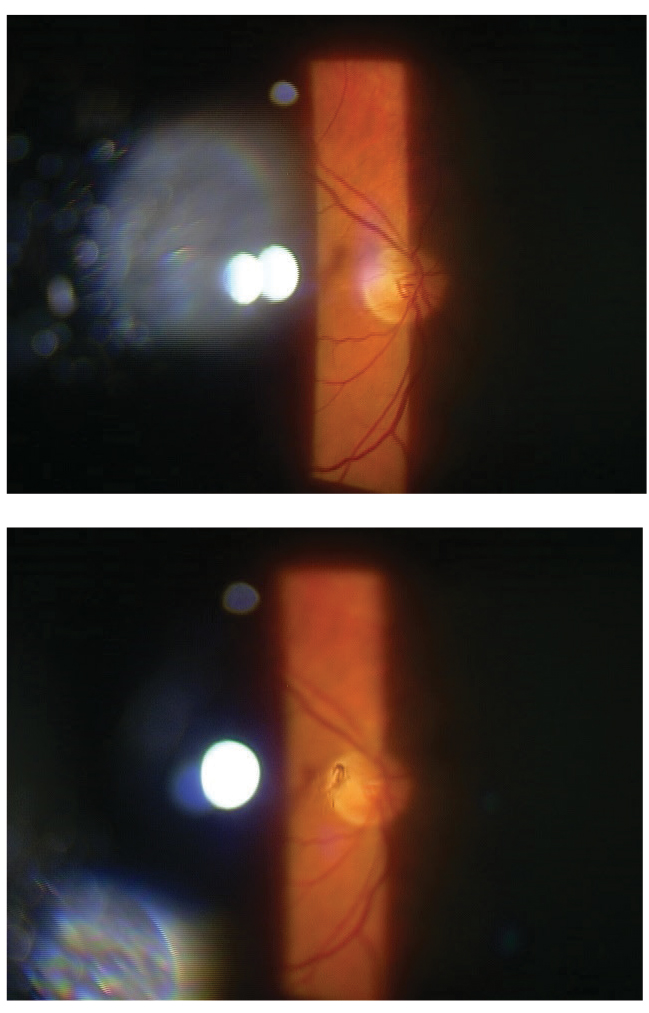 |
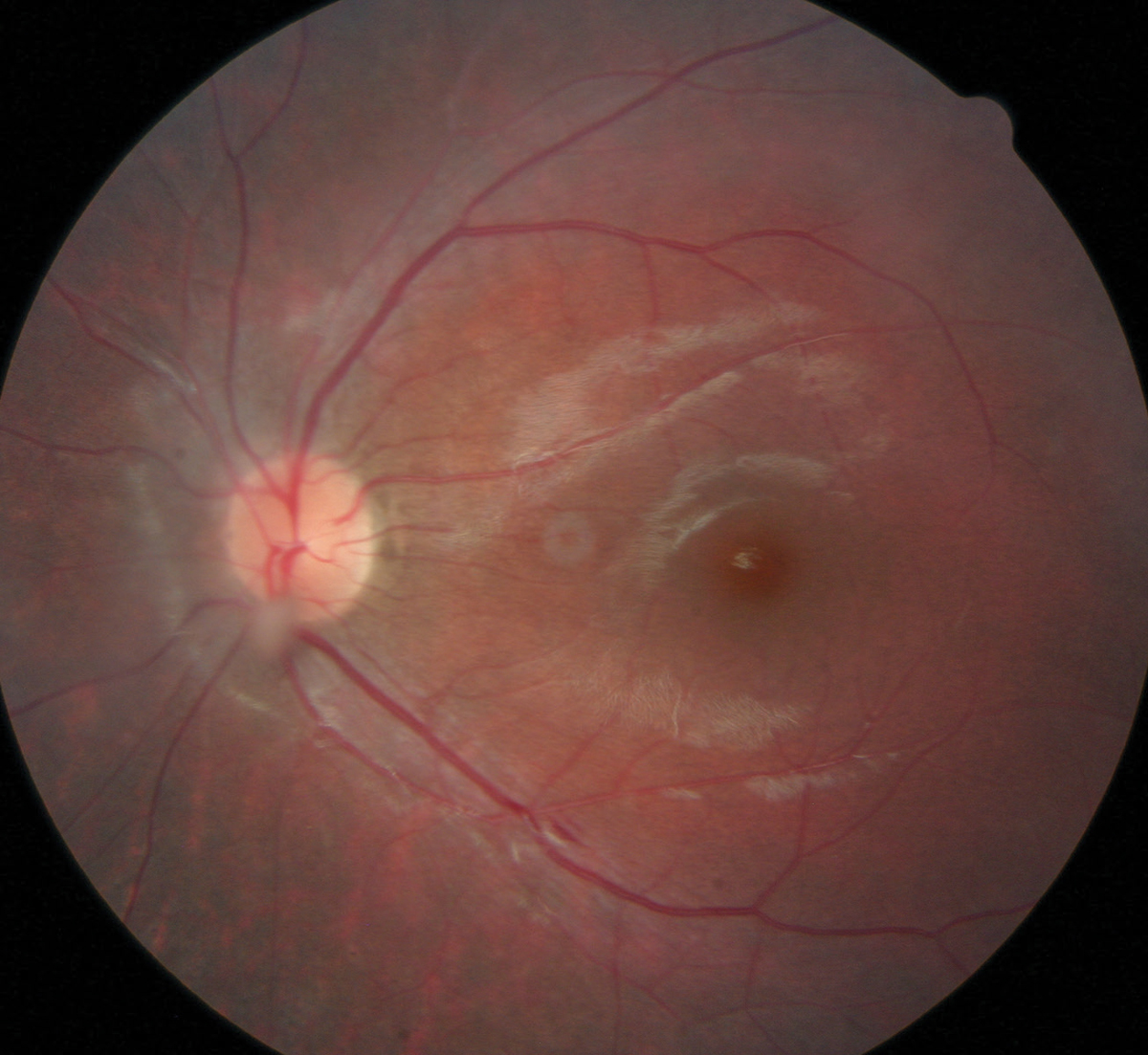
| This patient has a partial Weiss ring with PVD that displays a shadow on their retina. Click image to enlarge. |
Laser Dynamics
The treatment spot size and pulse width are fixed at 8µm and 4 nanoseconds. The only parameters that vary are the energy of the pulse and the number of pulses fired in one shot (i.e., single, double or triple). The Ultra Q Reflex (Ellex) and Tango Reflex (Ellex) lasers are optimized for viewing the vitreous because they allow for coaxial illumination, giving the operator the ability to view the floater and retina at the same time, providing the necessary spatial context needed for safe and efficacious treatments.15 Most treatments can be performed at between 2.5mJ and 6.5mJ energy and typically take 150 to 200 pulses to accomplish for symptomatic Weiss rings. More shots may be required for amorphous cloud floaters. More energy will be required if the floater is located deep in the posterior vitreous.16
The vitreous strand/opacity may move or become mobile during the laser treatment due to the shock wave introduced with each shot fired. It is best to wait until the floater settles back down before firing again. This is why it can take up to 30 minutes for just one procedure, depending on the nature of the floater and the treating doctor’s experience. These lasers also have an air-cooled cavity that enables thousands of shots to be fired without overheating or causing the laser to reset.
Measuring Results
One thing no doctor wants is an unsatisfied patient, which is why it’s vital to understand whether an objective measurement can be established for a patient’s subjective complaint. In fact, the anatomical improvement may not directly correlate with the treatment’s success.
Recently published research shows vitreolysis can, in fact, decrease both the amount of vitreous floater opacities seen on color fundus imaging and improve related symptoms.16 That research employed the National Eye Institute Visual Functioning Questionnaire 25 (NEI VFQ-25) responses of 32 patients to establish subjective successes.16 The investigators established a statistically significant improvement in the near visual function following laser vitreolysis.16 Also, the visual disturbance rate improvement showed a statistically significant reduction after the treatment.16 However, they note that distance visual function did not show a statistically significant difference after the procedure.16
