 |
An 86-year-old Hispanic male with a history of wet age-related macular degeneration in both eyes presented with a chief complaint of painless, progressive vision loss in both eyes. He received multiple intravitreal Avastin injections, most recently three months prior in the left eye.
His past ocular history was significant for a recent intraocular lens exchange and anterior vitrectomy in the left eye.
His ocular medications included prednisolone acetate in the left eye four times a day, as well as Timolol twice a day in the left eye due to a history of ocular hypertension from steroid response. He admitted to very poor compliance with both of his topical ophthalmic medications.
His medical history was significant for multiple systemic pathologies, including benign prostatic hyperplasia, arthritis, hypertension, osteoporosis and a pacemaker. His systemic medication list was extensive, although none with known significant ocular side effects.
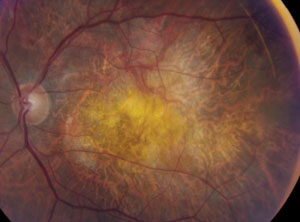 | |
| Fig. 1. This fundus photo shows the left eye of an 86-year-old presenting with painless, progressive vision loss. Can you identify the cause? |
Upon examination, his distance BCVA was 20/60+ in the right eye and counting fingers at one foot in the left eye. His intraocular pressure was 18mm Hg in the right eye and 31mm Hg in the left eye. The slit lamp examination of his right eye revealed a posterior chamber intraocular lens, geographic atrophy without obvious fluid or heme in the macula, and old laser scars around a horseshoe tear in the peripheral retina. The slit lamp examination of his left eye revealed an anterior chamber intraocular lens with a patent peripheral iridotomy and superior corneal sutures intact. The anterior chamber of his left eye revealed 1+ cell. Fundus findings of the left eye are represented in figure 1. Heidelberg SD-OCT images of his left eye are available for review in figures 2 and 3.
Take The Retina Quiz
1. What is the likely cause for vision loss in this patient’s left eye?
a. High IOP causing glaucomatous damage from chronic steroid response.
b. Inflammation from recent IOL exchange.
c. Fibrosis and geographic atrophy from age-related macular degeneration.
d. All of the above.
2. What finding is represented by the arrows in figure 2 and 3?
a. Irvine-Gass macular edema.
b. Outer retinal tubulation.
c. Cystoid macular edema.
d. Subretinal fluid.
3. What other diagnostic test would be helpful in determining the etiology of the findings in figures 2 and 3?
a. B-scan echography.
b. Fundus autofluorescence.
c. Fluorescein angiography.
d. Time-domain ocular coherence tomography.
4. What is the appropriate treatment for the findings highlighted in figures 2 and 3?
a. Anti-VEGF injection.
b. Focal laser photocoagulation.
c. Combination of topical NSAID and steroid.
d. Observation.
For answers, see below.
Diagnosis
The structures denoted with arrows on the SD-OCT (figures 2 and 3) represent outer retinal tubules. Thanks to the precision of SD-OCT, investigators in 2009 detected a “peculiar” change in the outer retina in their study of 63 patients with advanced retinal disease.1 They described round or ovoid spaces with a hyporeflective center and hyperreflective border within the outer nuclear layer that simulated the appearance of cystoid macular edema or subretinal fluid on isolated scans. The study also made use of SD-OCT C-scans to allow en face visualization of the outer retina, which showed that these spaces often continued linearly throughout the outer nuclear layer in branching tubular structures. They determined these changes represented “outer retinal tubulation.”
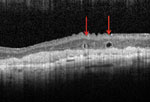 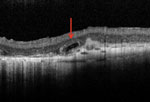 | |
| Figs. 2. and 3. Can you identify what the red arrows are pointing to in this patient’s Heidelberg SD-OCT images? |
Outer retinal tubules are commonly seen in advanced AMD patients. In the CATT study, outer retinal tubules were present in 10.1% of AMD patients at 56 weeks after initial treatment with anti-VEGF and 17.4% at 104 weeks after treatment.2
In patients with geographic atrophy, outer retinal tubules may be present in 21% to 26% of patients.3 Outer retinal tubules can also be found in other advanced retinal diseases such as associated CNVM and subretinal fibrosis, pattern dystrophy, AZOOR, multifocal choroiditis, pseudoxanthoma elasticum, Stargardt disease, gyrate atrophy, choroideremia, chronic central serous chorioretinopathy, retinitis pigmentosa, cone dystrophy and Bietti crystalline dystrophy.
