 |
An 18-year-old male presented for evaluation of a red and irritated left eye. He had a history of brain damage and seizures from birth, and only a minimal history could be elicited.
Upon examination, his best-corrected vision was 20/20 OD and 20/60 OS. Confrontation visual fields were full to careful finger counting in both eyes; pupils were equally round and reactive to light. No afferent pupillary defect was found. Intraocular pressure (IOP) was 15mm Hg OD and 8mm Hg OS.
Slit lamp examination of the right eye was unremarkable. The left eye was positive for 3+ episcleral injection and 3+ cell and flare in the anterior chamber (Figure 1).
On dilated fundus exam, the right eye was completely normal. The left eye had 1-2+ vitreous cell and haze, with tortuous vasculature and mild disc edema. Mid-peripherally in the superior nasal quadrant, a white lesion was visible (Figure 2). The retina was attached.
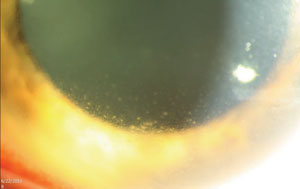 | |
| Fig. 1. An 18-year-old male’s irritated left eye brought him to our office. What does his anterior segment presentation tell you about his likely diagnosis? |
Take the Quiz
1. What are the findings seen on the retinal photograph of the left eye?
a. Retinal necrosis with intraretinal hemorrhage.
b. Roth spot.
c. Choroidal osteoma.
d. White without pressure.
2. What is the correct diagnosis?
a. Choroidal metastases.
b. Toxoplasma chorioretinitis.
c. Acute retinal necrosis.
d. Leukemia.
3. How should he be treated?
a. High-dose antivirals tapered to a lifetime prophylactic dose.
b. Pyrimethamine, sulfadiazine and corticosteroids.
c. Plaque radiotherapy.
d. Referral to oncology.
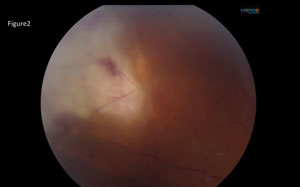 | |
| Fig. 2. What do these peripheral retinal findings represent? |
4. What is this patient at increased risk of developing?
a. Choroidal neovascular membrane.
b. Metastatic cancer to the liver.
c. Serous retinal detachment.
d. Rhegmatogenous retinal detachment.
For answers, see below.
Discussion
Based on the clinical findings, we suspected that our patient had acute retinal necrosis (ARN). An anterior chamber tap was performed and sent for culture. The patient was treated empirically with 900mg IV acyclovir, and started on 1g PO of valacyclovir TID. To treat his anterior segment inflammation he was started on atropine QID and prednisolone acetate QID in the left eye. At follow-up, three days later, 40mg of oral prednisone was added after consulting with the patient’s pediatrician.
The diagnosis of ARN is generally made based on The clinical triad of progressive retinal necrosis, vitritis and occlusive vasculopathy in an immunocompetent individual between the ages of 20 and 60.1 It is attributed to herpes simplex virus (HSV) or varicella zoster virus (VZV) infection. Our patient’s culture was positive for HSV type 2, which was present from birth.
ARN has an acute onset with a predilection for the peripheral retina and usually self-resolves within six to 12 weeks.1 It is followed by a late cicatrizing phase in which 30% to 50% of patients will develop a rhegmatogenous retinal detachment, usually within three to six months. The patient should be followed closely with dilated exams.1,2
 | |
| Fig. 3. Retina appearance after recent barricade laser treatment. |
Treatment
Historically, the standard treatment for ARN was intravenous acyclovir for five to 10 days, followed by oral acyclovir as prophylaxis for the fellow eye.2 Since the advent of antiviral medications with better bioavailability, many physicians have adopted the protocol of one to two grams of valaciclovir TID for a minimum of six weeks, as it provides comparable efficacy with less frequent oral administration.2
In cases of significant vitritis or papillitis, doctors may supplement with oral prednisone.2 You may also consider topical steroids and cycloplegics for significant anterior chamber reaction. Systemic aspirin is another option to combat the arteriolar occlusions.1
Generally, patients should respond in one to two weeks and experience resolution of the acute retinitis around one month after initial therapy—though doctors should perform dilated exams frequently for several months through the cicatricial phase to monitor for retinal tear or retinal detachment.1,2
Prophylactic laser barricade has occasionally been used to prevent subsequent retinal detachment, but the success in preventing retinal detachment is not clear at this point.1
Other surgical options, such as scleral buckle and vitrectomy, are reserved only for cases that progress to retinal detachment.1
Reports of second eye involvement range from 3% to 33% depending on treatment modality, warranting long-term prophylaxis.1,2 Prognosis for ARN patients is dependent on the amount of retinal necrosis, presence of retinal detachment and involvement of the fellow eye.1
Our patient required barricade laser early on and developed a total retinal detachment 10 months after initial presentation (Figure 3). A pars plana vitrectomy, lensectomy, silicone oil fill, scleral buckle, endolaser and intravitreal injection of foscarnet and ganciclovir was performed. The patient remains on a prophylactic dose of 500mg valaciclovir QD. The left eye has remained stable at 20/100 and the right eye remains uninvolved.
Dr. Hammond is an optometric resident at the Bascom Palmer Eye Institute in Miami.
1. Vemulakonda GA, Pepose JS, Van Gelder RN. Acute Retinal Necrosis Syndrome. In: Ryan SJ ed. Retina. Vol 2, ed. V. St Louis: Mosby;2013:1523-9.2. Taylor S, Hamilton R, Hooper C, et al. “Valacyclovir in the Treatment of Acute Retinal Necrosis.” BMC Ophthalmology 12.1 (2012):48.
Retina Quiz Answers:
1) a; 2) c; 3) a; 4) d.

