It is estimated that there are more than 140 million contact lens wearers worldwide, with approximately 44 million in the United States alone.1 A recent report offers encouraging news that the current contact lens market is healthy, estimated at approximately $7.6 billion globally—$2.5 billion of which is in the United States.1 Despite this healthy trend, one of the major issues related to contact lens wear is dropout, largely due to contact lens discomfort (CLD).
 | |
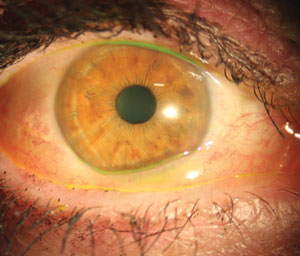
| Punctate keratitis from debris trapped under a gas permeable lens. Photo: Michael J. Lipson, OD. |
This article provides a brief overview of the current understanding of the factors that influence CLD, the impact of contact lens wear on ocular surface sensitivity and management strategies that a practitioner can adopt to minimize contact lens discomfort.
The Basics of CLD
Because CLD has attracted a significant amount of attention from practitioners, researchers and industry, the Tear Film and Ocular Surface Society (TFOS) organized an international panel of experts to delve into the issue. This group defined CLD as “a condition characterized by episodic or persistent adverse ocular sensations related to lens wear, either with or without visual disturbance, resulting from reduced compatibility between the contact lens and the ocular environment, which can lead to decreased wearing time and discontinuation of contact lens wear.”2
The perception of symptoms in CLD is extremely complex and is a result of interactions between several psychophysical channels. In addition to discomfort and dryness, scratchy and watery sensations have been reported 52% and 30% of the time in daily HEMA lens wearers.3 Other symptoms include blurry vision, irritation, light sensitivity, eye soreness, tiredness, itchiness, watering, pain, excessive blinking and burning.
There is a distinctive, five-step pattern to contact lens discomfort progression.2 Step one begins when patients start to struggle with symptoms such as physical awareness and visual disturbance. This is followed by step two, wherein patients adopt certain management strategies such as reducing comfortable wearing time, which leads to step three: reduced total wear time. Step four is temporary discontinuation of contact lens wear, and step five is when patients permanently discontinue lens wear. Given this progression, it is important that eye care providers identify the factors that play a role in the earlier stages of the discomfort in order to adopt appropriate management strategies. Such preliminary measures could help prevent patients from permanently dropping out of contact lens wear.
The terms contact lens discomfort, contact lens-related dryness and contact lens dry eye have been used synonymously in the literature. However, there are differences between these conditions, as outlined by the TFOS report. Contact lens-related dryness and contact lens dry eye both refer to contact lens wearers with pre-existing dry eye, which may or may not be exacerbated by lens wear. Contact lens discomfort occurs only during lens wear, and this can be induced by many factors, broadly classified into three sub-groups: (1) contact lens-related, (2) patient-related and (3) environmental.3
Contact Lens-Related Factors
There are several contact lens-related factors investigators believe play a role in determining comfort during lens wear.4 The only material-related factor shown to correlate with CLD was coefficient of friction.5 A number of other factors have only weak links with CLD, including oxygen transmissibility, wettability, surface modification, modulus and lens dehydration.4
Other physical properties of soft contact lenses that seem to be convincingly related to CLD include lens replacement frequency, design, thickness and edge configuration.4
Many studies have reported that improved comfort is linked with increasing lens replacement frequency.4 When it comes to lens design, thin, tapered edges interact less with the lids than thicker lenses, thereby resulting in improved comfort.6 Lens materials with thicker designs are often less comfortable than thinner ones and result in higher reports of CLD.7 Increased lens movement results in reduced comfort, while lower lens mobility increases perceived comfort.8
High water content is associated with an increase in contact lens discomfort as demonstrated in conventional hydrogel lens materials; however, research has yet to show a similar link with ionicity variations.9,10 No studies examine these factors using silicone hydrogel lens materials. Although deposition of tear film components, including proteins and lipids, did not correlate with subjective symptoms, one study showed that the degree of denaturation of protein had a significant correlation with subjective comfort.11
Another important aspect to consider is the use of lens care products, which are composed of several components including biocides, wetting agents, chelating agents, surfactants and buffering agents. Although reports show the presence of one biocide will improve comfort when compared with the other, in reality, it is not possible to isolate the presence of one specific component and attribute its presence to contact lens comfort.4 Evidence shows that the presence of certain wetting agents in a lens care product could result in reduced CLD, possibly by improving the wettability of lenses and by making the lenses feel moist.4
Practitioners can suggest their patients use lens care products that incorporate wetting agents, which can potentially improve CLD.
Patient-Related Factors
Several non-modifiable and modifiable patient-related factors may affect CLD.
