 |  |
Epiretinal membranes (ERMs) are caused by defects in the surface layer of the retina. Glial cells are released, migrating through and developing a membranous sheet on the retinal surface. They may look like a piece of cellophane, a wrinkle or puckered folds on the retina.
ERMs are one of the most common reasons to refer a patient for a retinal consultation. Historically, most optometrists waited until a patient’s best-corrected visual acuities were life-limiting before sending them for a surgical consultation. This delay was due to the risks associated with surgical intervention and the limitations of visual recovery.
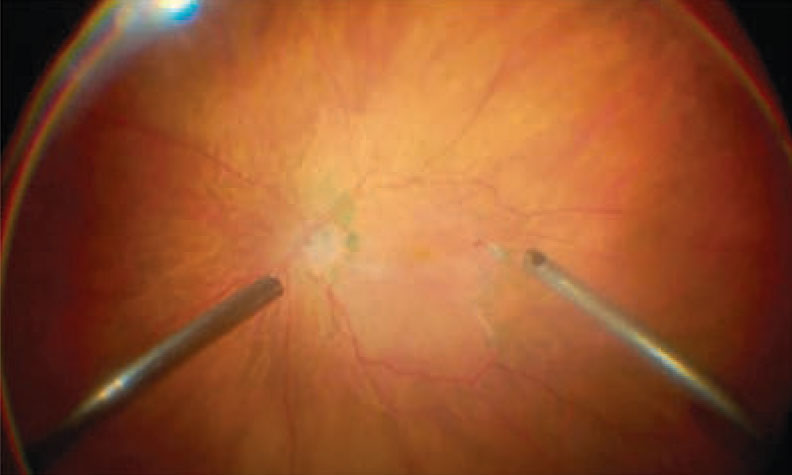 |
| New techniques limit the risks associated with surgical intervention for ERMs. Click image to enlarge. |
The threshold for recommending surgery, however, has changed dramatically over the last few decades. More precise instruments coupled with better imaging systems have effectively lowered the risks that come with surgery. These advancements have also led to much better re-establishment of macular architecture in even the mildest cases of ERM. It’s not uncommon any more to refer a patient for membrane peel surgery who has a best-corrected visual acuity around 20/20 but suffers from metamorphopsia.
Surgical Intervention
Many great innovations are now available to assist retinal surgeons in removing ERMs, such as the 25-gauge Finesse Sharkskin ILM Forceps (Alcon). With smaller instruments and faster cutting speeds, surgeons can use less force when separating retinal layers and attempt to peel membranes that would otherwise be considered too risky.
Surgeons now use fine forceps to tease away strong adhesion areas and a green dye for better visualization of the internal limiting membrane. Partway through the procedure, surgeons can change the color channel for better visualization of the dye that stains the internal limiting membrane. The macula appears paler once both the internal limiting membrane and ERM are removed.
With this technique, surgeons can remove both of these layers in one step as opposed to two, which was typical of the procedure up until this point, and ensure complete removal of the membrane with the best chance of re-establishing normal foveal architecture.
Due to the advancements in instrumentation, postoperative sutures are no longer required for ERM surgery. This allows for a much more comfortable and smoother post-op experience. Although the surgery is usually performed in a hospital or surgical center, it is an outpatient procedure.
While the patient can lead a relatively normal life starting the following day, post-op restrictions include Valsalva-type straining and swimming for two weeks. Medications include topical antibiotics and anti-inflammatories for several weeks.
Complication risks are small, with about one in 100 patients developing retinal detachment and one in 2,000 developing infection post-surgery.1 Those who still have their natural lens have an increased risk of cataract progression.1
Any amount of macular structural integrity loss that causes visual consequences should warrant a conversation about the potential risks and benefits of surgical intervention. Even the subtlest levels of visual distortion can often be improved with minimal risk to the patient thanks to new advances in the field.
| 1. American Society of Retina Specialists. Epiretinal membranes. www.asrs.org/patients/retinal-diseases/19/epiretinal-membranes. Accessed September 3, 2020. |

