 |
Q: I have a patient with corneal ectasia following LASIK with an acute corneal hydrops. Apparently, he was a big eye rubber! He is extremely bothered by his loss of vision and is quite light sensitive. Should an anterior chamber injection be considered early, or is there no need to rush? Is there any value in injecting retinal gas (C3F8 or SF 6) over air if you are treating a patient with corneal hydrops?
A: It’s best to do it earlier rather than later, and to use gas rather than air.
Corneal hydrops, an uncommon complication seen in patients with keratoconus and other corneal ectatic disorders, occurs when a tear in Descemet’s membrane allows the aqueous humor to enter the stroma, resulting in corneal edema. While painful and visually obstructive, most cases resolve naturally over several months, during which endothelial cells cover the break, restoring Descemet’s membrane.1

|
|
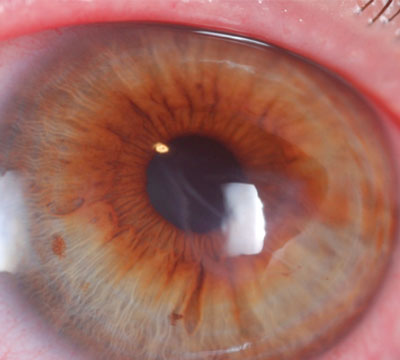
| Fig. 1. Placement of intracameral C3F8 at nonexpansile concentration. Photo: Edward Boshnick, OD |
|
 |
|
| Fig. 2. After the procedure, the hydrops has resolved. Photo: Edward Boshnick, OD |
|
To supplement the natural healing process, consider use of topical corticosteroids to reduce pain and inflammation, as well as glaucoma drugs to lower the IOP and reduce the hydrostatic forces causing the edema, says Eric Donnenfeld, MD, a Long Island ophthalmologist who specializes in laser vision correction. Topical antibiotics can also be prescribed to prevent a secondary infection if there is significant corneal compromise.1 Subsequent surgery may be necessary if corneal edema persists or resultant corneal scarring affects visual clarity.1
An alternative approach to managing corneal hydrops that has become more prevalent in recent years is the use of intracameral air or gas as a means to tamponade the exposure of aqueous to the corneal endothelium.
“Placement of air or gas can be performed at the slit lamp and can occlude the break in Descemet’s membrane, leading to a dramatic reduction in corneal edema and a rapid resolution of the condition,” explains William Trattler, MD, who performs refractive, corneal and cataract eye surgery at the Center for Excellence in Eye Care in Miami. Studies have shown markedly faster improvement compared to more conservative treatments.2-4
Dr. Trattler says gas does have a leg up over air. “The advantage of retinal gas is that it will stay within the anterior chamber for a longer period of time, reducing the chance a second injection is needed.” He cautions there are still associated risks with using either, however. “The main risk is pupillary block, as enough air or gas needs to be placed within the eye to block the entrance of aqueous into the cornea.” Thus, he adds, it is important to use a nonexpansile concentration of gas (figure 1), as expansion can lead to a complete fill of the anterior chamber, resulting in pupillary block. Other steps to reduce the risk of pupillary block include the use of dilating eye drops and placement of an inferior peripheral iridotomy.
Additional risks, says Dr. Trattler, include infection as a result of the needle’s entrance into the anterior chamber. There is also evidence the presence of the gas in the anterior chamber may induce cataracts, notes Dr. Donnenfeld. He recommends patients lie on their back for several days following placement of the gas in the anterior chamber to achieve the best results possible.
1. Association of Optometric Contact Lens Educators. Acute Corneal Hydrops. Available at: www.aocle.org/livingL/hydrops.html. Accessed December 28, 2014.
2. Miyata K, Tsuji H, Tanabe T, et al. Intracameral air injection for acute hydrops in keratoconus. Am J Ophthalmol 2002;133(6):750-752.
3. Panda A, Aggarwal A, Madhavi P, et al. Management of acute corneal hydrops secondary to keratoconus with intracameral injection of sulfur hexachloride (SF6
). Cornea. 2007; 26(9):1067-1069.
4. Basu S, Vaddavalli PK, Ramappa M, et al. Intracameral perfluoropropane gas in the treatment of acute corneal hydrops. Am J Ophthalmol 2011:118(5):934-939.

