Maintaining a patient’s contact lens comfort and lens wear success often comes down to one invaluable element: patient education. Imparting the knowledge a patient needs to ensure proper contact lens replacement and care is integral to maintaining comfort. However, it’s not always easy to cover all the contingencies in the initial patient encounter, and practitioners must be careful not to take anything for granted. For instance, a contact lens patient recently presented to my office with an emergency exam for bilateral chemical burns from using a store-bought eyeglass cleaner to store her contacts overnight.
Patients, especially those new to contact lenses, require repeated step-by-step instructions to retain the basics of contact lens care and develop an understanding of how real-world factors such as routine care, allergies, injuries and even their occupations can impact contact lens comfort.
 | |
| Using the Korb-Blackie light test, the examiner places the transilluminator at the lid crease and then evaluates the lash margin, looking for light to spill out, indicating inadequate lid closure. Photo: Caroline Blackie, OD. |
Discomfort should not be an acceptable reason for contact lens dropout—it is an eminently correctable problem when it does occur, and careful attention to patient education, particularly at the initial encounter, can help avoid it in the first place. This article focuses on patient education for contact lens wearers, and how doctors and patients alike can maintain an awareness of potential causes for discomfort before complaints arise.
Pre-fitting Evaluation
Ocular surface symptoms, namely dryness and discomfort, are the leading causes of contact lens drop out for both soft and rigid lenses.1 Contact lens patients are 50% more likely to experience these symptoms than those who do not wear contacts.2 You may be able to prevent this discomfort before it starts by first evaluating the ocular surface health of all your patients before fitting them with contact lenses.
Investigators estimate that 10% of patients will discontinue contact lens wear.3,4 Developing a protocol for evaluating all contact lens patients, new and long-time wearers alike, is the first step to reducing these rates. This protocol should include:
- A dry eye questionnaire, such as the SPEED or OSDI—both validated questionnaires. These can help identify patients with ocular discomfort before initiating contact lens wear.
- Obtaining a comprehensive history, including daily wear time, digital device use, cleaning habits, lens replacement schedule and hobbies—even occupation and social history. These are important factors to consider for long-term lens comfort.
- A clinical evaluation, including vital dye staining to test for lid wiper epitheliopathy (LWE) as well as corneal/conjunctival staining indicative of dry eye disease.
- An osmolaritiy test.
- Testing for matrix metalloproteinase 9.
- Lid and meibomian gland evaluation.
- Lash evaluation.
These tests are designed to help identify common causes for dry eye, non-obvious meibomian gland dysfunction (MGD), Demodex infestation, blepharitis, lid wiper epilethiopathy (LWE) and lid-parallel conjunctival folds, as well as aqueous deficient dry eye.
To institute this protocol start by educating your staff about risks associated with contact lenses and the need to treat any pre-existing ocular conditions before dispensing the lenses.
 | |
| Patients often apply make-up directly to the meibomian gland orifices. However, even when applied properly, make-up debris can migrate to the lid, conjunctiva and even deposit on contact lenses, ultimately leading to discomfort. |
Also, be sure to update the protocol, as investigators learn more regarding knowledge of the underlying causes of contact lens discomfort.
Likely Discomfort Causes
Research shows contact lens patients have a higher incidence of dryness and end-of-day irritation than non-contact-lens-wearing patients.5 These complaints may or may not be part of a prior dry eye condition. For patients who did not experience any pre-existing symptoms or display any signs of dry eye prior to fitting, we must search for other causes. In some cases, contact lens materials or cleaning solutions may play a role.6
To determine the cause of this discomfort, develop a treatment plan and decrease our rate of contact lens discontinuation, doctors must put on their sleuthing hats. Start by listening to patients’ complaints, with an acute awareness of dry eye triggers.
Therapeutic Factors
The history for a contact lens patient should include a comprehensive list of medications. Many medications can cause ocular surface dryness. The prime culprits include antihistamines, blood pressure medications, oral contraceptives, antidepressants and cholesterol-lowering medications.7-9
Non-prescribing physicians should not discontinue medications; however, alternative choices are often available with a lower risk of ocular side effects from dryness. Keeping the line of communication open between the primary care providers, OB-GYN, allergists and immunologists, rheumatologists and cardiologists can create a more comprehensive treatment approach.
Lifestyle
In addition to a dry eye questionnaire, it is also helpful to add a few key questions before your exam. Questions may include: ‘How do your eyes feel upon awakening?’ or ‘Do you have fluctuations in your vision throughout the day, with reading for any length of time or when using a computer?’ A patient with complaints upon waking in the morning should be evaluated for inadequate lid seal, corneal conditions such as recurrent corneal erosions and even Demodex blepharitis. Fluctuations in vision throughout the day is a common symptoms for underlying ocular surface dryness.
