Cataract patients—and their need for care—are both on the rise, especially as the baby boomer generation approaches retirement age. The 2000 United States census data estimated that roughly 20.5 million Americans older than 40 years of age had a cataract. By 2020, that number is expected to rise 46.8%, to 30.1 million.1 Plus, the growing diversity and complexity of IOL options adds to the patient’s need for guidance, a task particularly well-suited to optometrists.
As primary eye care providers, we are often the first to recognize, diagnose and educate the patient regarding the presence of a cataract. Leading the comanagement effort for these patients is an essential part of our practice modality as well. We establish enduring relationships with our patients and become particularly acquainted with their medical and social histories.
Patients will look to us for guidance from the moment we inform them of the presence of a cataract to the final postoperative follow-up.
| Table 1. Ocular Examination of Cataract Patients2 | ||
| Minimal testing | Recommended ancillary testing | |
| Visual acuity Pupillary evaluation Ocular motility Visual field screening (confrontations, etc.) Refraction Intraocular pressure measurement Biomicroscopy (undilated and dilated) Fundus evaluation | Contrast sensitivity Glare testing Potential acuity testing | |
This article reviews the basic principles and protocols of caring for this perpetually expanding patient population.
Initial Evaluation
By age 60, most individuals develop some degree of cataract. Our role is to evaluate and diagnose visually significant cataracts and determine the most appropriate treatment plan. A comprehensive examination may include, but is not limited to, elements listed in Table 1.
Contrast sensitivity, a glare test or both may be of assistance in quantifying the functional disability that may be far worse than visual acuity measurements indicate.2
Potential acuity testing is valuable in determining how much the cataract is contributing to the patient’s visual loss. A poor best-corrected visual acuity and a poor potential acuity may reveal that the cataract may not be the sole culprit for the patient’s decreased vision and symptoms. Further investigation for other possible causes (e.g., retinal disease or amblyopia) is necessary.
Diagnosis
Cataracts are frequently graded by visual examination and then assigned numerical values to indicate severity. Alternate grading systems, such as the Lens Opacity Classification Systems (LOCS, LOCSII and LOCSII) use cross-sectional slit lamp photographs as references to aid in grading. The recently introduced LOCSIII system contains a sequence of six reference photos for three types of cataract.3 Due to the limited availability of reference photos in the everyday clinical setting, clinicians commonly use a modified four-point grading system derived from the LOCSII (Table 2).2-3
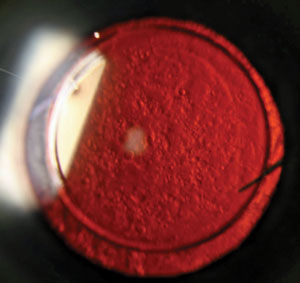 | |
| Typical posterior capsule opacity, a complication of cataract surgery, as seen with retroillumination. Photo: Aaron Bronner, OD. |
For finer incremental steps, clinicians can add a ‘+’ sign to designate any cataract that falls between grade levels.
Basis for Treatment
Not all visually significant cataracts require surgical treatment.2 Therefore, patients with cataracts can be divided into two groups: surgical and nonsurgical. The basis of treatment depends on the extent of the patient’s visual disability, symptoms and visual needs. Common symptoms of incipient cataracts include visual blur, reduced contrast sensitivity, perceived color changes and sensitivity to light, glare or both.
Non-surgical Patients
Some patients may appear to be developing cataracts, but are not yet candidates for surgery. The initial treatment for symptomatic cataracts may include updating a patient’s prescription (spectacles, contact lenses or both). Patients may also benefit from wearing a wide-brimmed hat and sunglasses with specific tints or filters to increase ultraviolet (UV) protection and reduce glare disability. Tints that selectively filter shorter wavelengths may increase image contrast by reducing light scattering and lens fluorescence. Pink, grey or green filters can decrease the amount of light entering the eye to improve light scatter. Other special lenses, such as the Corning CPF filter 511 and 527, may also help in contrast enhancement and glare reduction.5
In addition, advising these patients on appropriate illumination control and lighting sources for reading may give them the tools they need to improve their functional visual ability.2
Follow these patients at four- to 12-month intervals to determine whether further vision loss or functional disabilities develop. Such progression may require an updated refraction or consideration for cataract surgery at that time. To ensure patients are aware of their condition’s prognosis, it is helpful to educate them on the natural course of cataract formation, as well the signs and symptoms associated with progression. Proper patient education is necessary to ensure patients understand the limitations of corrective lenses, which can decrease chair time from refraction checks.