Non-modifiable factors
Several studies indicate that women are more likely to report symptoms of CLD than men.9 Age is another non-modifiable factor; younger wearers report more symptoms compared with elderly wearers, perhaps because patients become more tolerant as they age.12 Other non-modifiable factors known to play a role in CLD include poor tear film quality and quantity and seasonal allergies.9,13 While factors such as ethnicity, blink rate and systemic diseases play a huge role in dry eye disease, little evidence indicates these non-modifiable factors impact CLD.14 However, conditions such as ocular medicamentosa, atopic and autoimmune disease, tear film abnormalities and corneal and conjunctival diseases could affect comfort during contact lens wear.14
 | |
| Inflamed conjunctival tissue prolapsed onto the cornea. Photo: Michael J. Lipson, OD. |
Modifiable factors
Oral contraceptives and over-the counter pain medications have been shown to be associated with symptoms of scratchiness and dryness.9,15 Other factors commonly associated with CLD include diet, alcohol consumption, smoking, cosmetic use and psychology; yet, little evidence supports the supposition that these factors play a role in CLD.14
Environmental Factors
Although it is commonly believed that environmental conditions such as high altitude, air conditioning, pollution, climate and temperature will impact CLD, there is no direct evidence to support this.14
However, any condition with reduced relative humidity, increased air flow (wind) and blink rate-modifying activities (such as computer use or video-gaming) can cause contact lens discomfort.14
Ocular Surface Sensitivity
Different ocular structures perceive various sensory messages, which can be measured using aesthesiometry. The neurons that innervate the cornea respond to different physical and chemical stimuli, and the impulses originating at the peripheral nerves ultimately reach the cortex via the lower brain stem. Among the various sensations that are perceived by the ocular surface is pain, which is evoked by inflammatory and traumatic events, especially in the cornea. Tactile sensations, however, are evoked at the conjunctiva. Other sensations such as dryness, grittiness and fatigue are due to psychophysical channels and complex interactions in the brain.
Contact lenses interact with the ocular surface, including the cornea, conjunctiva and eyelid tissues during lens wear. These structures are densely innervated.15 Because the stimuli to the ocular surface from a contact lens are extremely complex and multifactorial, there is limited evidence for understanding the mechanisms involved in CLD. The various stimuli to the ocular surface during lens wear could include the effects of a lens care product, thermal effect, hyperosmolarity, desiccation, friction, inflammation and mechanical stimulation.
Several studies show that polymethyl methacrylate (PMMA), rigid gas permeables (RGP), orthokeratology and conventional hydrogel contact lens wear are associated with reduced sensitivity.16-18 Researchers speculate that this reduced sensitivity impacts the blinking mechanism and lacrimal glands’ tear secretion, leading to increased tear evaporation and tear secretion, ultimately resulting in increased symptoms of dry eye.15
Recent studies show the use of silicone hydrogels or daily disposables have no impact on corneal sensitivity.17,19 There is limited information on the effect solutions have on the neurobiology of the ocular surface from which to draw any meaningful conclusions. Throughout the past decade, researchers have advanced our understanding of the dynamic nature of pain and various mechanisms involved in perceiving pain, which will help in better understanding CLD.
CLD Management
CLD is multifactorial, and there is no single, straightforward solution to treat this condition. Each case should be considered carefully, and individual assessment is required. Here are steps every doctor should take when seeing a patient with contact lens discomfort:
1. Take a careful history and assess the status of both the patient and the lenses he or she is using.20 This assessment should include, but should not be limited to, determining the patient’s age, sex, current lens type, lens care product, replacement schedule, environmental conditions (especially the occupational environment), onset of symptoms and use of any drops or oral medications.
2. Identify non-contact lens related factors such as systemic and ocular conditions that could contribute to contact lens discomfort. Treating these could significantly reduce your patient’s contact lens discomfort.
3. Identify contact lens- and care system-related factors that may be causing discomfort. These include physical defects on the lens, poor lens fitting or deposition. Fitting with steeper base curves, using larger diameter lenses, alternating the back lens surface shape and using lenses with a thinner center thickness may improve CLD.
Also consider changing the replacement frequency, material or care system. For example, peroxide systems have long been appreciated for their superior cleaning capabilities, leading to better overall patient satisfaction. You can also suggest the use of tear supplements and wetting agents to improve comfort.
Oral azithromycin and a change in diet to include more omega-6 fatty acids, such as evening primrose oil, has also shown to improve contact lens discomfort.20 One study also highlighted that intracanalicular plug occlusion of the upper and lower drainage systems improves symptoms in hydrogel lens wearers who are symptomatic of dry eye.20 Lower punctal occlusion with a silicone plug resulted in increased wearing times in symptomatic wearers of soft lenses.20
Because contact lens discomfort is a complex condition, it is essential for practitioners to understand the myriad patient- and contact lens-related factors that can contribute to the problem. With a firm grasp of the potential issues in play, we can manage each patient’s contact lens concerns in the earliest stages of CLD. Such an approach could potentially improve the long-term prognosis of safe and comfortable contact lens wear.