Ask the Right Questions
|
Asking patients about their hobbies can clue you in to the potential for environmental hazards that can lead to CL discontinuation. Take a soccer mom for example: exposure to wind and dust while watching kids’ sporting events can dry out lenses and lead to foreign body sensation. Many of our patients are active in exercise, biking, running and swimming. Exposure to sand, sweat, water and suntan lotion can also complicate contact lens routines. Riding in a car with either the heat or air conditioning on, or even with the windows down, can also cause discomfort due to evaporative stress to the ocular surface and tear film.
We are also a nation obsessed with appearance and youthful skin. Ask patients what, if any, skin creams they are applying around the eye. Retinol has been found to damage meibomian glands leading to dry eye symptoms.10 This is present in many OTC and high-end face and eye creams. Eye make-up is another area of concern. Mascara, eyeliners and eye shadows are commonly applied to the lid and sometimes even to the meibomian gland orifices. These contain pigments and talcs that can block the glands and irritate the ocular surface, not to mention deposit on the contact lenses themselves.
Eyelash growth products like Latisse, eyelash extensions and false eyelashes give the appearance of extended lashes. However, these products also can lead to ocular surface discomfort and possibly contact lens discontinuation.
Occupational Hazards
One issue to consider when evaluating patients with contact lens discomfort is the patient’s job. Some occupations, like those that predispose one to reduced or incomplete blinking, are notorious for the negative impact they can have on contact lens comfort. Spending hours using a computer increases the risk for end-of-day dryness. And one group of professionals you might overlook are staring at you each morning in the mirror and the office—health care workers.
Doctors in most any setting, ranging from routine care to surgical, are a group at risk for MGD. The more concentrated someone is on a task, the less likely they are to blink, resulting in evaporative stress to the ocular surface.11 Advise patients to take breaks from screen time and follow the “20/20 rule”; that is, for every 20 minutes of computer use, take a 20-second break. Also, start introducing the idea of blink exercises for patients who spend a lot of time in front of computers and have impartial blinks. Instruct the patient to take 10 consecutive, thoughtful blinks, holding each for two seconds.
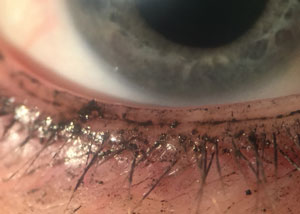
 | |
| Cylindrical debris around lashes, as seen here, is a hallmark of Demodex blepharitis. |
Air quality also has an impact on comfort. Pilots and flight attendants work in low humidity environments. Construction workers and military personnel are often exposed to large amounts of dust and dirt from their environments.
Another group of patients that might have higher risk of contact lens discontinuation is first responders (e.g., firefighters, EMTs, military personnel and police). These professionals may have to spring into action and feel they cannot be bothered to remove and insert contact lenses. In my practice, I’ve seen these patients sleep in their lenses frequently for the convenience of being able to see immediately when they awake.
Allergies
Recurring discomfort problems for contact lens wearers can stem from allergies and increased pollen counts.
In my experience, patients blame much of their contact lens discomfort on allergies. But, a proper diagnosis requires more than a patient’s intuition.
Ruling allergies in or out can be a tremendous help in patient education and also determining a proper course of treatment. Fortunately, we now have in-office allergy tests (e.g., DoctoRx, new IgE tear analyses, TearScan) that can play a role.
Systemic Disease
Ask contact lens patients, “Do you struggle with dry mouth?” If a patient suffers from both dry eye and dry mouth symptoms, you may consider advising them to explore the potential influence of underlying autoimmune diseases, such as Sjögren’s syndrome or rheumatoid arthritis, as a possible cause for this combination of symptoms.
Treatments
Once the root cause of contact lens discomfort is identified, the next step is to develop a treatment plan that will help keep the patient satisfied with the prescribed lenses.
Maintaining Comfort
Treat the underlying condition(s) whenever possible. If aqueous deficient dry eye is present, Restasis is a often great option to maintain comfort in a lens. Remember that clinical improvement may be delayed (taking up to six months in some patients) and initial burning is an acceptable side of effect of treatment. Restasis should be used 10 minutes prior to lens insertion and again after the lens is removed at the end of the day. When MGD is present, treat it aggressively. Controlling any underlying dry eye will help improve comfort.
