 |
A busy day at the clinic practically dares you not to fall behind schedule. On top of that, your caseload is full of complex patients, some presenting for the first time, with multiple issues. How do you juggle these responsibilities in an efficient yet non-cavalier manner, especially if your schedule, like mine, is packed with appointments backlogged by COVID-19? This column offers a case example that illustrates the importance of prioritizing patient care in a timely, beneficial way.
The Case
A 72-year-old Caucasian female presented as a new patient in mid-June. She wanted to establish care after recently moving to the area and heard that I specialize in glaucoma. She also needed an updated pair of glasses, as her current prescription was 2.5 years old and she noticed a change in her vision.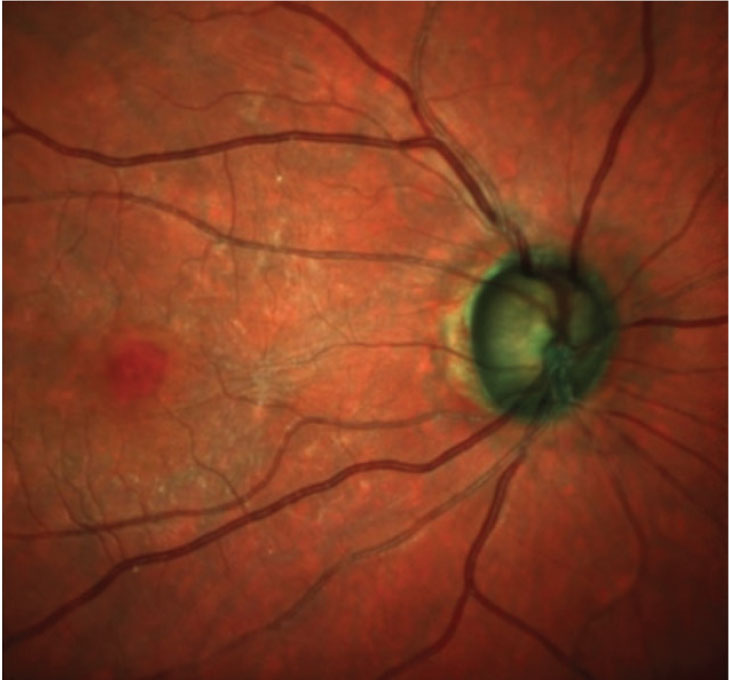 |
Fig. 1. Observe the thin neuroretinal rim and the ERM just nasal to the foveal avascular zone. Click image to enlarge. |
She was taking lansoprazole 30mg QD, levothyroxine 75mcg QD, simvastatin 40mg QD, citalopram 20mg QD, cetirizine 10mg QD, Vyzulta (latanoprostene bunod, Bausch + Lomb) HS OU and generic Cosopt (dorzolamide/timolol, Akorn) BID OD. She had no allergies to meds.
Significant in the patient’s ophthalmic history were bilateral cataract extractions with posterior chamber intraocular lens (IOL) implantations. Her right eye was done in 2009 and her left in 2019. A few years after her first cataract surgery, she had treatment with Jetrea (ocriplasmin, ThromboGenics) OD. During last year’s surgery, she also had two iStent devices (Glaukos) implanted in the trabecular meshwork of her left eye. This device was not available when her first eye was done.
The patient’s entering visual acuities were 20/40-2 OD and 20/25+1 OS and best-corrected acuities were 20/25+3 OD and 20/20-2 OS. Her pupils were equally round and reactive to light with no afferent pupillary defects, and her extraocular muscles were full in all positions of gaze.
Slit lamp examination of the anterior segment was fairly unremarkable. There was mild sectoral iris transillumination OD, which is not uncommon following cataract surgery. One of the iStent devices in the left eye was visible through the slit lamp without angle gonioscopy. The patient’s applanation tensions were 21mm Hg OD and 19mm Hg OS, and her pachymetry measures were 563µm OD and 551µm OS.
Through dilated pupils, the posterior chamber IOLs were clear and centered. The capsule in the right eye was opened, and the IOL was pitted from the YAG capsulotomy. The capsule in the left eye was clear and intact. Bilateral posterior vitreous detachments were noted.
Optic nerve exam demonstrated cup-to-disc ratios of 0.8/0.9 OD and 0.7/0.75 OS. The temporal neuroretinal rims were exceedingly thin (OD>OS) and consistent with advanced glaucoma (Figure 1).
The macular evaluation showed a foveal aberration OD consistent with a lamellar hole. There was also an epiretinal membrane (ERM) centered between the fovea and the disc OD (Figure 2). The left macula was characterized by RPE granulation. The retinal vasculature had both mild hypertensive and arteriolarsclerotic retinopathy OU. The peripheral retinal exam was normal OU.