Interestingly, Christine Curcio and colleagues first described outer retinal tubules in a histopathologic study of AMD in 1996.4 They found that surviving photoreceptors in advanced AMD had an apparent reorganization into interconnecting tubes over areas of scarring. However, it was not until the advent and common clinical use of SD-OCT that a clearer understanding of outer retinal tubules was realized.
Initial studies postulated the process of outer retinal tubulation likely begins with sublethal injury of photoreceptors leading to invagination of the photoreceptor layer until opposing ends establish connections and form tubular structures.
Another study compared the appearance of outer retinal tubulation in patients with advanced AMD on SD-OCT to their actual histology in post-mortem retinal tubule specimens, allowing researchers to definitively correspond OCT appearance to anatomical composition.5 That team determined the defining features of outer retinal tubulation on histology as a circular or ovoid external limiting membrane border made by Müller cell processes with radially oriented photoreceptors in four phases of degeneration, ranging from both outer and inner segments to minimal or no photoreceptor segments.
Beyond the clinical appearance, they also determined the location of the outer retinal tubulation to be in the outer nuclear layer with a hyperreflective band in either a closed or open configuration, with often overlying dysmorphic or absent retinal pigment epithelium. These defining features help differentiate these lesions from cystoid macular edema, which is more commonly found in the outer plexiform and inner nuclear layer and does not have a hyperreflective border on SD-OCT.
It is easy to confuse the clinical appearance of outer retinal tubules and cystoid macular edema. It is clinically important to make the distinction because improper diagnosis may prompt physicians to unnecessarily treat with anti-VEGF injections or focal laser photocoagulation when no actual fluid is present. In fact, outer retinal tubules are relatively refractory to treatment and the mere presence suggests the disease is end-stage and relatively quiescent and therefore this finding alone shouldn’t prompt intervention.
Our patient was treated with an intravitreal Avastin injection in the left eye solely due to his preference for a treat-and-extends approach, as his fundus exam and SD-OCT did not reveal any intra-retinal fluid. He was also counseled extensively on the importance of compliance with his topical ocular medications, and was told to resume Prednisolone Acetate in the left eye with a weekly taper, and well as Timolol twice a day in the left eye.
The presence of outer retinal tubulation on the SD-OCT images of this patient’s left eye likely indicates quiescent and end-stage age-related macular degeneration.
This case was written and provided by Savannah Brunt, OD, ocular disease resident at Bascom Palmer Eye Institute.
1. Zweifel S, Engelbert M, Laud K, et al. Outer retinal tubulation. Arch Ophthalmol. 2009;127(12):1596-602.2. Lee J, Folgar F, Maguire M, et al. Outer retinal tubulation in comparison of age-related macular degeneration treatment trials (CATT). Ophthalmology. 2014;121:2423-31.
3. Hariri A, Nittala M, Sadda S, et al. Outer retinal tubulation as a predictor of the enlargement amount of geographic atrophy in age-related macular degeneration. Ophthalmology. 2015;122:407-13.
4. Curcio C, Medeiros N, Millican C. Photoreceptor loss in age-related macular degeneration. Invest Ophthalmol Vis Sci. 1996;37(7):1236-49
5. Schaal K, Freund K, Litts K, et al. Outer retinal tubulation in advanced age-related macular degeneration: Optical Coherence Tomographic Findings Correspond to Histology. Retina. 2015 Jan. [Epub ahead of print]. Accessed: March 17, 2015.
Retina Quiz Answers:
1) c; 2) b; 3) c; 4) d.