Drs. Srinivasan and Subbaraman are optometrists at the Centre for Contact Lens Research (CCLR), School of Optometry and Vision Science, at the University of Waterloo, Ontario, Canada.
Disclosure: CCLR has received research support or honoraria from Advanced Vision Research, Alcon, AlgiPharma, Allergan, Ciba Vision, CooperVision, Contamac US, Eleven Biotherapeutics, Essilor, Johnson & Johnson Vision Care, Ocular Dynamics, Oculus, Ocusense, TearScience and Visioneering Technologies.
1. Nichols J. Contact Lenses 2014. Contact Lens Spectrum. 2015 January.2. Nichols KK, Redfern RL, et al. The TFOS International Workshop on Contact Lens Discomfort: report of the definition and classification subcommittee. Invest Ophthalmol Vis Sci. 2013;54:14-9.
3. Nichols JJ, Willcox MD, Bron AJ, et al. The TFOS International Workshop on Contact Lens Discomfort: executive summary. Invest Ophthalmol Vis Sci. 2013;54:7-13.
4. Jones L, Brennan NA, Gonzalez-Meijome J, et al. The TFOS International Workshop on Contact Lens Discomfort: report of the contact lens materials, design, and care subcommittee. Invest Ophthalmol Vis Sci. 2013;54:37-70.
5. Coles C, Brennan N. Coefficient of friction and soft contact lens comfort. Optom Vis Sci. 2012;89:E-abstract: 125603.
6. Maissa C, Guillon M, Garofalo RJ. Contact lens-induced circumlimbal staining in silicone hydrogel contact lenses worn on a daily wear basis. Eye Contact Lens. 2012;38:16-26.
7. Young G, Chalmers RL, Napier L, et al. Characterizing contact lens-related dryness symptoms in a cross-section of UK soft lens wearers. Cont Lens Anterior Eye. 2011;34:64-70.
8. Young G. Evaluation of soft contact lens fitting characteristics. Optom Vis Sci. 1996;73:247-54.
9. Nichols JJ, Sinnott LT. Tear film, contact lens, and patient-related factors associated with contact lens-related dry eye. Invest Ophthalmol Vis Sci. 2006;47:1319-28.
10. Ramamoorthy P, Sinnott LT, Nichols JJ. Treatment, material, care, and patient-related factors in contact lens-related dry eye. Optom Vis Sci. 2008;85:764-72.
11. Subbaraman LN, Glasier M, Srinivasan S, et al. Protein deposition and clinical symptoms in daily wear of etafilcon lenses. Optom Vis Sci. 2012 Oct;89(10):1450-9.
12. Chalmers RL, Hunt C, Hickson-Curran S, Young G. Struggle with hydrogel CL wear increases with age in young adults. Cont Lens Anterior Eye. 2009;32:113-9.
13. Glasson MJ, Stapleton F, Keay L, et al. Differences in clinical parameters and tear film of tolerant and intolerant contact lens wearers. Invest Ophthalmol Vis Sci. 2003;44:5116-24.
14. Dumbleton K, Caffery B, Dogru M, et al. The TFOS International Workshop on Contact Lens Discomfort: report of the subcommittee on epidemiology. Invest Ophthalmol Vis Sci. 2013;54:20-36.
15. Brennan NA, Efron N. Symptomatology of HEMA contact lens wear. Optom Vis Sci. 1989;66:834-8.
16. Millodot M, Henson DB, O’Leary DJ. Measurement of corneal sensitivity and thickness with PMMA and gas-permeable contact lenses. Am J Optom Physiol Opt. 1979;56:628-32.
17. Lum E, Golebiowski B, Gunn R, et al. Corneal sensitivity with contact lenses of different mechanical properties. Optom Vis Sci. 2013;90:954-60.
18. Murphy PJ, Patel S, Marshall J. The effect of long-term, daily contact lens wear on corneal sensitivity. Cornea. 2001;20:264-9.
19. Situ P, Simpson TL, Jones LW, Fonn D. Effects of silicone hydrogel contact lens wear on ocular surface sensitivity to tactile, pneumatic mechanical, and chemical stimulation. Invest Ophthalmol Vis Sci. 2010;51:6111-7.
20. Papas EB, Ciolino JB, Jacobs D, et al. The TFOS International Workshop on Contact Lens Discomfort: report of the management and therapy subcommittee. Invest Ophthalmol Vis Sci. 2013;54:183-203.