Following the posterior pole examination, I retook the patient’s intraocular pressures (IOPs) and found that they were similar to pre-dilation measures.
There is no question that this patient has advanced glaucoma, OD>OS. Close examination of blue laser imaging shows significant loss of the retinal nerve fiber layer (RNFL) in the right eye (Figure 3). Though she’s only been in for one visit, I’m confident her IOPs are not adequately controlled, given the level of optic nerve damage.
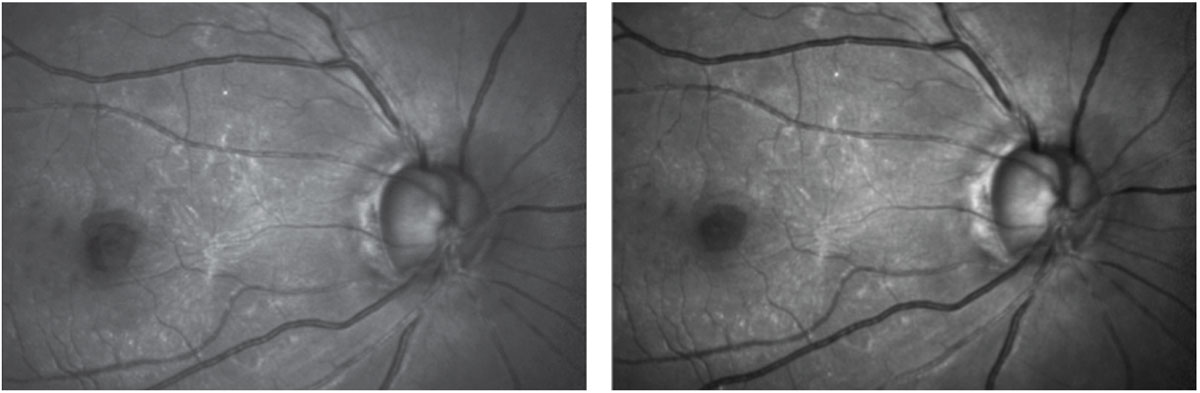 |
Figs. 2 and 3. Green laser imaging highlights the ERM and the foveal abnormality, at left. Blue laser reflectance imaging shows some fine striations remaining in the superotemporal sector of the arcuate retinal nerve fibers and very few nerve fibers remaining inferiorly. Click image to enlarge. |
Discussion
During an initial office visit, you need to be aware of the patient’s full clinical story. Only then can you determine and prioritize care, including what testing will be done, and when.
Each of us has developed protocols for certain situations and disease entities in our practices. At various times and with varying frequencies, all my glaucoma patients will complete a series of testing and imaging, including the obvious data points—IOP, visual fields, OCT and gonioscopy. They will also eventually undergo fundus photography, HRT-3 imaging (Heidelberg Engineering) of the optic nerves, anterior segment OCT and ultrasound biomicroscopy. That’s a lot of data, and certainly too much to obtain over a few visits, let alone on the initial presentation.
Compounding the issue of figuring out an appropriate testing schedule is the fact that certain items are not covered by insurance when performed on the same day as other items. For example, Medicare will not pay for OCT and fundus photography in the same sitting (for the same disease). Regardless, patient care and well-being trumps coding and reimbursement issues, so if OCT and imaging need to be done on the same day, then so be it.
Keep insurance coverage in mind when deciding which tests are needed right away and which can wait. To a large extent, this depends on the patient and how advanced their disease is, how controlled their IOPs are and other clinical signals. We also need to be mindful of juggling multiple patients and managing office flow, as there will inevitably be other patients in the clinic at the same time and we can’t get bogged down with one at the expense of three others.
Patient Management
An adjustment to the patient’s spectacle prescription should improve her sight, so I updated her prescription to get new glasses. The bigger issue at hand is her advanced glaucoma. This is how I prioritized her initial testing:
- Pachymetry to get a sense of her IOPs and progression risk
- Photography in the form of multimodal laser imaging to see (and record) what’s happening in the neuroretinal rim, macula and RNFL
- IOPs to get a feel for how tenuous her IOP situation is, knowing full well that when I saw her in the afternoon, her IOPs were probably higher earlier in the day
- Slit lamp examination of the posterior pole to get an idea of how things look in vivo
Her next visit will include:
- IOPs to document her diurnal fluctuations
- Standard automated perimetry 24-2 visual field thresholds to assess the extent of vision loss
- OCT and HRT-3 imaging of the optic nerves and OCT imaging of the macula to quantify the glaucomatous damage
- Gonioscopy to evaluate the nuances of her angles and the positions of the iStents OS
At the completion of the second visit, I should have a reasonable set of data points that I can use to set and start working toward a target pressure for the patient.
There is a lot to take into consideration when juggling different conditions and patients, especially the first time around. Luckily, the more cases we see, the easier it will become to prioritize testing.

