 |
|
|
This "early ad
opter" underwent LASIK many
years ago. Now, he has developed
a visually
significant cataract.
How should we
approach
the surgical work-up
?
|
Interestingly, many of refractive surgery’s “early adopters” (i.e., those who had a procedure in the mid 1990s) have already reached age 50 to 60, and we are now beginning to see them return with visually significant cataracts and presbyopia. A sizeable majority of early adopters had some form of laser corneal reshaping procedure––either LASIK or PRK. A history of corneal reshaping poses a unique challenge to optometrists when considering a cataract procedure. For example, intraocular lens (IOL) calculations and corneal refractive measurements may be substantially different from what generally is anticipated in patients who have not undergone laser vision correction.
Despite the inherent challenges in comanaging refractive surgery’s early adopters, it is your responsibility to discuss all the available cataract surgery options with these patients to determine the most suitable way to meet or exceed their visual expectations.
The Patient Education Process
Our patients are always increasing their awareness of current refractive procedures and premium IOL technologies through a variety of sources, including the Internet. Nevertheless, optometrists remain the primary educators when guiding patients through their final assessment and comprehensive surgical plan. No other eye care providers are better positioned for this task than primary care optometrists.As such, practitioners who have worked with patients during a previous laser vision correction process are especially familiar with their anticipated visual expectations following surgery. And because many of these patients expect significant visual improvements with today’s latest innovations, you should make every effort to keep up to date with all current IOL options, including standard, toric and presbyopia-correcting modalities. Be sure to provide a thorough overview of each IOL’s benefits and disadvantages, as well as have a discussion about the desired refractive outcome, before you refer a patient for surgery. Educating patients on every aspect of their future cataract surgery and playing an active role in both their pre- and postoperative care will ensure that their visual needs are best met. If a referral for surgery is made without adequately discussing the preoperative information, including all available treatments and lens options, patients could be unhappy with their postoperative result and might seek the services of a different eye care provider for all future needs.
IOL Calculations and ‘Refractive Surprise’
|
|
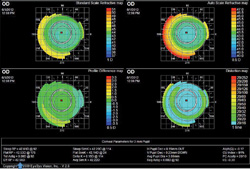
Automated topography is one of the most accurate methods to
determine IOL ca lculations in patients who've previously undergone a corneal re shaping procedure. |
• The historical method relies on the gathering of pre-corneal shaping surgical information, including K values and refractive error, and comparing it to the postoperative data. The difference in refractive error from before and after the corneal reshaping procedure is subtracted from the pre-refractive surgery K values to arrive at the effective Ks needed in the IOL calculation. Ideally, you’d like to know the patient’s post-corneal shaping refractive error prior to cataractogenesis. But, we don’t always have this information on file before cataract development, which increases the potential for error when adjusting the original K values.
• The contact lens method requires you to apply a plano rigid lens of a known base curve onto the surface of the postoperatively reshaped cornea. Then, you must perform an over-refraction, which will allow you to determine the resultant tear lens power. This figure then can be factored into the known contact lens curvature to arrive at the effective K value needed in the IOL calculation.
• Automated topography captures many refractive data points on the anterior corneal surface and determines effective K values through one of the formulas contained in the corneal topography software.
If given a choice between available formulas, I prefer to select the flattest effective K values possible, thereby resulting in an IOL calculation with additional plus power. This approach enhances the likelihood that a patient may experience a residual myopic outcome, rather than a highly undesirable residual hyperopic outcome. Also, because the effective Ks often overestimate the cornea’s true focusing power, I’ll usually target a refractive endpoint of -0.75D to further avoid the potential for a hyperopic result. In my experience, this often yields a spherical equivalent close to plano.Additionally, we use several diagnostic instruments and newer technologies to help with our IOL calculations––including the Lenstar (Haag Streit) and the Pentacam (Oculus). These technologies measure central and peripheral pachymetry, lens thickness, anterior and posterior topography, axial length, anterior chamber depth and white-to-white distances, as well as calculate the effective K values in post-corneal reshaping patients. It is worth noting that aberrometry can be particularly helpful in post-corneal reshaping surgery patients who are interested in premium IOLs. If, for example, the patient exhibits significant higher-order aberrations, such as trefoil or coma, a mulifocal IOL––which yields further contrast loss––would be contraindicated.