| Table 2. Grading of Three Common Types of Cataracts | |||||
| Cataract Type | Grade 1 | Grade 2 | Grade 3 | Grade 4 | |
| Nuclear | Mild | Moderate | Pronounced | Severe | |
| Cortical | Obscures 10% of intrapupillary space | Obscures 10% to 15% of intrapupillary space | Obscures 50% to 90% of intrapupillary space | Obscures more than 90% of intrapupillary space | |
| Posterior Subcapsular | Obscures 3% of the area of the posterior capsule | Obscures 30% of the area of the posterior capsule | Obscures 50% of the area of the posterior capsule | Obscures more than 50% of the area of the posterior capsule | |
Surgical Patients
Poor visual acuity testing results—or subjective interference in daily function—indicate that it is time for cataract surgery. It should be stressed that functional complaints of daily living are the most important criteria, more so than visual acuity. Ideally, a cataract is ready for surgery if it meets the “Goldilocks criteria,” meaning it has to be “just right.” Cataracts that cause almost no preoperative decline in visual acuity are at risk for worse postoperative visual acuity.6,7 Inversely, a hypermature cataract increases the risk of intraoperative complications.6,7
Today, the Goldilocks cataract is considered one that has reduced visual acuity to the level that it interferes with the patient’s lifestyle and everyday activities, and satisfactory functional vision cannot be obtained with spectacles, contact lenses or other optical aids.
The American Optometric Association (AOA) guidelines divide surgically indicated cataract patients into two groups:
(1) visual acuity of 20/40 or better
(2) visual acuity of 20/50 or worse
The American Academy of Ophthalmology (AAO) guidelines designate a patient as a surgical candidate when visual function no longer meets the patient’s needs.8 There is no specific acuity requirement. Eye care providers must pay extra attention to sort out the 20/40 vision or better surgically indicated group due to the less obvious visual acuity deterioration. These patients often have complaints of decreased vision during specific tasks, complaints of monocular diplopia, large refractive difference between the eyes or a combination of all three. All of these symptoms require further investigation to confirm that the cataract is the primary etiology for the complaints and whether surgery would be beneficial.
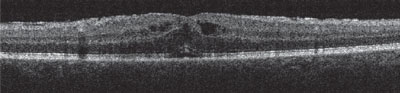 | |
| Postoperative CME appearing three weeks after surgery. Central macular thickness of 430µm. Patient had self discontinued topical steroid 10 days after surgery. Photo: Aaron Bronner, OD. |
Individuals with visually significant cataracts who elect to defer surgery should be advised of the dangers of reduced vision, including increased risk of falls and possibly decreased driving ability. If reduced vision is significant, patients should be educated on whether or not they meet their state’s legal requirements for driving. Low vision evaluation would be an option in cases where the cataract progresses but the patient continues to defer surgery or if surgery is not a viable option due to comorbidities.
Coexisting Conditions and Contraindications
As primary eye care providers, we become closely acquainted with our patients’ histories. It is our responsibility to remain attentive to any coexisting ocular conditions (e.g., dry eye, recurrent anterior uveitis, pseudoexfoliation syndrome, glaucoma) and to ensure those conditions are stable prior to referring a patient for surgical consultation.
Table 3. Coexisting Conditions That Contraindicate Cataract Surgery
|
Patients with conditions that may result in pupillary rigidity or zonular weakness or both, such as pseudoexfoliation syndrome, or have history of ocular trauma should be informed about the higher risk of surgical complications.8,9 It is also helpful to know the patient’s current list of medications, because some potentially increase the risk of surgical complications. For example, Flomax (tamsulosin, Boehringer Ingelheim) has been known to cause intraoperative floppy iris syndrome (IFIS).8
Risk of developing pseudophakic cystoid macular edema increases in patients with diabetes mellitus, recurrent anterior uveitis, epiretinal membrane, vitreomacular traction, retinal vein occlusion or a combination of any of these.10 While these factors are not absolute contraindications, these patients should be counseled regarding possible surgical risks and complications.
