With everyone’s eyes perpetually scanning the myriad of glowing screens around us, dry eye symptoms are getting worse and affecting younger demographics than ever. For the optometrist, these habits make it more likely that a patient with dry eye will appear in your chair complaining of fluctuating vision, redness, foreign body sensation and even pain.
According to the most recent Tear Film and Ocular Surface Society International Dry Eye Workshop II (TFOS DEWS II), dry eye disease (DED) is characterized by a loss of homeostasis of the tear film.2 By discovering and understanding the underlying etiology—whether due to hormonal changes, contact lens intolerance, dysfunction of the meibomian glands or other reasons—using a targeted work-up and approach towards management is the only effective way to improve patient symptoms and clinical signs.
Management of these patients is not “one size fits all,” and requires significant tailoring to each patient’s symptoms, severity and lifestyle. Often, practitioners advise patients to first use artificial tears, up to four times a day. If used properly, tear supplementation therapy may increase lubrication; however, in some cases, they alone may not alleviate all complaints.
In most dry eye cases, practitioners will often apply vital dyes to assess for corneal staining to determine tear break-up time. Although this offers valuable information, a thorough eyelid assessment is also necessary to determine additional contributors to the patient’s signs and symptoms. This article provides a guide through a variety of eyelid findings and evaluation techniques that can alter your typical management approach and provide the relief your patients are seeking.
 |
| Korb-Blackie test indicating incomplete closure of the eyelids due to light being seen emanating from the lid margin of the right eye. |
Incomplete Blink
Corneal staining with sodium fluorescein, particularly in the inferior one-third of the cornea, often arises from incomplete blink and closure. Even just asking a patient to close their eyes under high magnification, or watching their blink rate and pattern, can provide insight. If poor closure, incomplete blink or infrequent blinking is present, the patient may be suffering from the effect of the lids poorly distributing the tears along the ocular surface, or from lagophthalmos during sleeping hours, both causing chronic dryness.
Even if the eyelids appear to have complete closure, the Korb-Blackie light test can discern if the patient has incomplete closure, if any, and to what degree.1 By resting a transilluminator along the patient’s closed eye, light escaping from the lid margin indicates a lack of closure. Thicker artificial tears in the form of gels or ointments for overnight use are available for these cases. Lid-taping regimens when the patient is asleep, and moisture goggles for more severe cases, can also help.
 |
| Meibography images of the upper and lower eyelids indicating mild gland tortuosity and dilation. |
Meibomian Glands
Keratinized—or capped—meibomian glands are an easily discoverable finding, which can indicate meibomian gland dysfunction (MGD) as a component to the patient’s dryness. If the glands themselves are clogged and unable to secrete the lipid component of the tear film, tear evaporation time will likely be compromised. Heat masks may be effective in liquefying material trapped in the glands and help express meibum.13
Lipiview (Tearscience), Keratograph (Oculus) and Meibox (Box Medical Solutions) are some of the options doctors use to evaluate the glands for tortuosity, dropout or atrophy. However it’s accomplished, meibomian gland imaging should be part of your work-up on all patients, no matter the age.5 This protocol can help establish baseline information and potentially uncover signs prior to the onset of symptoms.
Lipid-based artificial tears can help patients battle underlying gland dropout or dysfunction, as the oily components in these drops can help thwart evaporation of tears from the ocular surface.
Even prior to performing any dry eye work-up or instillation of dyes, using the high magnification with biomicroscopy to view the eyelids is helpful. In addition, by manually moving the eyelids and assessing the meibomian glands and palpebral conjunctiva, complete with lid eversion, more details are revealed. It is critical not only to assess the cornea with fluorescein staining, but also to assess the eye with lissamine green stain. Unlike sodium fluorescein, lissamine will allow for visualization of the devitalized cells of the bulbar and palpebral conjunctiva. Staining of these areas may indicate extreme global dryness that can be missed on standard fluorescein staining.