| Gadgets Galore New technology is making it easier than ever to identify dry eye patients. Tear osmolarity testing (TearLab) as well as a quick evaluation for inflammatory mediators (InflammaDry) can add diagnostic specificity to your exam. Measure the tear meniscus and tear break-up time (TBUT). The normal tear meniscus height is 0.34mm above the lower lid margin.1 TBUT is important at baseline evaluation, as soft contact lenses will dehydrate on most eyes with extended wear. This should be done using only a small quantity of fluorescein dye; the dry eye test strips are ideal. When applying, it is recommended to have the patient look down and inward, placing the strip on the superior-temporal bulbar conjunctiva. Using the slit lamp, have the patient blink a couple of times followed by a blink and hold, until the dye is breaking up on the ocular surface. 1. Bartlett JD, Jannus SD. Clinical Ocular Pharmacology. 5th ed. St. Louis: Butterworth Heinemann; 2008:415-35. |
Lens material, cleaning solutions and replacement schedules are modifiable and easy ways to improve patient comfort. Increasing replacement frequency improves the comfort of the lens. There are many daily lens options available with a wide variety of parameters to assure good comfort and good vision for patients. Preservative-free peroxide-based cleaning systems also improve comfort of the lens when dailies are not an option. This simple change to a daily routine can increase wear time and comfort with little effort on either the patient or doctor’s part.
Ask patients how they are washing their hands with before lens insertion. Patients who describe a strong urge to remove lenses at the end of the day and who gain little relief from rewetting drops should be counseled on the type of solution they are using as well as the type of soap to use when handling lenses. Glycerin soaps can be used to help prevent chemical build-up on the lens during instillation. Removing the lenses mid-day to soak and rehydrate in their case, as well as using artificial tears compatible with contact lenses, are also good management methods.
Talk to your patients about their make-up use and removal habits. I recommend avoidance of any waterproof mascara or liners, as they often contain pigments that make them more difficult to remove. Replacing eye make-up on the recommended three-month cycle will also help decrease the risk for bacterial overgrowth. Coconut oil can be used to remove make-up without the exposure to harsh chemicals.
Listening Can Build a Practice
Take the extra time with your patients to discuss the exam findings and the importance of compliance to your treatment plan. Educate all new contact lens patients—and, in the case of juveniles, their parents—about lens discomfort. Let them know that once discomfort begins, it’s time to call the office. The earlier we intervene, the better the end result. Educate patients about end-of-day dryness and recommend ways to keep ahead of this to retain contact lens wear late in the day.
Take the time to listen and work with patients to solve their discomfort issues. Not only will it aid you in creating customized solutions that will make a huge difference in their day-to-day life, it will help you develop a strong bond with your patient and give them a reason to refer their friends.
Ensuring comfortable contact lens wear has no “one-size-fits-all” approach. We must offer curated care that takes into consideration how individual patients behave in the real world. Collecting a variety of information during your encounter with the patient, from critical testing to anecdotal interactions, will help you develop a tailored education and treatment plan that will allow patients to remain comfortable long-term in their lenses.
Dr. O’Dell is an optometrist at the May Eye Care Center & Associates in Pennsylvania, and a member of the Pennsylvania Optometric Association and the American Optometric Association.
1. Richdale K, Sinnott LT, Skadahl E, Nichols JJ. Frequency of and factors associated with contact lens dissatisfaction and discontinuation. Cornea 2007;26:168-74.2. Chalmers RL, Begley CG. Dryness symptoms among an unselected clinical population with and without contact lens wear. Cont Lens Anterior Eye 2006;29:25-30.
3. Dumbleton K, Woods CA, Jones LW, Fonn D. The impact of contemporary contact lenses on contact lens discontinuation. Eye Contact Lens. 2013 Jan;39:93-99.
4. Pritchard N, Fonn D, Brazeau D. Discontinuation of contact lens wear: a survey. Int Contact Lens Clin. 1999 Nov;26(6):157-62.
5. Begley CG, Chalmers RL, Mitchell GL, et al. Characterization of ocular surface symptoms from optometric practices in North America. Cornea. 2001 Aug;20:610-8.
6. Young G, Chalmers R, Napier L, et al. Soft contact lens-related dryness with and without clinical signs. Optom Vis Sci. 2012 Aug;89:1125-32.
7. Bartlett JD. Ophthalmic toxicity by systemic drugs. In: GCY Chiou, ed. Ophthalmic Toxicology. 2nd ed. Michigan: Taylor and Francis, 1999:225-83.
8. Jaanus SD. Ocular side effects of selected systemic drugs. Optom Clin. 1992;2(4):73-96.
9. Jaanus SD, Bartlett JD, Hiett, JA. Ocular effects of systemic drugs. In: Bartlett JD & Jaanus SD (eds.). Clinical Ocular Pharmacology, 3rd ed. Boston: Butterworth-Heinemann, 1995:957- 1006.
10. Ding J, Kam W, Dieckow J, Sullivan D. The Influence of 13-cis Retinoic Acid on Human Meibomian Gland Epitheilial Cells. Invest Ophthalmol Vis Sci. 2013 Jun;54:4341–50.
11. Portello JK, Rosenfield M, Chu CA. Blink rate, incomplete blinks and computer vision syndrome. Optom Vis Sci. 2013 May;90(5):482-7.

