
|
|
Retina surgery has historically been a high-risk proposition, given the delicate nature of the retina and the relative crudeness of instruments used. No retina surgery is undertaken without significant risk, and less than ideal outcomes are an eventuality even with the most skilled surgeons.
However, the evolution of retinal surgery instruments has greatly aided surgeons in ensuring better outcomes. The general trend is to decrease the size of the handheld instruments to produce less collateral tissue disruption and allow more precise tissue dissection.
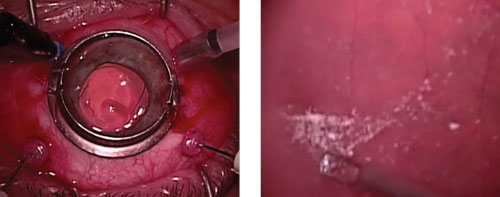 | |
| Trocar insertion (left) and membrane peel (right) using 27-gague instruments. Watch the video here. |
Vitrectomies are the most commonly performed retinal surgeries in the United States, and require surgeons to insert instruments through scleral tunnel incisions. Commonly, three or four incisions (often called ports) are made. If fluid is injected into the vitreous, suturing of these incisions will be required.
Every scleral incision carries with it the risk of retinal detachment and infection. Decreasing the size of the incisions should decrease the risk of sclerotomy-related tears and infections, especially endophthalmitis—a rare but devastating complication.
The other major benefit that comes with the adoption of smaller instruments is an increased ability to dissect tissue. Smaller instruments allow for more precise placement and manipulation of the remarkably thin layers of the retina/vitreous interface. Dissection of preretinal membranes is the most difficult portion of a vitrectomy, and is also the stage when most surgical related complications happen.
Although trivial to the average observer, the decreased size of the 27-gauge vitrectomy tool can be a huge advantage over the traditionally larger 25-gauge instrument class—which, not long ago, was itself a pioneering advance over previous generations of instruments (20- and 23-gauge).
Complex Case,
Smooth Sailing
In the accompanying video, Dr. Alan Franklin walks us though a vitrectomy in a patient with excessive diabetic fibrovascular proliferation throughout the retina. The video showcases the 27-gauge instrument’s ability to aid in dissecting the vitreous and tenacious preretinal membranes from the underlying mobile, detached retina. Another 27-gauge instrument is also then used to perform prophylactic panretinal photocoagulation with scleral indentation. A secondary benefit to the patient in this case: no sutures are needed at the sclerotomy site after the instruments are removed.
Due to the extensive manipulation of the retina in a case like this, postoperative retinal bleed or detachments are a concern. Close monitoring of the patient is needed in the post-op period while the patient uses topical steroids and antibiotics. Patients should be educated that visual fluctuation may be normal, but sudden or significant loss of vision should warrant an immediate evaluation.
Patients with this level of diabetic retinopathy are at high risk of future vision loss and need to be monitored closely. Risk factors for diabetic retinopathy progression should be reviewed by comanaging optometrists at follow-up visits; also encourage proper lifestyle maintenance.