Papillary Reaction
Foreign body sensation or irritation in the eyes can masquerade as a papillary reaction, with or without seasonal allergies. Although papillary reactions are often associated with symptoms such as ocular itching, some patients may have difficulty in expressing their symptoms, and if papillae are present, it is important to consider an antihistamine/mast cell stabilizer combination drop to improve ocular comfort. More severe presentations—namely, giant papillary conjunctivitis—may occur, typically with soft contact lens wear, due to frictional forces or protein hypersensitivity. A steroid may be warranted in these cases, depending on the level of severity of patient symptoms and clinical signs. Monitoring the appearance of the palpebral conjunctiva is critical to a patient’s success and specifically in avoiding contact lens intolerance.
On the Lashes
Often overlooked, the lashes too can offer clues on what might be exacerbating a patient’s symptoms. For example, if trichiasis exists, positive sodium fluorescein staining near the lash margin may be confused with lagophthalmos or incomplete blink, based on corneal signs alone.8 However, if rogue lashes are noted, epilation or (in severe cases) surgical manipulation may be necessary to relieve the globe from irritation.
If debris is present, depending on the shape of the scurf (or collarettes), a practitioner must determine whether the underlying etiology is seborrheic (flaky debris) or secondary to Demodex (round, tubular debris found at the base of the lashes). Although Demodex presence was originally thought to be a symbiotic relationship, patients with more prominent Demodex are found to have a higher likelihood of inflammatory markers in the tear films, with increased symptoms of dryness compared to those with reduced Demodex levels.7 Lid scrubs, such as from Ocusoft or Avenova, are options to assist in eyelid hygiene in cases of blepharitis. Similarly, if Demodex is noted, research shows tea tree oil scrubs can be effective in reducing a patient’s ocular surface discomfort index (OSDI) score and improve symptoms.7
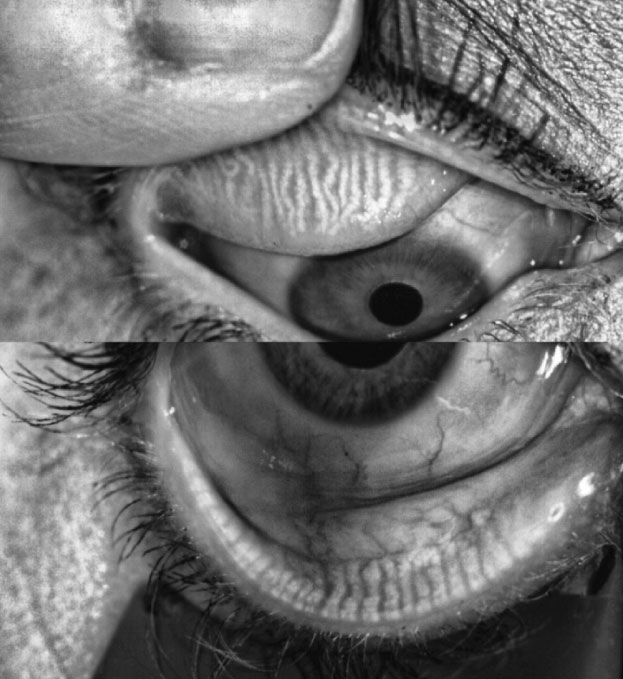
Lid Wiper Epitheliopathy
This disturbance of the eyelid margin affects the portion of the lid that is essential for spreading tears across the globe. This finding can be seen in patients with abnormal eyelid structures, dry ocular surfaces or a history of contact lens wear.3 By using lissamine green staining, significant dryness can be discovered secondary to frictional and mechanical forces of the eyelids against the globe.
Unfortunately, findings of lid wiper epitheliopathy may not be seen with sodium fluorescein, as the condition has no correlation to tear break-up time or Schirmer testing.3 Therefore, instillation of lissamine green staining is essential in those patients who are symptomatic but showing no signs of dryness.3
These patients may benefit from lid exfoliation with lid scrubs, as well as tear supplementation therapy to decrease friction. In addition, switching soft contact lens materials or adding coatings to rigid lenses may help to alleviate these signs and symptoms.
 |
| Staining shows lid wiper epitheliopathy present on the upper eyelid. |
Ocular Rosacea
Whether present with a diagnosis of systemic rosacea or not, underlying inflammation due to ocular rosacea can cause a patient to have discomfort and irritation.10 Telangiectatic vasculature present on the eyelid margins is pathognomonic for the condition, but can also be present alongside blepharitis, keratitis or conjunctivitis.10 This condition most commonly manifests between the ages of 40 to 60 and can have significant detrimental effects on ocular comfort and productivity.10 Targeted therapies toward eliminating or decreasing the inflammation, such as with low-dose oral doxycycline, is necessary in these cases.