 |
| Here, a floater can be easily seen just above the bottom part of the patient’s optic nerve head. This particular floater was too close to the retina, which contraindicated laser treatment. Photo by Katie West, OD. Click image to enlarge. |
On the objective side, the researchers used color fundus photography to determine whether vitreous opacity improved over time.16 Using this method, complete vitreous opacity improvement was observed in 18 eyes (56.2%), partial improvement in 12 eyes (37.5%) and no change in vitreous opacities in only two eyes (6.3%).16
That study also shows no elevation in IOP, retinal tears or detachment, significant visual decline or a recurrence of floaters during the follow-up period.16
A 2017 study shows that performing vitreolysis can subjectively improve Weiss ring-related symptoms and objectively improve Weiss ring appearance.17 That research shows 52 subjects split into two groups: one that received the laser procedure and a sham control group.17 A total of 19 patients in the nd:YAG laser group reported significantly or completely improved symptoms vs. zero in the sham group.17
As mentioned, the patient’s expectations must be managed beforehand. The 2017 research showed seven of the study’s patients who had residual postoperative floaters believed that those were just as bothersome as their original Weiss ring.17 Eight reported zero improvement in symptoms, even while seven of them had significant objective improvement based on before and after color photography as determined by a masked grader.17 This means that, for some patients, although a surgeon can vaporize most of a Weiss ring, some residual particles can bother the patient subjectively as much as the initial floater.18
Vitreolysis is a relatively new procedure. For some optometrists, knowing about what it can achieve will help them guide their patient and avoid complications. For those optometrists in the few states where it is within the scope of practice, directly providing them relief is possible. In either case, patient education before and after the procedure is critical. Remind patients that, depending on the floater, it may take multiple treatment sessions over multiple visits to significantly improve their symptoms. Patients are always reminded that YAG vitreolysis may not completely eradicate their symptoms but likely will offer a significant improvement.
