 |
Each year, nearly 800,000 people in the United States suffer a stroke, and one American dies from a stroke every four minutes, on average.1 A stroke is an acute loss of neurological function due to an abnormal perfusion of brain tissue. A stroke occurs when the blood supply to part of the brain is interrupted or severely reduced, depriving brain tissue of oxygen and nutrients. Within minutes of the blood flow interruption, brain cells begin to die. Also called cerebrovascular accident (CVA), stroke is a medical emergency.
Symptoms of stroke may include sudden loss of speech, dizziness, confusion, weakness or paralysis of one side of the body, headache and seizure. Common ocular symptoms in stroke patients may include blur, visual field loss and diplopia. Prompt treatment is crucial, as early action can minimize brain damage and potential complications.
Stroke patients are at significantly high risk for another event. One of every four survivors has another stroke within five years.1,2
Types of Stroke
There are three categories of stroke:
Ischemic Stroke. Most strokes (85%) are ischemic and commonly result from an arterial obstruction by a thrombus or embolus.2
 | |
| Retinal emboli increase the risk of stroke-related death. |
Hemorrhagic Stroke. A hemorrhagic stroke occurs when a blood vessel in the brain leaks or ruptures. The hemorrhage applies pressure to brain cells and causes damage. These leaks or ruptures occur either within the primary brain tissue or in the subarachnoid space.
Transient Ischemic Attack (TIA). A TIA is also known as a “mini-stroke.” It is different from the ischemic and hemorrhagic types in that blood flow to the brain is blocked for only a short time—usually no more than five minutes.
As a warning sign of an impending ischemic or hemorrhagic cerebrovascular event, TIA is considered a medical emergency. More than a third of those who have a TIA end up having a major stroke within one year if they don’t receive treatment, and 10% to 15% will have a major stroke within three months of the TIA.1,2 Recognizing and promptly treating TIAs can reduce the risk of a major stroke and severe disability.
Ocular Signs and Symptoms
As many as 75% of those who sustain a stroke also experience one or more TIAs in the preceding days to months, and some of these initial events involve visual symptoms and signs.2 Symptoms are similar, though more pronounced, in ischemia and hemorrhagic stroke. A patient experiencing a TIA may have monocular vision loss—known as amaurosis fugax, Greek for “fleeting blindness”—that occurs rapidly and resolves in a few minutes.
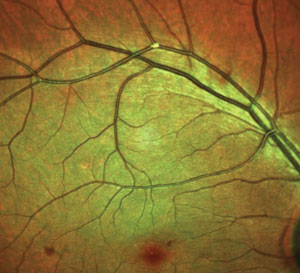
Retinal emboli also may be a premonitory sign of cerebral stroke.3 Cholesterol emboli originate from plaques in the carotid artery or occasionally the aortic arch. Calcific emboli usually arise from the heart or the great vessels. Platelet-fibrin emboli can occur from the heart or blood vessels. Retinal emboli are associated with an increased incidence of vascular disease and stroke-related death.3
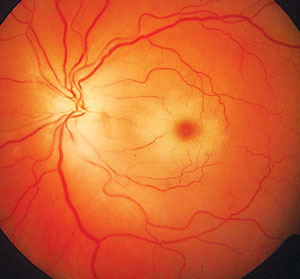 | |
| A central retinal arterial occlusion (CRAO) may result from an embolus or atherosclerotic changes. Similarly, ischemic stroke often results from an arterial obstruction by a thrombus or embolus. |
Bilateral transient monocular vision loss (TMVL) may result from vertebrobasilar insufficiency to the brain’s posterior aspect. Other possible ocular manifestations of stroke include diplopia (cranial nerve involvement) and homonymous field loss. Stroke patients are more likely to develop ocular ischemic syndrome, retinal arterial occlusions and anterior ischemic optic neuropathy.3
FAST Intervention
Acting FAST can help stroke patients get the urgent treatment they desperately need. The most effective treatments are only available if the stroke is diagnosed within three hours of the first symptoms. Stroke patients may not be eligible for the most effective treatments if they don’t arrive at the hospital in time.
If you think someone may be having a stroke, perform the following simple tests:3-5
Face: Ask the person to smile. Does one side of the face droop?
Arms: Ask the person to raise both arms. Does one arm drift downward?
Speech: Ask the person to repeat a simple phrase. Is his or her speech slurred or strange?
Time: If you observe any of these signs, call 9-1-1 immediately. Note the time symptoms first appear. Call an ambulance so that medical personnel can begin life-saving treatment on the way to the emergency room.
Treatment
If a patient gets to the hospital within three hours of the first symptoms of an ischemic stroke, the health care team may administer a thrombolytic (or clot-busting) drug. Tissue plasminogen activator (tPA) is an example of such an agent that improves the chance of recovery. Several studies show that ischemic stroke patients who received tPA are more likely to fully recover or have less disability than those who do not receive the drug.6,7 In addition, patients treated with tPA are less likely to need ongoing care in a long-term health facility.6,7
In hemorrhagic stroke, basic life support, as well as controlling bleeding, seizures, blood pressure (BP) and intracranial pressure (ICP), are critical. Medications, surgery or endovascular procedures may be necessary to stop the bleeding and save brain tissue.
Risk Factors for Stroke1,4,5,8
|
Medications. Classes of medications used in the treatment of acute hemorrhagic stroke include anticonvulsants (to prevent seizure recurrence), antihypertensive agents (to reduce BP and other risk factors of heart disease) and osmotic diuretics (to decrease ICP in the subarachnoid space).8,9
Endovascular procedures. These procedures are less invasive and less risky for the patient than surgical treatments. A long tube is inserted through a major artery in the leg or arm and then guided to the site of the weak spot or break in a blood vessel. The tube is then used to install a device to repair the damage or prevent bleeding.8,9
Surgery. Hemorrhagic strokes may be treated surgically. If the bleeding is caused by a ruptured aneurysm, a metal clip may be put in place to stop blood loss.8,9
Optometrists encounter patients at risk for stroke every day. We must acquaint ourselves with the first symptoms and signs, including ocular complications. Our next column will address optometry’s role in post-stroke care.
1. Centers for Disease Control and Prevention. Stroke Facts. Accessed June 5, 2015. www.cdc.gov/stroke/facts.htm.2. Mozzafarian D, Benjamin EJ, Go AS, et al. Heart disease and stroke statistics—2015 update: a report from the American Heart Association. Circulation. 2015:e29–322.
3. Purvin V. Cerebrovascular disease and the visual system. Ophthalmol Clin N Am. 2004;17:329-55.
4. Lambert M. Practice Guidelines: AHA/ASA guidelines on prevention of recurrent stroke. Am Fam Physician. 2011;83(8):993–1001.
5. National Institute of Neurological Disorders and Stroke. Brain Basics: Preventing Stroke. Accessed December 4, 2013.
6. National Institute of Neurological Disorders and Stroke rt-PA Stroke Study Group. Tissue plasminogen activator for acute ischemic stroke. N Engl J Med. 1995;333:1581–7.
7. Marler JR, Tilley BC, Lu M, et al. Early stroke treatment associated with better stroke outcome: the NINDS rt-PA stroke study. Neurology. 2000;55:1649–55.
8. National Institute of Neurological Disorders and Stroke. Stroke: Challenges, Progress, and Promise. Bethesda, MD: National Institutes of Health; 2009.
9. American Heart Association/American Stroke Association. Stroke Treatments. 2013.

