 |
Watery eyes, known as epiphora, seems like a misnomer for dry eye disease (DED), which can be very confusing to patients. It’s imperative that we first determine the cause of the epiphora so we can properly educate patients and provide them the best treatment options. If it is caused by dry eye disease, or more specifically lipid layer deficiency causing the lacrimal gland to upregulate, then it becomes very important to educate the patient that their eyes are tearing due to a lack or decrease of one of the components of the tear film. If it’s not caused by dry eye, the appropriate management or referral must be made.
Causes
Epiphora is typically a multifactorial issue with many causes.1 Four general categories include: (1) lid apposition issues, (2) nasolacrimal duct obstruction or stenosis, (3) dry eye disease and (4) a broad category we’ll define as something you’d see on a slit lamp examination such as trichiasis or allergic conjunctivitis. A large-scale study showed that epiphora causes included lower lid malposition (33.3%), nasolacrimal/canalicular obstruction (29%), multifactorial (22%), punctal stenosis (11%) and reflex tearing (4.7%).1 It also showed that women tended to experience epiphora at a younger age than men and the primary cause of their epiphora was punctal stenosis compared with men (34.6% vs. 22.4%); however, more men had eyelid malposition than women (39.5% vs. 27.9%).1 Let’s look at all the potential causes.
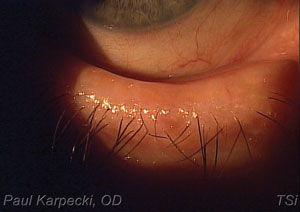
Slit Lamp Findings. The first step is to rule out the non-dry eye causes. During your slit lamp exam look for a turned-in lash (trichiasis) that requires epilation or a foreign body.
 | |
| A diagnosis of ectropion, as seen here, may warrant surgical tightening. |
One very important cause of excessive tearing is conjunctivochalsis, or folds in the conjunctiva due to a loss of Tenon’s.2 Conjunctivochalsis can often advance to the point of resting on the lower eyelid. If this is present, the patient requires a surgical procedure to tighten the conjunctival tissue via resection or cautery. Most cases of conjunctivochalasis can be monitored, but once it causes a foreign body sensation or persistent epiphora, it should be surgically treated.
Lower Lid Malposition. The presence of ectropion or entropion also warrants a referral to an oculoplastic surgeon for repair. Ectropion and entropion are typically diagnosed on presentation; however, pre-clinical or early cases of lid laxity may cause epiphora sooner. You can conduct two tests to reveal early cases of ectropion or entropion in patients with epiphora. To induce entropion, have a patient forcefully blink or close their eyes and note if the eyelid turns in. To check for lid laxity or early ectropion, pull the lower lid away from the globe and see how quickly it snaps back. If it remains out for an extended period of time, this is a diagnosis of lower lid laxity and may require surgical tightening in cases of persistent epiphora. This seems to be very effective, although ectropion may potentially recur.3
Nasolacrimal Duct Obstruction. The third category is obstruction of the nasolacrimal duct system preventing tears from draining. In the past, tests such as the Jones test I and II were used to help determine if the nasolacrimal duct (NLD) system was clear or not. Today, you can simply instill sodium fluorescein (NaFl) dye and leave it in place for five to 10 minutes. In a person with an open canal, the dye should drain in that time (five minutes for a non-dry eye disease patient and 10 minutes for a patient with DED because of their slower clearance). After five or 10 minutes the clinician should gently press upward along the lower lacrimal sac; if NaFl dye regurgitates back through the punctum, this is a positive sign of obstruction. The patient should then receive a dilation and irrigation procedure. If that does not open the NLD, refer to an oculoplastic surgeon for dacryocystorhinostomy.
 | |
| Conjunctivochalasis, a common cause of excessive tearing, may require surgical tightening of the conjunctival tissue. |
Evaporative Dry Eye. Finally, if all of these tests and findings are negative, your next step is ruling out evaporative dry eye. Effective testing includes osmolarity testing, tear film break-up time, meibomian gland expression, lipid layer interferometry or meibography. If evaporative dry eye is indeed present, have the patient begin a lipid-based tear every two to four hours per day and an anti-inflammatory medication such as a corticosteroid or cyclosporine and see if the tearing subsides.4
Explain to the patient that they are deficient in one of the layers of the tear film, known as the oil layer, and the body is trying to compensate for this by over-producing aqueous; by treating the inflammation and supplementing the oil layer, you will soon know if evaporative dry eye is the cause. If true evaporative dry eye is present, it should be treated long-term and should include options to address obstruction such as commercial warm compresses, manual expression or thermal pulsation treatments, cyclosporine, omega-fatty acids, lid hygiene and tear supplementation.5 In non-responsive conditions, and although not performed routinely, studies have shown a benefit to injecting the lacrimal gland with botulinum toxin.6 Although the results are temporary, the patient satisfaction rates are very high.
Although there are other causes of chronic epiphora, these four categories likely account for more than 95% of the potential underlying pathologies.7 By testing for each one and taking the appropriate management steps, you can help patients find relief from the irritation and frustration of epiphora.
1. Nemet AY. The Etiology of Epiphora: A Multifactorial Issue. Semin Ophthalmol. 2015 Aug 21:1-5. [Epub ahead of print].2. Chhadva P, Alexander A, McClellan AL, et al. The impact of conjunctivochalasis on dry eye symptoms and signs. Invest Ophthalmol Vis Sci. 2015 May;56(5):2867-71.
3. Narayanan K, Barnes EA. Epiphora with eyelid laxity. Orbit. 2005 Sep;24(3):201-3.
4. McCann LC, Tomlinson A, Pearce E et al. Effectiveness of artificial tears in the management of evaporative dry eye. Cornea. 2012 Jan;31(1):1-5.
5. Korb DR, Blackie CA, Finnemore VM, et al. Effect of using a combination of lid wipes, eye drops, and omega-3 supplements on meibomian gland functionality in patients with lipid deficient/evaporative dry eye. Cornea. 2015 Apr;34(4):407-12.
6. Wojno TH. Results of lacrimal gland botulinum toxin injection for epiphora in lacrimal obstruction and gustatory tearing. Ophthal Plast Reconstr Surg. 2011 Mar-Apr;27(2):119-21.
7. Tse DT, Erickson BP, Tse BC, et al. The BLICK mnemonic for clinical-anatomical assessment of patients with epiphora. Ophthal Plast Reconstr Surg. 2014 Nov-Dec;30(6):450-8.