Generally, surgical intervention is contraindicated when it will not significantly improve visual function due to the presence of
coexisting ocular disease or if the patient is unfit for surgery due to an underlying medical condition.
Table 3 is a list of conditions that contraindicate surgery.10,11 However, under special circumstances, cataract surgery may be necessary to improve visualization of the posterior segment for treatment of coexisting posterior segment disease, even if only minimal visual acuity improvement is expected.
| Table 4. Onset and Incidences of Potential Postoperative Cataract Complications | |||
| Complications | Postoperative Onset | Incidence | |
| Toxic anterior segment syndrome | 12 hrs to 24 hours | 0.1% to 2% | |
| Anterior uveitis | 24 hrs to 14 days | ~0.20% | |
| Ocular hypertension | 24 hrs to 14 days | 0.3% to 10% | |
| Acute endophthalmitis | 72 hrs to weeks | 0.02% to 0.5% | |
| Pseudophakic cystoid macular edema | one to four months | 3% to 5% | |
| Posterior capsule opacity | Months to years | 20% to 40% | |
The Postoperative Comanagement Protocol
The postoperative follow-up schedule for a typical cataract patient is generally advocated at one day, one week, one month and two months subsequent to the surgical extraction of the cataract.4 Conventionally, the surgeon will see the patient the day after the surgery, and the optometrist assumes postoperative care at the one-week or one-month visit. This may vary depending on the comanagement relationship with the surgeon.
In addition, postoperative medications—such as topical antibiotic, steroids and NSAIDs—are given to control postoperative inflammation and prevent infection. Exact medications and dosage vary by surgeon. Here is a summary of the general postoperative guidelines:2,4
First postoperative visit:
- Occurs 24 to 36 hours after surgery.
- Examination includes: unaided and aided visual acuity (with pinhole); IOP; slit-lamp evaluation; fundus exam with evidence of especially poor vision or retinal disease.
- Fully instruct patients on their postoperative drop regimen (topical antibiotic, steroids and NSAIDs).
- Review with patient the signs and symptoms of possible postoperative complications that may require emergent care.
Second postoperative visit:
- Seven to 14 days after surgery.
- Examination includes: unaided and aided visual acuity (with pinhole); IOP; slit-lamp evaluation; fundus examination with evidence of especially poor vision or retinal disease.
- If eye is quiescent, consider discontinuing antibiotic drops and starting steroid and NSAID taper (a typical taper schedule is decreasing dosage frequency by one less daily drop each week).
- If inflammation is persistent, topical steroid and NSAID use should be increased accordingly. Once inflammation resolves, begin taper.
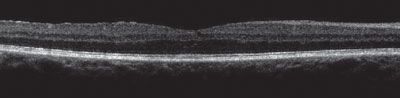 | |
| CME resolving with macular thickness of 300µm after one month of a topical steroid and NSAID. Photo: Aaron Bronner, OD. |
Third postoperative visit:
- Three to four weeks after surgery.
- Examination is analogous to previous visit.
- Consider prescribing spectacles if the eye is quiet and stable.
Fourth postoperative visit:
- Six to eight weeks after surgery.
- Examination is analogous to previous, with a dilated fundus examination.
- Perform a refraction test for a final postoperative prescription, if one has not been done earlier.
- Discuss the benefits and importance of UV protection, especially for patients with IOL implants.
Postoperative Complications
The most imperative part of our postoperative care is to determine whether findings and symptoms are typical or anomalous at the postoperative stage. For example, mild cells in the anterior chamber and/or increased IOP are common a few days following surgery and most often resolve on their own with time. However, we must remain vigilant in distinguishing signs of complications that could be detrimental if not promptly diagnosed and treated. Possible postoperative complications are listed by time of typical occurrence in Table 4.2,3,12-14 Here is a brief overview of some postoperative complications:4,15,16
Acute Endophthalmitis
Causes: Intraocular inflammation due to direct microbial invasion.