Trauma
Lid anatomy can vary widely after trauma, which includes surgical interventions. For example, after correction of an entropion or ectropion, removal of lid lesions or with blepharoplasties, normal eyelid architecture may be compromised. This in turn can impact the apposition of the eyelid to the globe, disrupt the correct placement of the meibum component into the tear film, as well as the anatomy of the glands themselves.
Careful case history and communication with other eye care providers will assist in determining if trauma or surgery may be confounding factors in a patient’s dry eye symptoms.
Contact Lens Discomfort
Although all of the above lid findings can be noted in any patient, patients who wear contact lenses require an especially careful assessment, as these findings may be the determining factor between whether a patient is successful or discontinues lens wear. Forty-one percent of patients drop out of contact lenses due to visual complaints, and 36% due to ocular discomfort, with both of these complaints potentially being secondary to dryness.9 However, most sources report that up to half of all contact lens wearers have some discomfort.4 Materials and coatings can influence comfort, but lens wear itself also has effects on the ocular surface and adnexa.4 The palpebral conjunctiva, which directly abuts a contact lens, has been found to yield more prominent lid wiper epitheliopathy, especially in lenses with low lubricity.4
While more studies are necessary, current research also indicates that contact lens wear can cause dilation and inflammation of the meibomian glands, as well as partial or complete loss, with contact lens wearers having gland length that is half of that observed in non-contact lens wearers.4 These effects were noted in both rigid and soft lenses, with more gland dropout occurring in the upper and lower eyelids, respectively.4 In addition, wearers have more microbes colonized on their lid margins, foaming of the inferior lid margin and decreased blink rate compared with non-contact lens wearers.4 Therefore, as these patients are more prone to having pertinent eyelid findings, take extra care to enhance lubrication and overall comfort with the proper recommendations.
Regardless of whether a patient wears contact lenses, prescribed home therapies can significantly help to treat dry eye. However, it is also essential to consider in-office therapies as an adjunct in cases where patients are still symptomatic. The variety of these in-office procedures have expanded significantly, and options for patients range from relatively simple to more complex involving purchased equipment in your office.
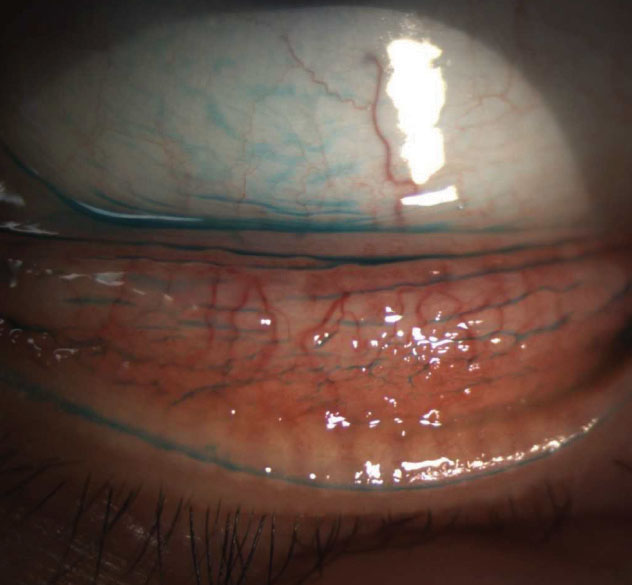 |
This patient displays moderate papillary reaction with lid wiper epitheliopathy on the lower eyelid. |
In-office Procedures
Optometrists have a number of potential interventions to consider and offer in their practices:
Gland expression. With the use of in-office warm compresses, and the high magnification achieved with biomicroscopy, a practitioner is able to express the meibomian glands manually or with the use of expressor paddles. With this technique, you can not only assess the quality and consistency of the meibum expressed but also encourage healthy expression once the patient is out of the office. Meibomian gland probing has also recently gained popularity due to case reports showing regrowth and restoration of atrophied glands.6
Lid debridement/Blephex (Blephex). Running a spud along the meibomian gland orifices to remove keratinization, as well as assist in exfoliation the eyelids, can eliminate capped glands, lid wiper epitheliopathy and promote healthy expression of meibum afterwards.