Individualized Considerations
• A history of RK or AK. Patients who have undergone an incisional procedure (i.e., radial keratotomy or astigmatic keratotomy) are evaluated and managed in the same manner as those who have had laser vision correction. These patients likely will report persistent diurnal vision changes following cataract surgery if they had similar issues following incisional keratotomy. Additionally, they are more likely to experience persistent glare under dim lighting conditions secondary to incisions entering the scotopic pupil zone.3• Astigmatism. Ideally, you should instruct the surgeon to make the cataract wound incision further away from the limbus (i.e., a mini scleral tunnel incision, rather than a clear corneal incision) to reduce the potential impact on corneal shape in patients with previous incisional keratotomy. Otherwise, limbal relaxing incisions made at the time of cataract surgery or postoperative PRK enhancement could help reduce residual astigmatic error that a standard IOL may not correct.4 Provided there is significant corneal astigmatism, all previous corneal reshaping patients also can be considered candidates for a premium toric IOL.
• Presbyopia. Likewise, presbyopia-correcting IOLs are an option in post-corneal reshaping patients. Again, keep in mind that implantation of multifocal IOLs can exacerbate the severity of higher-order aberrations in some individuals who have undergone corneal reshaping. Patients who are highly disinterested in wearing glasses, express reasonable visual expectations and have otherwise unremarkable internal and ocular surface examinations may be suitable candidates for multifocal IOLs. Careful evaluation, including similar documentation of the corneal topography measurements used in pre-laser vision correction, is required for post-corneal reshaping patients who are deciding the suitability of multifocal IOLs.
As with virgin corneas, macular and ocular surface health also must be ascertained in all patients who are considering presbyopia-correcting IOLs.
Preoperative Management
Successful comanagement truly is the result of continuous communication amongst all involved parties, including the referring optometrist, cataract surgeon and––most importantly––the patient. During the preoperative period, educate the patient about his or her pre-existing ocular conditions and IOL options in an effort to design the optimal individualized plan for the entire cataract surgery experience.Further, during the preoperative work-up, we administer a simple questionnaire to determine each patient’s lifestyle demands and visual expectations. (An electronic version of the questionnaire we use in our office is available here.)
Carefully explaining the intraoperative details and positioning yourself as the individual chiefly responsible for the patient’s postoperative care not only will help solidify his or her trust in you, but also will help foster a mutually respectful relationship between you and the surgeon, ultimately benefitting the overall care of the patient. All patients––regardless of whether they have undergone previous corneal reshaping––who elect premium IOLs implantation should be informed that their very best possible visual outcome may only be attained via fine tuning with spectacles or contact lenses. Always be sure to discuss this consideration in every pre-cataract surgery evaluation––particularly if the patient has high or unrealistic visual demands. Pre-existing ocular surface conditions (i.e., dry eye status) and personality characteristics are among the most important considerations during the IOL selection process in post-refractive cataract surgery candidates. The identification and aggressive treatment of dry eye and significant tear film instability are essential prior to surgical referral. In my experience, topography scans have revealed IOL calculation errors as high as 1.50D in patients with unstable cornal surface health.