| Dropless Cataract Surgery A recent development may make the traditional postoperative routine simpler for both practitioners and patients. So-called ‘dropless’ cataract surgery includes the delivery of formulated medications at the end of the surgery by transzonular technique to provide sustained therapeutic protection against endophthalmitis and postoperative cystoid macular edema. The intention is to improve compliance and convenience, as well as reduce postoperative drop cost.1,2 However, questions of pharmacokinetics compared with that of topical daily drops and concerns of steroid response are still under investigation. Although dropless cataract surgery has yet to make its way to mainstream management, if the surgeon you refer to performs it, be prepared to discuss the risks and benefits with the patient prior to surgery. The patient must be cautioned about the potential initial blur 24 to 48 hours after surgery due to the medication possibly obstructing the visual axis. At any time, if significant inflammation is present postoperatively, additional topical anti-inflammatory medications may be used. Additionally, patients should be made aware that this medication delivery method may not be covered by insurance. The postoperative management and follow-up timeline remains the same. 1. Steinert RF. Cataract Surgery. 3rd ed. Philadelphia: WB Saunders; 2004:589-92. 2. Heier JS, Topping TM, Baumann W, et al. Ketorolac versus prednisolone versus combination therapy in the treatment of acute pseudophakic cystoid macular edema. Ophthalmology. 2000;107:2034-9. |
Signs/symptoms: Decreased vision, pain, photophobia, redness, corneal edema, anterior chamber reaction, hypopyon and vitritis.
Management: Immediate referral back to surgeon. Typical treatment is topical fortified vancomycin and tobramycin Q1H for 24 to 48 hours, topical Pred Forte 1% Q1H and atropine 1% TID-QID. More complicated cases may require intravitreal vancomycin, ceftazidime, dexamethasone or pars plana vitrectomy.
Toxic Anterior Segment Syndrome
Causes: Sterile acute postoperative inflammation due to a noninfectious substance entering the anterior segment and inducing toxic damage to the intraocular tissues.
Signs/symptoms: Decreased vision, redness, “limbus-to-limbus” corneal edema, marked anterior chamber reaction and possible hyphema.
Management: This condition usually responds well to topical steroid (prednisolone acetate 1% every one to two hours). Patients must be followed closely to ensure inflammation does not worsen.
Ocular Hypertension
Causes: Increased IOP induced by steroids, IOL irritation or synechial angle closure.
Management: Treatment depends on the severity of the condition. The elevated IOP can be treated with topical aqueous suppressants as long as such agents are not contraindicated. If there is minimal inflammation, the steroid can be quickly tapered. If there is mild inflammation, consider changing to a mild steroid or topical NSAID.
Pseudophakic Cystoid Macular Edema
Causes: Vessel leakage caused by surgically induced insults, inflammation or both.
Signs/symptoms: Decreased vision, metamorphopsia, scotoma and thickening with or without small intraretinal cysts in the foveal region.
Management: Currently no standardized protocol exists for the prophylaxis and management of pseudophakic CME because of a lack of prospective randomized clinical trials. Therapeutic interventions are based on the proposed pathogenesis of edema, mainly inflammation and vitreous traction.
Posterior Capsule Opacity
Causes: Epithelial cell proliferation and migration, collagen deposition and lens fiber generation.
Signs/symptoms: Decreased vision, opacification of the posterior capsule in the form of fibrosis or pearls.
Management: If functional vision loss is reported, consider Nd:YAG capsulotomy.
Education
Despite the good prognosis, cataract patients may still feel apprehensive when we mention the presence of cataracts and the possible surgical intervention. Therefore, as the patient’s primary eye care provider, we are responsible for educating our patients on the natural course of cataracts and determining the treatment option that best fits the individual patient.
As optometrists we have received extensive training and fought hard for the opportunity to care for our patients from initial cataract diagnosis through their final postoperative exam. Surgeons often prefer that the referring optometrist manage the postoperative care, as it increases the time they have available for surgeries. Patients usually prefer to continue care with their optometrist because of their established relationship and the convenience of being seen at the optometrist’s office, which is usually closer and offers more flexible scheduling.
For us, it can be financially beneficial to see our patients for postop visits, as we are entitled to a portion of the global fees collected by the ophthalmologist. If you are currently referring your cataract patients to a practice that does not allow you to do the postop care, we encourage you to express your interest in it. Explain that our scope of practice and training has significantly expanded over the years, allowing you to deliver this highly specialized care.