Another option is the Blephex procedure, which involves a rotating sponge that the practitioner uses to clean and exfoliate the eyelid margins. The process takes approximately seven minutes and is performed on each individual eyelid. Results are optimal if the procedure is repeated every four to six months.
Lipiflow/Mibo Thermoflo (Mibo Medical). These systems are a way of adapting a common home therapy (warm compresses) into a pulse-dosed in-office therapy. Both involve heating of the eyelids with concurrent massage. The procedures differ in that the Mibo Thermoflo involves a probe operated by a technician or doctor on the outside of the lids whereas Lipiflow is an automated system with an applicator that provides massage of the lids both on the underside and outside. Research shows these procedures are about equal in efficacy in improving signs and symptoms compared to three months of twice daily home warm compresses.11
iLux (Alcon). This handheld device uses light-based technology to heat the meibum from the inner and outer portions of the eyelids, allowing for expression of the glands, all under high magnification. This therapy allows manual gland expression outside of the slit lamp and provides specific measurements regarding length of treatment as well as the actual temperature when performing meibum expression.
Bandage contact lenses/scleral lenses. Depending on the severity of the ocular surface disease, bandage contact lenses and scleral lenses can be useful for patients who are unsuccessful with other therapies. By providing a mechanical barrier from the eyelids and environmental conditions, contact lenses can be extremely useful not only to provide symptomatic relief for patients, but also to protect and promote healing of the cornea and ocular tissues.
Although many patients may present with similar symptoms of dryness, burning or ocular irritation, it is important to evaluate the lids for clues. Many eyelid findings will direct you to very specific treatments targeting the underlying etiologies, in cases where typical artificial tear supplementation may have been unsuccessful.
There are many options for us to consider for our dry eye patients with lid disease. From improvements in lid hygiene to medical management ranging from ocular lubricants to steroid therapy, careful observation and examination may allow you to discover the targeted therapy necessary to finally be able to help these patients achieve the relief they are looking for.
Dr. Morrow is an assistant clinical professor at the State University of New York College of Optometry.
1. Blackie C, Korb D. A Novel Lid Seal Evaluation: The Korb-Blackie light test. Eye Contact Lens. 2015 Mar;41(2):98-100. 2. Craig J, NicholsK, Akpek E, et al. TFOS DEWS II definition and classification report. Ocul Surf. 2017 Jul;15(3):276-83. 3. Efron N, Brennan N, Morgan P, Wilson T. Lid wiper epitheliopathy. Prog Retin Eye Res. 2016;53(7):140-74. 4. Efron N, Jones L, Bron A, et al. The TFOS international workshop on contact lens discomfort: report of the contact lens interactions with the ocular surface and adnexa subcommittee. IOVS. 2013;54(10):98-122. 5. Gupta P, Stevens M, Kashyap N, Priestley Y. Prevalence of meibomian gland atrophy in a pediatric population. Cornea. 2018;37(4):426-30. 6. Hillman L. Research finds meibomian gland growth after probing technique. Eyeworld. www.eyeworld.org/research-finds-meibomian-gland-growth-after-probing-technique. October, 2017. Accessed December 15, 2018. 7. Koo H, Kim T, Kim K, et al. Ocular surface discomfort and Demodex: effect of tea tree oil eyelid scrub in Demodex blepharitis. Journal of Korean Medical Science. 2012;(27):1574-79. 8. Sridharan K, Sivaramakrishnan G. Therapies for meibomian gland dysfunction: a systematic review and meta-analysis of randomized clinical trials. Open Ophthalmol. 2017;11:346-54. 9. Sulley, A., Young, G., Hunt, C. Factors in the Success of New Contact Lens Wearers. Contact Lens and Anterior Eye. 2017; 40:15-24. 10. Wladis E, Adam A. Treatment of ocular rosacea. Surv Ophthalmol. 2018;63(3):340-6. 11. Zhao Y, Veerappan A, Yeo S, et al. Clinical trial of thermal pulsation (Lipiflow) in meibomian gland dysfunction with pretreatment meibography. Eye Contact Lens. 2016;42(6):339-46. |