Dr. Partin is residency trained and currently works at Oklahoma Eye Surgeons as a glaucoma and dry eye specialist.
Dr. Lighthizer is the Associate Dean, Director of Continuing Education and Chief of Specialty Care Clinics at the NSU Oklahoma College of Optometry.
| 1. Syed Z, Stewart M. Age-dependent vitreous separation from the macula in a clinic population. Clin Ophthalmol. 2016;10:1237-43. 2. Stuart A. To Treat—or Not to Treat—Vitreous Floaters. Eyenet Magazine. www.aao.org/eyenet/article/to-treat-or-not-to-treat-vitreous-floaters. March 2018. Accessed December 20, 2019. 3. Brown G. Vision and quality of life. Trans Am Ophthalmol Soc. 1999;97:473-511. 4 . Elliot D, Pesudovs K, Mallinson T. Vision-related quality of life. Optom Vis Sci. 2007;8(84):656-8. 5. Bergstrom R, Czyz C. Vitreous floaters. Treasure Island (FL): StatPearls Publishing; January 14, 2020 . 6. Tram N, Swindle-Reilly K. Rheological Properties and Age-Related Changes of the Human Vitreous Humor. Front Bioeng Biotechnol. 2018;6:199. 7. Shah CP, Heier JS. YAG laser vitreolysis vs sham YAG vitreolysis for symptomatic vitreous floaters: A randomized clinical trial. JAMA Ophthalmol 2017;135:9:918-923. 8. Bond-Taylor M, Jakobsson G, Zetterberg M. Posterior vitreous detachment – prevalence of and risk factors for retinal tears. Clin Ophthalmol. 2017;11:1689-95. 9. Wa C, Yee K, Huang L, et al. Long-term Safety of Vitrectomy for Patients with Floaters. Invest Ophthalmol Vis Sci. 2013;54(15):2142. 10. J Sebag, Yee K, Nguyen J, Nguyen-Chuu J. Long-term safety and efficacy of limited vitrectomy for vision degrading vitreopathy resulting from vitreous floaters. Ophthalmol Retina. 2018;2(9):881-7. 11. Delaney YM, Oyinloye A, Benjamin L. Nd:YAG vitreolysis and pars plana vitrectomy: Surgical treatment for vitreous floaters. Eye (Lond) 2002;16:1:21-26 12. Jeong Hun Bae, Park H, Kim J, et al. In vivo assessment of Pharmacologic vitreolysis in rabbits with the digital fluoroscopy system. Invest Ophthalmol Vis Sci. 2015;56(8):4817-22. 13. Lipuma L. Pearls for YAG vitreolysis of floaters. EyeWorld. www.eyeworld.org/article-. September 2015. Accessed December 12, 2019. 14. Singh IP. Neodymium YAG laser vitreolysis: retrospective safety study. ASCRS paper presentation. ascrs.org/resources/abstracts?field_abstract_year_value=2017&keys=&page=0%2C0&order=field_abstract_category&sort=desc. 2017. Accessed December 9, 2019. 15. Laser floater treatment. Ellex. www.ellex.com/us/treatments/laser-floater-treatment/. Accessed December 9, 2019. 16. Souza C, Lima L, Nascimento H, et al. Objective assessment of YAG laser vitreolysis in patients with symptomatic vitreous floaters. Int J Retina Vitreous. January 21, 2020. [Epub ahead of print]. 17. Shah CP, Heier JS. YAG laser vitreolysis vs. sham YAG vitreolysis for symptomatic vitreous floaters: a randomized clinical trial. JAMA Ophthalmol. 2017;135(9):918-23. 18. Bethke W. Vitreous floaters: what can be done? Rev Ophthalmol. 2018;25(4):48-51;83.1. |

