 |
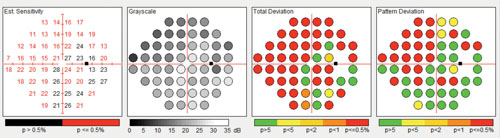
| This patient's glaucoma was largely under control until her mental status began to decline. Around that time, her visual fields showed an arcuate scotoma and nasal step in the right eye. |
Patient History
When I first saw her as a new patient in 2006, she presented with complaints solely related to vision. Her systemic medications included Lipitor (atorvastatin, Pfizer), Fosamax (alendronate, Merck), lisinopril, metoprolol and metformin. She was under treatment for diabetes mellitus type 2, which had been diagnosed four years earlier.
At this first visit, her best-corrected visual acuity was 20/20 OD and OS through hyperopic, astigmatic correction. Pupils were equal, round and reactive to light and accommodation, with no afferent defect. Slit lamp examination of her anterior segments was unremarkable. Intraocular pressure measured 26mm Hg OD and 14mm Hg OS. Central corneal thickness readings were 521μm OD and 498μm OS.
Upon dilation, examination revealed exfoliation syndrome in the right eye, with the appearance of characteristic exfoliative material in the anterior lens capsule. Close scrutiny of the anterior segment OD (and OS) revealed no other discernable deposition of this material, in particular along the papillary margin or in the angles. The left eye showed no evidence of exfoliation. Also, her crystalline lenses had minimal age-appropriate nuclear sclerosis, which did not interfere with vision.
Cup-to-disc ratios were 0.40 x 0.40 OD and 0.15 x 0.15 OS; there was no notching or thinning of the right neuroretinal rim that would indicate glaucomatous damage. The retinal vasculature showed mild hypertensive and arteriosclerotic retinopathy OU, which was consistent with her systemic health history. There was no evidence of diabetic retinopathy OU.
Diagnosis
She returned one month later for a complete glaucoma workup. IOP measured 25mm Hg OD and 17mm Hg OS. Standard automated perimetry testing was normal in both eyes. Gonioscopy showed 4+ open angles with minimal trabecular pigmentation OU and no evidence of exfoliative material in the angles. Optic nerve imaging correlated well with the clinical examination of the optic nerve head, as well as the general robustness of the neuroretinal rims OU.
Given the clinical presentation, I diagnosed the patient with exfoliative glaucoma OD and suspicion of glaucoma OS, and prescribed Travatan (travoprost, Alcon) HS OD.
The patient responded nicely to therapy, with post-treatment IOP generally ranging between 15mm Hg and 18mm Hg OD. Visual fields and HRT-III (Heidelberg Engineering) imaging of the optic nerves remained stable.
However, her IOP eventually began to increase. In 2010, I added Alphagan P (brimonidine tartrate, Allergan) to the right eye on a QAM basis. But by 2011, her IOP was steadily rising again, so I increased the Alphagan P to BID OD. Other than gradually increased IOP in the right eye, the neuroretinal rim appearance and SAP field studies had remained stable. Throughout this time, the left eye remained unchanged and exhibited no evidence of conversion to glaucoma.
In 2012, we obtained her first Heidelberg Edge Perimeter Flicker-Defined Form (HEP FDF) visual fields, which showed no significant field defects in either eye.
Medication Compliance
Sometime during 2012, I began to notice changes to the patient’s affect. All her visits with me had been friendly, cordial and quite interactive. But a subtle change was occurring. Although still smiling and friendly, she left me with the distinct impression that she either no longer fully understood or had lost interest with what was happening with her eyes (and why we were seeing her three times a year).
Furthermore, my ophthalmic technician had made several notes questioning her compliance with the drops; at the completion of each visit, we had to go over very explicit instructions for her medication use (which had continued with Travatan HS OD and Alphagan P BID OD).
By early 2013, her IOP OD was on the rise again, which further concerned me that she was failing to comply with her medication regimen. Also at this time, we noticed slight changes consistent with progression in the neuroretinal rim OD. Visual field testing with HEP FDF confirmed these changes, showing a well-developed arcuate scotoma and nasal step OD. Meanwhile in the left eye, the IOP, fields and neuroretinal rim continued to remained stable.
Once again, we stressed compliance with the medication regimen––but I was doubtful that she would be able to continue without laser intervention. I planned on one more follow-up visit to firm up the need for laser trabeculoplasty in the right eye. Unfortunately, she missed the next several visits due to other health concerns and to issues that I believed were related to her worsening mental status.
When she ultimately returned in October 2013, she’d had an obvious decline in her mental ability. Her historical skills had deteriorated to the point that we were unable to determine her compliance with her medications. Although she was able to carry on a reasonable conversation, she was simply no longer the person whom I met just a few years ago.
She complained of gradually decreasing vision that corresponded to her slowly progressing cataracts, yet she also reported that she was able to drive. By this time, IOP in the right eye had risen to the mid-20s, and the neuroretinal rim and FDF fields showed continued progression.
We were now officially at the point where surgical intervention was necessary.
Surgical Treatment
While laser trabeculoplasty OD was an option, I did not foresee that it would give us a long-term and hopefully medication-free solution to the problem. So, in early December 2013, the patient had combined cataract surgery and trabeculectomy with MMC in the right eye. In January 2014, she underwent lens extraction and IOL implantation in the left eye.
Postoperatively, both eyes are doing remarkably well. Although her post-op medication regimen was a challenge, we were able to enlist the help of her friends and neighbors to facilitate compliance, as she has no family nearby.
At her most recent visit in March 2014, her unmedicated IOP was 14mm Hg OD and 21mm Hg OS. Field testing and HRT-III imaging showed stabilization of the visual field and neuroretinal rim loss. She appears to be fine now (her eyes, at least), and she will likely continue to do well as the bleb is well formed and not inflamed.
Discussion
Even on a good day, with a fully cognizant patient, compliance with glaucoma medications can be a challenge. Add to the picture a patient who is getting older and perhaps more forgetful, and a disease that’s highly demanding in its need for control, and you have the perfect setup for a tenuous situation to go bad or get even worse.
What can we do about such a situation? Do we need to move toward surgical intervention sooner in such a case than we usually would? How do we really judge unwillingness to comply against inability to comply, and how do we recognize that?
I don’t propose to have the answers. But, having seen this patient for as long as I have, and having gotten to know her, my hunch that she was undergoing a decline in her mental status turned out to be true. Should I have moved her to laser therapy sooner? Perhaps. But, the counter-argument is that everything was going well at that time, so why alter therapy that was working?
The take-home message is, perhaps, that not only do we need to be focused clearly on the status of the neuroretinal rim and visual fields in glaucoma patients, but we also need to be more attentive to the patient’s affect, mood and demeanor––as these may be clues to some neurodegeneration elsewhere than the optic nerve.