Postoperative Management
Following careful preoperative consideration and meticulous intraoperative techniques applied by an expert cataract surgeon, it is your responsibility to address postoperative complications. Patients who do not experience optimal visual results or have unmet expectations will seek your guidance. Reasons for decreased vision following cataract surgery include residual refractive error, exacerbated dry eye disease, posterior capsular opacification (PCO) and cystoid macular edema (CME). Fortunately, you are able to manage many of these conditions postoperatively. Dry eye can be remedied via aggressive treatment with artificial tear supplements, topical anti-inflammatories, punctal occlusion and omega-3 fatty acids to improve the quantity and quality of tears. Posterior capsular opacification is a common etiology for decreased vision following otherwise unremarkable cataract extraction––although it is important to always carefully examine the macula to rule out the possibility of pseudophakic CME. In the absence of CME and the presence of PCO, a YAG capsulotomy may help restore vision. Keep in mind that a YAG procedure should be considered earlier in the postoperative period for patients with multifocal IOL implantations, because these individuals could be more sensitive to decreased contrast. If cystoid macular edema is detected, treat with both topical and periocular corticosteroids as well as non-steroidal anti-inflammatory agents––deferring YAG capsulotomy until the CME has resolved.Enhancements and Exchanges
The potential for refractive surprise must be discussed in all previous corneal reshaping patients. During the preoperative period, be sure to inform them that a subsequent refractive enhancement may be performed if they are unhappy with their uncorrected vision following IOL implantation. Because re-lifting the LASIK flap after one to two years post-op can result in epithelial cell ingrowth, PRK typically is advised in these instances.5Keep in mind, however, that any laser vision enhancement is contingent upon a suitable corneal profile, including sufficient thickness and a healthy ocular surface. We generally give patients six weeks to stabilize post-cataract extraction, but sometimes they require a longer period of adaptation before deciding upon the need for postoperative enhancement. Remember to inform them that residual refractive error may be a blessing in disguise, permitting them to function well with intermediate range tasks such as computer usage. Should the post-cataract surgery outcome be significantly different than planned, an IOL exchange is another enhancement option—but only if the potential benefits of another intraocular procedure outweigh the risks. If desired, an IOL exchange should be done within three months following the initial IOL implantation to reduce the risk of complications. Prior to confirming the IOL power necessary for a fellow cataract eye with previous corneal reshaping, I’ll review the refractive outcome of the first eye and make IOL power adjustments based on the predicted healing response and visual result. Should a patient decide to proceed with a postoperative laser enhancement to the first eye, it is recommended that he or she first undergo cataract implantation in the fellow eye and wait for bilateral stabilization. This affords the patient a longer adaptation period, as well allows him or her to fully weigh the pros and cons of proceeding with an enhancement. Then, if still desired, a laser enhancement can be conveniently performed bilaterally after a minimum of six weeks following the second cataract procedure.
Refractive surgery’s earliest adopters are becoming increasingly eager to learn about their potential cataract surgery options. As we refine our clinical skills in managing these patients, our primary responsibility is to serve as the directors and counselors of their overall care. In particular, this includes the creation of a tailored assessment and surgical plan that best meets the needs of those who’ve previously undergone corneal reshaping procedures.
Dr. Pohl is the clinical director at Pacific Cataract and Laser Institute in Bellevue, Wash. Additionally, he serves as an adjunct assistant professor at the Pacific University College of Optometry.
1. Solomon KD, Fernández de Castro LE, Sandoval HP, et al. LASIK world literature review: quality of life and patient satisfaction. Ophthalmology. 2009 Apr;116(4):691-701.2. Wang L, Hill WE, Koch DD. Evaluation of intraocular lens power prediction methods using the American Society of Cataract and RefractiveSurgeons Post-Keratorefractive Intraocular Lens Power Calculator. J Cataract Refract Surg. 2010 Sep;36(9):1466-73.3. Salamon SA, Hjortdal JO, Ehlers N. Refractive results of radial keratotomy: a ten-year retrospective study. Acta Ophthalmol Scand. 2000 Oct;78(5):566-8.4. Pisella PJ. Post-operative residual astigmatism after cataract surgery: Current surgical methods of treatment. J Fr Ophtalmol. 2012 Mar;35(3):226-8.5. Macsai MS, Fontes BM. Refractive enhancement following presbyopia-correcting intraocular lens implantation. Curr Opin Ophthalmol. 2008 Jan;19(1):18-21.