Our responsibility is to make sure our patient fully understands the process and feels comfortable from the preoperative discussion to the postoperative recovering process. Working closely with the surgeon will help ensure the best possible outcome.
Dr. Lu is a graduate of Nova Southeastern College of Optometry and recently completed her residency at C.W. Bill Young VA Medical Center in Bay Pines, Florida. She practice in Kansas City, Mo.
Dr. Gruosso is the director of the Low Vision Clinic and the Externship Program at the C.W. Young VA Medical Center.
Dr. Miller is a graduate of the Indiana University School of Optometry. He is the chief of the Optometry Section and resident program supervisor at the C.W. Young VA Medical Center.
Dr. Santos-Nevarez is a graduate of Salus University Pennsylvania College of Optometry. She completed a Primary Care residency at C.W. Young VA Medical Center, where she is an attending optometrist.
1. Congdon N, Vingerling JR, Klein BE, et al. Prevalence of cataract and pseudophakia/aphakia among adults in the United States. Arch Ophthalmol. 2004;122:487-94.2. Murrill CA, Stanfield DL, VanBrocklin MD. Optometric Clinical Practice Guideline: Care of the Adult Patient with Cataract. St.Louis, MO: American Optometric Association; 1995.
3. Davison JA, Chylack LT Jr. Clinical application of the Lens Opacities Classification System III in the performance of phacoemulsification. J Cataract Refract Surg. 2003;138-45.
4. Ehlers JP, Shah CP. The Wills Eye Manual: Office and Emergency Room Diagnosis and Treatment of Eye Disease. Philadelphia: Lippincott Williams & Wilkins; 2008.
5. Takeshita B, Wing V, Gallarini L. Corning CPF filters for the preoperative cataract patient. J Am Optom Assoc. 1988;59:793-7.
6. Lundström M, Goh PP, Henry Y, et al. The changing pattern of cataract surgery indications. Ophthalmology. 2015;122.1:31-8.
7. Lundström M, Barry P, Henry Y, et al. Visual outcome of cataract surgery: study from the European Registry of Quality Outcomes for Cataract and Refractive Surgery. J Cataract Refract Surg. 2013;39:673-9.
8. American Academy of Ophthalmology. Cataract in the Adult Eye. Cataract and Anterior Segment Preferred Practice Pattern (PPP) Panel. Accessed June 2, 2015. www.aao.org/preferred-practice-pattern/cataract-in-adult-eye-ppp--october-2011.
9. Kuchle M, Viestenz A, Martus P, et al. Anterior chamber depth and complications during cataract surgery in eyes with pseudoexfoliation syndrome. Am J Ophthalmol. 2000;129:281-5.
10. Noble B, Hayward M. Contraindications to intraocular lens implantation. In: Percival P, ed. Color Atlas of Lens Implantation. St. Louis: Mosby-Year Book; 1991:147.
11. Berontsky DA, Stark WJ, McCartney DL, et al. Changing indications for intraocular lenses: guidelines (legal and ethical) for cataract surgery. In: Caldwell DR, ed. Cataracts: Transactions of the New Orleans Academy of Ophthalmology. New York: Raven Press; 1988:1-8.
12. Javitt JC, Vitale S, Canner JK, et al. National outcomes of cataract extraction: endophthalmitis following inpatient surgery. Arch Ophthalmol. 1991;109:1085-9.
13. Henderson BA, Kim JY, Ament CS, et al. Clinical pseudophakic cystoid macular edema. Risk factors for development and duration after treatment. J Cataract Refract Surg. 2007;33(9):1550-8.
14. Hellinger WC, Hasan SA, Bacalis LP, et al. Outbreak of toxic anterior segment syndrome following cataract surgery associated with impurities in autoclave steam moisture. Infect Control Hosp Epidemiol. 2006 Mar;27(3):294-8.
15. Steinert RF. Cataract Surgery. 3rd ed. Philadelphia: WB Saunders; 2004:589-92.
16. Heier JS, Topping TM, Baumann W, et al. Ketorolac versus prednisolone versus combination therapy in the treatment of acute pseudophakic cystoid macular edema. Ophthalmology. 2000;107:2034-9.

